颈前路椎间盘切除融合术(anterior cervical discectomy and fusion,ACDF)是治疗颈椎病应用最为广泛的手术方式之一,大量的临床实践证明传统前路融合手术能够取得良好的治疗效果[1]。但也有越来越多的证据表明ACDF可加速邻近节段退变,甚至引发症状[2]。近年来使用逐渐广泛的人工颈椎椎间盘置换则旨在恢复、维持椎间盘切除术后的正常颈椎活动度(range of motion,ROM),进而减少临近节段问题的发生率[3]。本研究前瞻分析Bryan人工椎间盘置换与ACDF治疗单节段颈椎病的疗效,并注重分析二者术后颈椎ROM的变化情况,报道如下。
1 资料与方法 1.1 一般资料2006年8月~2009年2月,本院连续治疗单节段脊髓型或神经根型颈椎病患者94例。纳入标准:①年龄>18岁;②有明显症状的C3~7单节段神经根型或脊髓型颈椎病患者;③经6周的非手术治疗后无效或症状加重。排除标准:①多节段颈椎病变;②颈椎过伸过屈侧位X线片上水平位移>3 mm;③病变椎间隙活动成角>11°;④严重的小关节退变;⑤骨质疏松症代谢性疾病。共59例患者纳入本研究,男39例,女20例;平均年龄45.3岁(32~63岁);其中脊髓型颈椎病36例,神经根型颈椎病18例,混合型(神经根型+脊髓型)颈椎病5例;手术节段:C3/C4 5例,C4/C5 20例,C5/C6 26例,C6/C7 8例。59例患者随机分为Bryan组和ACDF组,其中Bryan组27例,ACDF组32例,对比2组手术时间、术中出血量和住院时间。所有患者随访3~24个月,平均16.2个月。术前及术后6周、3个月、6个月、12个月、24个月均进行各项疗效评价指标评分,并拍摄颈椎正侧位和伸屈位X线片。
1.2 手术方法2组显露和减压方法相同。患者仰卧位,颈部轻微后伸,取右侧颈部横切口显露手术间隙。C形臂X线机透视下确定目标间隙,适当撑开后切除椎体前缘骨赘、椎间盘和后纵韧带。ACDF组彻底切除椎间隙上下软骨终板,随即置入大小合适的椎间融合器,椎体前方钢板螺钉固定。Bryan组则首先将牵引架和双轨导向器固定于椎体前方表面,确定椎间盘中心后用精确打磨器械处理、塑形终板,注意保留骨性终板以防止术后人工椎间盘下沉。试模确定假体大小后置入Bryan人工颈椎椎间盘(美敦力枢法模)。
1.3 术后处理Bryan组患者术后即允许进行颈部肌肉力量及屈伸活动锻炼,日常活动无特殊限制。ACDF组则必须佩带软颈围4~6周。
1.4 临床及影像学评估指标评估项目包括:①颈椎功能障碍指数(neck disability index,NDI)[4];②颈痛及上肢疼痛视觉模拟量表(visual analog scale,VAS)评分[5];③手术节段ROM,在过伸过屈侧位X线片上测量手术节段脊柱功能单位(functional spinal unit,FSU)Cobb角和颈椎整体曲度(C2~7 Cobb角)。
1.5 统计方法应用SPSS 15.0软件进行统计分析。所有数据以x±s的形式显示。对符合正态分布的数据,组内对比进行配对t检验分析,组间对比使用成组t检验分析。P<0.05为差异有统计学意义。
2 结果2组患者术前各项参数差异无统计学意义(P>0.05)。手术时间、手术出血量、住院时间差异均无统计学意义(P>0.05,见表 1)。共48例患者完成2年随访,Bryan组21例,ACDF组27例。2组术后6周、3个月的颈痛VAS评分和颈部NDI差异有统计学意义(P>0.05),其余各随访时间段2组间差异均无统计学意义(P>0.05),但与术前相比差异均有统计学意义 (P<0.01,见表 2)。Bryan组置换节段ROM存在,ACDF组置换间隙ROM基本消失;整个颈椎的屈伸范围Bryan组在各个时间段与术前相比变化不显著,而ACDF组在术后6周、3个月与术前相比差异有统计学意义(P<0.05),6个月逐渐恢复正常(P>0.05,见表 3)。2组患者典型病例影像学资料见图 1,2。
| | 表 1 2组手术相关指标对比 Tab. 1 Operation indices between Bryan group and ACDF group |
| | 表 2 2组临床疗效指标对比 Tab. 2 Cilnical data between Bryan group and ACDF group |
| | 表 3 2组颈椎整体ROM对比 Tab. 3 Cervical ROM between Bryan group and ACDF group |

|
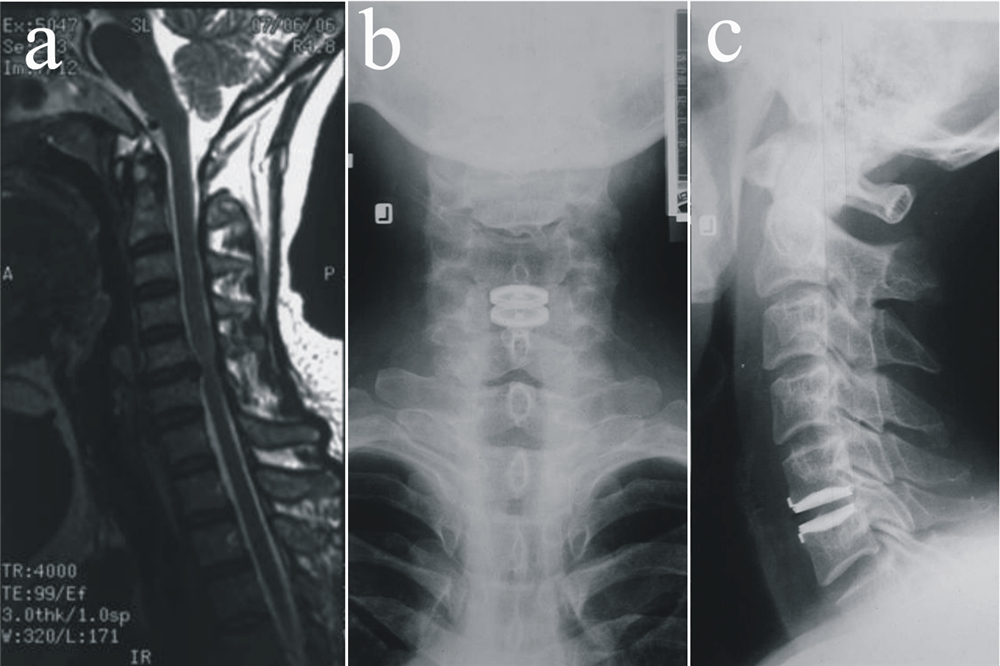
图 1 ACDF组典型病例影像学资料
Fig. 1 Radiologic data of a typical patient in ACDF group
