腰椎椎间盘突出症是脊柱外科常见病和多发病,是引起腰腿疼痛最常见的原因之一,许多患者需要手术治疗。椎板开窗髓核摘除术(fenestration laminectomy,FL)是治疗腰椎椎间盘突出症的经典术式,该方法在直视下去除病变髓核组织,能对受压的神经结构直接减压,效果较为肯定[1]。随着微创脊柱外科技术不断革新,经皮椎间孔镜椎间盘切除 术(percutaneous transforaminal endoscopic discectomy,PTED) 应运而生,实现了真正意义上的微创,且能对病变部位进行定位治疗[2]。
手术节段椎间隙变窄是腰椎椎间盘突出症术后常见并发症,并可能继发一系列改变,如纤维环、后方韧带、关节囊松弛等[3]。而这些因手术产生的变化可能对腰椎的运动功能、 载荷传导等产生影响,亦可能会导致双侧小关节不对称,引起异常增生,最终影响手术的中远期效果。本院收治单节段腰椎椎间盘突出症患者82例,比较分析PTED与FL 2种不同术式对脊柱运动单位的影响。现报告如下。
1 资料与方法 1.1 一般资料
2008年3月~2012年3月,本院对91例符合标准的单节段腰椎椎间盘突出症患者行手术治疗,全部患者符合以下纳入标准:①腰痛伴/不伴一侧下肢放射痛,经非手术治疗3个月无效或治疗后仍反复发作,疼痛程度较重;②影像学检查明确诊断为单节段腰椎椎间盘突出,伴/不伴同侧侧隐窝狭窄或椎管狭窄;③未合并腰椎不稳、滑脱等;④无神经、内分泌、代谢性疾病及心、肺、肝、肾等疾病,近期无急、慢性炎症活动;⑤无其他手术禁忌证。共82例获得了2年随访。PTED组48例,其中男27例,女21例,平均36.2岁(16~67岁),平均病程26.3个月(9~51个月),L4/L5 31例,L5/S1 17例;FL组34例,其中男21例,女13例,平均40.2岁(23~63岁),平均病程28.3个月(11~54个月),L4/L5 22例,L5/S1 12例。
1.2 手术方法PTED组所有患者采用静脉泵盐酸右美托咪啶并1%利多卡因局部浸润麻醉,均采用经椎间孔镜下脊柱内固定系统 (transforaminal endoscopic spine system,TESSYS)[4],所用器械为德国Jomax公司生产的椎间孔镜操作系统;FL组所有患者采用全麻方法,后正中入路,最大程度地保留脊柱的骨性和软组织结构。
1.3 术后处理PTED组手术次日腰围保护下可进行简单活动;FL组术后伤口放置引流片,24 h内拔除,术后3 d行X线检查后可佩戴护具下床活动。所有患者术后1周出院,术后2年进行复查随访。
1.4 检测项目椎间隙高度(intervertebral space height,ISH)以侧位X线片手术节段间隙前、后缘高度的平均值表示[5];椎间孔高度(foraminal height,FH)以侧位X线片椎间孔上下缘最凹处2点之间的距离表示[5];手术节段活动度(range of motion,ROM)以动力位X线片前屈和后伸时上位椎体下终板与下位椎体上终板延长线的交角之差表示[6];关节突关节间隙差(difference of interfacet distance,DID)以CT上手术节段椎间盘中线层面的上下关节突关节面中点之间的距离差表示[7];小关节角度差(difference of facet joint angle,DFJA)以椎间盘正中矢状面与棘突基底部连线,小关节上关节面前内侧缘与后侧缘连线,2条直线与中线夹角的差值表示[8]。
