强直性脊柱炎(ankylosing spondylitis,AS) 是一种主要累及中轴关节的慢性炎症性疾病,晚期易伴发僵硬固定的胸腰椎后凸畸形,导致站立、行走、平视、呼吸困难等,日常活动明显受限[1, 2, 3, 4]。近年来,腰段、胸腰段经椎弓根截骨(pedicle subtraction osteotomy,PSO)被证实为安全、有效的AS后凸畸形截骨矫形方式,术后患者外观及生活质量明显改善[5, 6, 7, 8, 9]。本研究着重对AS后凸畸形患者PSO前后全脊柱后凸角、矢状面平衡距离、骨盆参数做相关统计分析及研究,探讨其变化趋势及临床意义。
1 资料与方法 1.1 一般资料2004年1月~2010年3月,本院收治38例无脊髓神经症状、体征,双髋活动良好的AS胸腰段后凸畸形患者(手术组)。其中男24例,女14例;平均35岁。24名健康志愿者作为对照组,其中男18名,女6名;平均33岁。
1.2 手术方法行后路经椎弓根单节段(L1 2例,L2 14例,L3 8例)或双节段(T12、L1 1例,T12、L2 3例,T12、L3 2例,L1、L3 8例)楔形闭合截骨矫形椎弓根螺钉内固定术,截骨角度(截骨部位头侧椎体上终板与尾侧椎体下终板之间的Cobb角差值)为26°~85°,平均39°。
1.3 影像学资料自然站立位拍摄全脊柱侧位X线片,测量矫形前后影像学参数:T1上终板与骶骨终板夹角(Cobb T1~S1);骨盆入射角(pelvic incidence,PI);骶骨终板与其中点垂线夹角,骨盆倾斜角(pelvic tilt,PT);髋轴中点与骶骨上终板中心铅垂线的夹角,骶骨倾斜角(sacral slope,SS);骶骨终板与水平 面的夹角(见图 1);C7铅垂线与骶骨后上角水平距离(sagittal vertical axis,SVA);截骨角度(PSO angle),即截骨椎体上下终板夹角变化值(如为双节段截骨,则为2个节段截骨角度之和)。
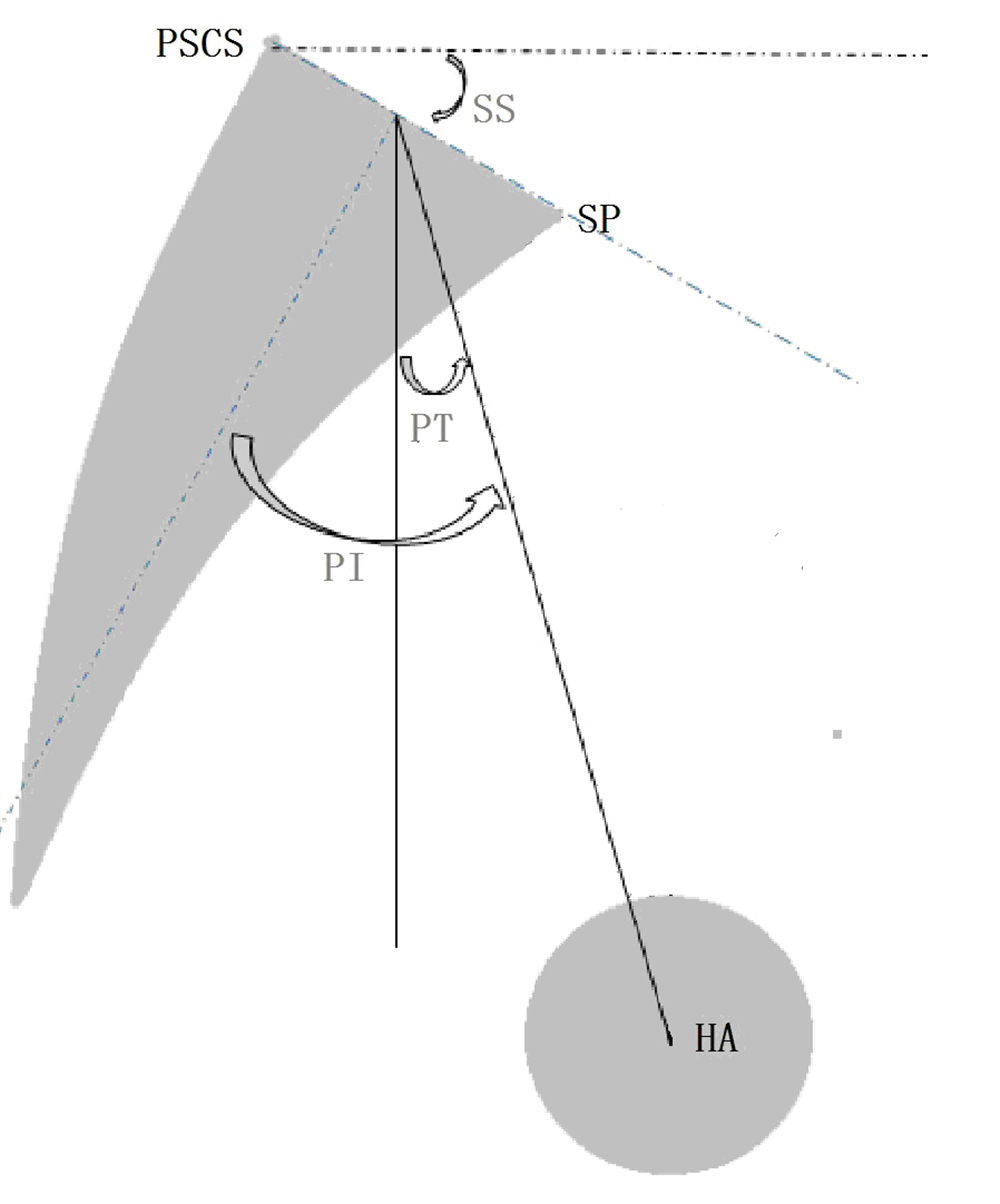
|
图 1 角度示意图
Fig. 1 Schematic diagram of angles
HA: 髋轴中点,双侧股骨头中心连线中点 SP: 骶骨岬,骶骨上终板前下角 PSCS: 骶骨后上角,骶骨上终板后上缘 PI=PT+SS HA: hip axis,midpoint between approximate centers of both femoral heads SP: sacrum promontory PSCS: posterior superior corner of S1 PI=PT+SS |
将矫形前后患者、对照组影像学参数做统计描述及均值t检验。把患者个体差异参数(PI、性别、年龄、体重、患病前身高)作为控制变量,将矫形前后影像学参数做偏相关分析。使用SPSS 16.0 统计软件,以P<0.05 作为检验水准。