a:术前矢状位MRI显示C5/C6椎间盘突出压迫神经根 b:术前冠状位MRI显示双侧椎间盘退变突出,右侧显著,压迫脊髓侧前方及神经根 c,d:术后2年正侧位X线片显示颈椎整体曲度正常 a: Preoperative MRI shows on sagittal view that herniated C5/C6 intervertebral disc is compressing the nerve root b: Transverse view of preoperative MRI shows significant bilateral disc herniation which compresses the anterolateral spinal cord and the nerve root c,d: Anteroposterior and lateral radiography show that the cervical spine is well alligned 2 years after surgery |
|
图 2 Bryan组典型病例影像学资料
Fig. 2 Radiologic data of a typical patient in Bryan group
a:术前MRI检查显示C5/C6椎间盘突出压迫神经根 b,c: 术后2年正侧位X线片显示颈椎整体序列正常,人工椎间盘假体位置良好 a: Preoperative MRI shows that herniated C5/C6 intervertebral disc is compressing the nerve root b,c: Anteroposterior and lateral roentgenographs show that the cervical spine is well alligned and the disc prosthesis is in good position 2 years after surgery |
ACDF至今仍是治疗颈椎病的“金标准”,也是使用最为广泛的手术方式,但有越来越多的证据表明,融合可使手术节段ROM丧失并导致相邻节段退变加速。Hilibrand等[6]发现,ACDF术后邻近节段退变的患者中2.9%需要再次手术处理。因此,非融合技术成为近年来开发研究的热点,而颈椎人工椎间盘的问世和应用为上述问题的解决带来了很大希望。
单纯从运动学角度考虑,ACDF术后手术节段 的ROM明显减少,整个下颈椎的活动范围是通过 邻近节段的代偿实现的[7]。而从目前国内外的临 床报道上看,Bryan人工颈椎椎间盘置换后手术节 段和整个下颈椎的活动范围接近正常人群[8, 9],生物力学和运动学的研究报告也得到了相似的肯定结果[10, 11]。一项人工颈椎椎间盘置换和ACDF对比的前瞻随机对照多中心研究中显示,术后24个月随访时,人工颈椎椎间盘置换患者手术节段的ROM平均达到了7.95° ,而ACDF组只有0.87°[12]。韩国的一项研究也表明人工颈椎椎间盘置换在保留手术节段ROM方面显著优于ACDF[13]。本研究在手术节段ROM结果上与之前的报道类似,但在下颈椎整体ROM上,尽管短期内Bryan置换组要好于ACDF组,但随着时间的延长,2组均恢复到了术前的ROM水平。
既然Bryan人工椎间盘置换能够保留置换节段的ROM,那就有理由相信它能减少邻近节段新发病的发生率,后者是指手术干预的脊柱节段的头、尾侧节段手术后新出现明确的退变和严重的临床症状而需要手术治疗。Hillibrand等[14]随访21年409例颈椎前路减压融合术患者,邻近节段新发病的年发生率为0.0%~4.8%,在手术后的10年内,大约有近1/4的患者出现邻近节段新发病,其中多数需行再次颈椎手术治疗。而关于ACDF术后颈椎邻近节段退变是因融合所引起的生物力学改变,还是因年龄增加而发生的颈椎退变,仍待进一步研究。
颈椎手术后颈部及上肢不适和疼痛的缓解是疗效评价的主要指标,也是影响患者生活质量的重要因素。而颈臂痛或不适的缓解主要得益于脊髓和神经根的减压以及脊柱稳定的重建[15, 16]。由于Bryan人工椎间盘置换和ACDF的减压操作相同,因此理论上来说二者的术后疗效应相近。本研究对2组患者术后颈痛VAS、臂痛VAS和NDI进行了多个时间点的评估和对比,发现术后3个月内Bryan人工颈椎椎间盘置换术的疗效比ACDF更好,而3个月之后则没有明显差异,2组患者均获得了满意的疗效。究其原因,可能与以下2点有关:首先,ACDF术后通常需要软颈托保护3个月,但目前使用的颈托规格有限,无法定制,其尺寸常无法很好地适合患者,很容易造成颈项部肌肉的疲劳;其次,长期的颈部制动也会造成颈项部肌肉的废用性萎缩从而影响疗效。Sasso等[17]的研究也表明人工颈椎椎间盘置换术后12个月以内尽管差异无统计学意义,颈痛VAS还是低于固定融合组,分析其原因同上。这些都说明Bryan人工颈椎椎间盘置换作为近年来新兴的一种非融合技术,在能够获得与“金标准”ACDF一样稳定的长期疗效的同时,其术后短期患者体验更好。人工颈椎椎间盘置换手术后根据患者的年龄和置换节段的多少,一般建议佩戴颈托1~2周,而国外人工颈椎椎间盘置换手术后一般制动4~7 d,短期的制动一方面可以保护手术部位创伤的顺利恢复,另一方面也避免了长期制动带来的负面影响。
综上,Bryan人工颈椎椎间盘置换能够取得与ACDF相似的临床效果,并且保持了病变节段正常的屈伸活动范围,在严格把握好适应证的前提下值得推广应用,但仍然需要大样本的长期随访资料来最终证实其可以有效减少或避免邻近节段新发病的问题。
| [1] | Chagas H, Domingues F, Aversa A, et al. Cervical spondylotic myelopathy: 10 years of prospective outcome analysis of anterior decompression and fusion[J]. Surg Neurol, 2005, 64 Suppl 1:30-35. |