1.5 统计学分析使用SPSS17.0软件对2组患者术前、术后2年手术节段ISH、FH、ROM、DID以及DFJA等定量资料的组间比较采用成组设计t检验;定性资料以相对数表示,组间比较采用χ2检验(Fisher 确切概率法),检验水准为α=0.05。
2 结 果
PTED组和FL组术前、术后2年的影像学测量结果见表 1。
|
|
表 1 2组患者术后影像学检查结果 Tab. 1 Postoperative radiographic data of 2 groups |
2组术后2年ISH和FH与术前相比均降低,差异有统计学意义(P<0.05);PTED组的丢失量均小于FL组,差异有统计学意义(P<0.01)。2组术后2年手术节段ROM与术前相比均增加,差异有统计学意义(P<0.05);FL组ROM增加大于PTED组,差异有统计学意义(P<0.01)。PTED组术后2年DID和DFJA较术前增加,差异有统计学意义(P<0.05);FL组则较术前降低,差异有统计学意义(P<0.05);2组间比较,差异有统计学意义(P<0.01)。典型病例影像学资料见图 1,2。
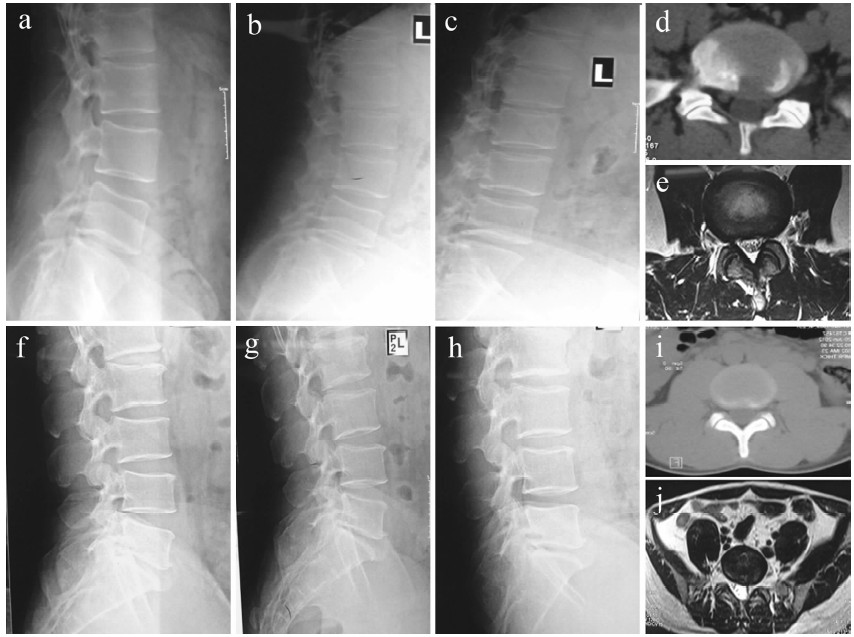 |
a:术前侧位X线片示L5/S1 ISH b,c:术前动力位X线片示腰椎ROM d:术前CT示DID e:术前MRI示DFJA f:术后2年侧位X线片示L5/S1 ISH降低 g,h:术后2年动力位X线片示腰椎 ROM增加 i:术后2年CT示DID增加 j:术后2年MRI示DFJA增加
a:Preoperative lateral roentgenograph shows ISH of L5/S1 b,c:Preoperative extension and flexsion roentgenographs show ROM of L5/S1 d:Preoperative transverse CT shows DID of L5/S1 e:Preoperative transverse MRI shows DFJA of L5/S1 f:Lateral roentgenograph at 2-year follow-up shows ISH of L5/S1 degraded g,h:Extension and flexsion roentgenographs at 2-year follow-up show ROM of L5/S1 increased i,j:Transverse CT at 2-year follow-up show DID of L5/S1 increased j:Transverse MRI at 2-year follow-up show DFJA of L5/S1 increased 图 1 PTED组典型病例影像学资料(L5/S1) Fig. 1 Radiologic data of typical case in PTED group(L5/S1) |
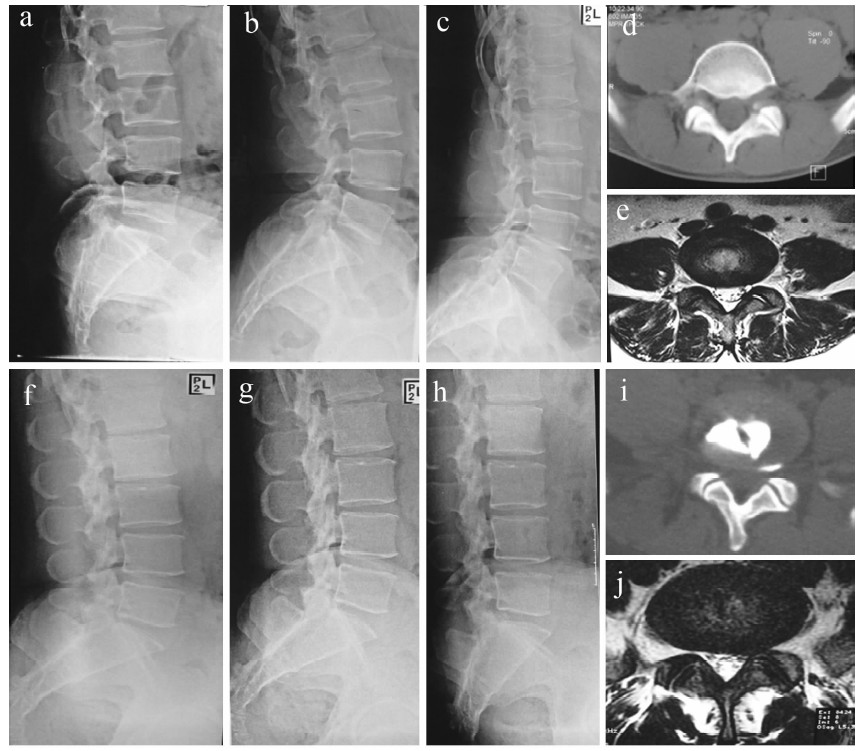 |
a:术前侧位X线片示L4/L5 ISH b,c:术前动力位X线片示腰椎ROM d:术前CT示DID e:术前MRI示DFJA f:术后2年侧位X线片示L4/L5 ISH降低 g,h:术后2年动力位X线片示腰椎ROM增加 i:术后2年CT示DID降低 j:术后2年MRI示DFJA降低