2 结果矫形前手术组Cobb T1~S1、SVA、PT较对照组显著增大,SS显著减小;矫形后,Cobb T1~S1、SVA、PT较术前明显减小,SS增大,但与对照组相比差异仍有统计学意义(P<0.05)。手术组PI矫形前后及对照组相比差异无统计学意义(P>0.05,见表 1)。矫形前后PT、SVA与Cobb T1~S1偏相关系数见表 2,矫形前后Cobb T1~S1与PT、SVA分别有明显的偏相关性。截骨角度、节段偏相关分析结果见表 3。截骨节段用其相应腰椎序列表示,双节段截骨用截骨椎体平均值表示(如L3矫正为3,L1、L3矫 正为2),PSO angle 与Cobb T1~S1、PT分别有明显的偏相关性,与SVA无明显的偏相关性。
|
|
表 1 患者矫形前后及对照组结果 Tab. 1 Comparison of parameters before and after treatment |
|
|
表 2 矫形前后影像学参数偏相关分析 Tab. 2 Preoperative and postoperative coefficients of partial correlation |
|
|
表 3 截骨角度、节段偏相关分析 Tab. 3 Partial correlation analysis of PSO angle and level |
从侧面观察直立的人体,头部通过颈椎连接至 躯干,躯干与骨盆相接,骨盆再经过髋关节连接下 肢,相邻的解剖学组件之间密切关联并相互平衡,以能量消耗最小的状态来维持相对稳定的姿势[10, 11, 12, 13, 14]。AS后凸畸形患者腰椎前弯减小,胸椎后弯增大,脊柱整体后凸加重,向前倾斜,矢状面失平衡。与此同时,后凸躯干重心前置,为代偿矢状面失平衡、恢复躯干重心与髋轴的相对位置,机体后旋骨盆。一般情况下,患者后凸越严重,其矢状面失平衡越严重,而相应的骨盆后旋代偿程度越重[7](见图 2)。矫形后,患者脊柱整体后凸变小,躯干倾斜程度减轻,而且由于躯干重心的相对后移,患者代偿性后旋骨盆程度减轻,但与健康人群相比仍有差异。患者脊柱骨盆序列部分改善的研究结果,一方面肯定了PSO治疗AS后凸畸形的有效性,另一方面指出了矫形的不充分性,也就是说对于多数患者的截骨角度偏小[7]。作为骨盆形态学参数的PI[7, 15],矫形前与矫形后及对照组相比,差异无统计学意义。
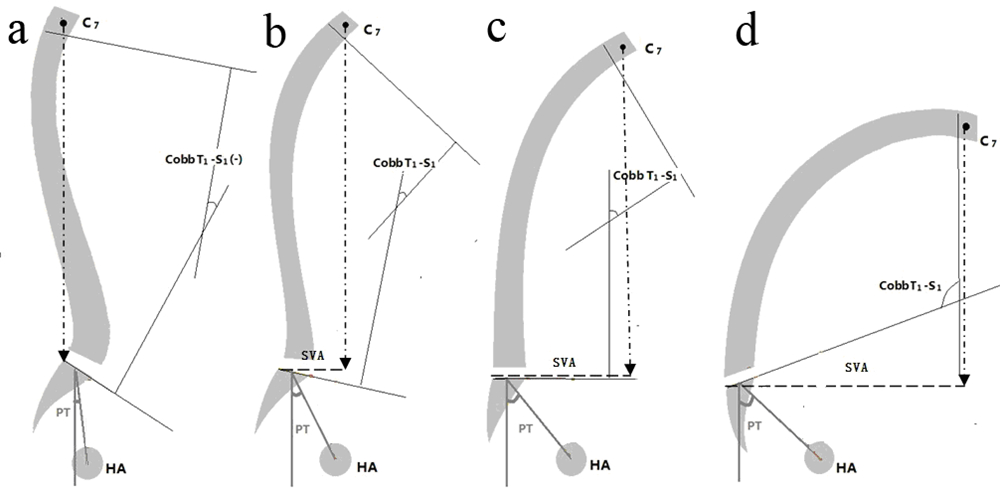
|
图 2 AS后凸畸形矢状面失衡的代偿机制示意图
Fig. 2 Schematic diagram of compensatory mechanism
a: 正常人自然站立状体下,C7铅垂线恰好落在骶骨后上角 b-d: AS患者随着后凸程度发展,CobbT1~S1逐减增大; PT逐渐增大,SS逐渐减小;SVA逐渐增大 a: In healthy adult,C7 falls on posterior superior corner of S1 b-d: AS patients gradually lose its LL and get a larger TK,Cobb T1-S1 increase. Then a backward pelvis appears for balance,leading to increasing PT and SVA. At the same time,SS decreases,and even becames negative |