| [2] | Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion[J]. Spine (Phila Pa 1976), 2002, 27(22):2431-2434. |
| [3] | 王岩, 肖嵩华, 陆宁, 等. 颈人工椎间盘假体置换术的临床应用[J]. 中华外科杂志, 2004, 42(21): 1333-1337. |
| [4] | Aslan E, Karaduman A, Yakut Y, et al. The cultural adaptation, reliability and validity of neck disability index in patients with neck pain: a Turkish version study[J]. Spine (Phila Pa 1976), 2008, 33(11):E362-365. |
| [5] | Joyce CR, Zutshi DW, Hrubes V, et al. Comparison of fixed interval and visual analogue scales for rating chronic pain[J]. Eur J Clin Pharmacol, 1975, 8(6):415-420. |
| [6] | Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis[J]. J Bone Joint Surg Am, 1999, 81(4):519-528. |
| [7] | Anderson PA, Sasso RC, Riew KD. Comparison of adverse events between the Bryan artificial cervical disc and anterior cervical arthrodesis[J]. Spine (Phila Pa 1976), 2008, 33(12):1305-1312. |
| [8] | 王岩, 肖嵩华, 陆宁, 等. 单双节段Bryan颈椎间盘假体置换术后1-8个月临床资料分析[J]. 中国矫形外科杂志, 2005, 13(1):14-17. |
| [9] | 王征, 王岩, 张雪松, 等. 颈椎间盘假体置换术治疗脊髓型颈椎病的近期效果观察[J]. 中国脊柱脊髓杂志, 2006, 16(6):420-423. |
| [10] | Sasso RC, Best NM. Cervical kinematics after fusion and bryan disc arthroplasty[J]. J Spinal Disord Tech, 2008, 21(1):19-22. |
| [11] | 张雪松, 王岩. 颈椎间盘假体的研究进展[J]. 中华外科杂志, 2004, 42(21):1338-1339. |
| [12] | Sasso RC, Best NM, Metcalf NH, et al. Motion analysis of bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial[J]. J Spinal Disord Tech, 2008, 21(6):393-399. |
| [13] | Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases[J]. Eur Spine J, 2009, 18(2):218-231. |
| [14] | Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion?[J]. Spine J, 2004, 4(6 Suppl):190S-194S. |
| [15] | Anderson PA, Sasso RC, Rouleau JP, et al. The Bryan Cervical Disc: wear properties and early clinical results[J]. Spine J, 2004, 4(6 Suppl):303S-309S. |
| [16] | Bertagnoli R, Duggal N, Pickett GE, et al. Cervical total disc replacement, part two: clinical results[J]. Orthop Clin North Am, 2005, 36(3):355-362. |
| [17] | Sasso RC, Smucker JD, Hacker RJ, et al. Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow-up[J]. J Spinal Disord Tech, 2007, 20(7):481-491. |
 2011, Vol. 9
2011, Vol. 9