Lafage等[10]研究发现,截骨矫形对于PT纠正明显大于SVA。本研究结果同样显示截骨角度与PT变化有明显的偏相关性,但未能证明截骨角度与SVA的偏相关系数具有统计学意义。由此可见,人体自身代偿机制优先恢复骨盆的中立状态而非改善矢状面平衡距离;或者说,对于AS患者,PT才是反应人体代偿机制的重要组成部分,而SVA只是一个代偿后的结果[13]。按照几何及力学原理,矫形节段越靠近骨盆,对重心的后移意义越大,但由于样本量有限,本研究未能证明截骨节段对于矫形效果的影响。
3.3 骨盆后旋对活动能力的影响矫形前,机体通过伸髋、屈膝,代偿性后旋骨盆 来维持直立姿势的平衡状态,但此代偿机制依赖于 伸髋、屈膝肌群的持续性收缩,所以同样会带来两大肌群的疲劳性疼痛,最终导致行走、站立困难。一般来说,AS脊柱后凸越严重,躯干重心越是远离髋轴,所需的骨盆代偿性后旋越明显(PT越大,SS越小),而其直立活动能力越差[11, 14]。合理的截骨矫形可使患者脊柱序列改善,躯干重心后移,机体不再需要后旋骨盆的代偿机制来维持直立姿势的平衡状态。所以,合理的矫形术后患者骨盆位置性参数(PT、SS)恢复正常。在此状态下,患者伸髋、屈膝肌群处于松弛状态,为行走、站立活动做好良好的运动储备,患者直立活动能力明显改善[5, 6, 11, 14]。因此,确保术后骨盆中立位(PT、SS恢复至正常值范围)比矫正矢状面平衡距离(SVA恢复至正常值范围)更有意义。
| [1] | Stafford L, Youssef PP. Spondyloarthropathies: an overview[J]. ActaIntern Med J, 2002, 32(1-2):40-46. |
| [2] | Kim KT, Suk KS, Cho YJ, et al. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity[J]. Spine (Phila Pa 1976), 2002, 27(6):612-618. |
| [3] | Van Royen BJ, De Gast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment[J]. Ann Rheum Dis, 1999, 58(7):399-406. |
| [4] | Suk KS, Kim KT, Lee SH, et al. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients[J]. Spine (Phila Pa 1976), 2003, 28(17):2001-2005. |
| [5] | Van Royen BJ, De Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis[J]. Eur Spine J, 2000, 9(6):492-498. |
| [6] | van Royen BJ, Scheerder FJ, Jansen E, et al. ASKyphoplan: a program for deformity planning in ankylosing spondylitis[J]. Eur Spine J, 2007, 16(9):1445-1449. |
| [7] | Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy[J]. Eur Spine J, 2010, 19(1):65-70. |
| [8] | Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance[J]. J Bone Joint Surg Am, 2003, 85-A(3):454-463. |
| [9] | 王岩, 毛克亚, 张永刚, 等. 双椎体截骨术矫正重度强直性脊柱炎后凸畸形[J]. 中国脊柱脊髓杂志, 2009, 19(2):108-112. |
| [10] | Lafage V, Schwab F, Vira S, et al. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction?[J]. J Neurosurg Spine, 2011, 14(2):184-191. |
| [11] | Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity[J]. Spine (Phila Pa 1976), 2009, 34(17): E599-606. |
| [12] | Legaye J, Duval-Beaupere G. Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations[J]. Int Orthop, 2008, 32(6):809-816. |
| [13] | Roussouly P, Gollogly S, Noseda O, et al. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers[J]. Spine (Phila Pa 1976), 2006, 31(11): E320-325. |
| [14] | Chang KW, Leng X, Zhao W, et al. Quality control of reconstructed sagittal balance for sagittal imbalance[J]. Spine (Phila Pa 1976), 2011, 36(3): E186-197. |
| [15] | Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves[J]. Eur Spine J, 1998, 7(2):99-103. |
 2012, Vol. 10
2012, Vol. 10