a:Preoperative lateral roentgenograph shows ISH of L4/L5 b,c:Preoperative extension and flexsion roentgenographs show ROM of L4/L5 d:Preoperative transverse CT shows DID of L4/L5 e:Preoperative transverse MRI shows DFJA of L4/L5 f:Lateral roentgenograph at 2-year follow-up shows ISH of L4/L5 degraded g,h:Extension and flexsion roentgenographs at 2-year follow-up show ROM of L4/L5 increased i,j:Transverse CT at 2-year follow-up show DID of L4/L5 degraded j:Transverse MRI at 2-year follow-up show DFJA of L4/L5 degraded 图 2 FL组典型病例影像学资料(L4/L5) Fig. 2 Radiologic data of typical case iin FL group(L4/L5) |
手术治疗腰椎椎间盘突出症至今已有70余年历史。手术切除可能导致椎间盘容积及所维持的高度丧失,同时也可能使得相邻上下椎体所形成的一体结构遭到破坏,产生多种中远期并发症。大量病例的长期随访研究证明了FL是治疗椎间盘突出的经典术式[9],但其创伤相对较大,术中可能需要去除部分椎板和关节突关节,因此可能导致术后远期稳定性丧失、继发椎间孔狭窄等并发症。另一方面,术后因缺乏内固定物导致的下床活动时间延迟也是缺点之一[10]。基于上述原因,微创脊柱外科技术逐渐兴起,PTED是目前微创治疗腰椎椎间盘突出手术方法中的重要分支,采用脊柱后外侧肌间隙入路,通过特殊器械建立手术通道直达病变部位,然后将突出的椎间盘组织去除,对未突出的髓核组织通常不做大部清理,因而局部组织损伤微小,可以保持腰椎自身解剖结构和生物力学的稳定性[11]。
以往对腰椎椎间盘突出术后的研究主要集中于椎间盘本身的变化上,对因椎间盘切除继发的后方小关节退变、手术节段运动变化情况等方面的报道较少,且采用不同术式行椎间盘切除对脊柱运动单位影响的相关报道结果也尚存争议。有研究表明,单节段椎间盘切除对腰椎的稳定性影响较小,仅在腰部屈曲活动达到一定程度时出现手术节段ROM增加的现象[12]。但是也有相关报道认为髓核摘除后对脊柱功能并无不良影响[13]。因此,本研究设计了上述实验,将PTED与FL对手术节段的影响进行了对比评估分析。
腰椎椎间盘切除后相应节段活动的限制因素减弱,髓核摘除量越大则韧带组织越松弛。椎间盘内的髓核组织为胶冻状半液态物质,自身具有一定流动性,髓核摘除术后椎间盘容量会随时间变化进一步退变吸收[14]。FL在直视下咬除突出椎间盘组织,为了避免术后复发,术中尽量将病变节段内的髓核组织进行清理;而PTED通过特殊器械建立 手术通道达到病变部位,然后将突出的椎间盘组织去除,对未突出的髓核组织通常不做彻底清理。上述原因可能导致了FL组ISH和FH丢失量及手术节段ROM增加量大于PTED组。椎间盘是维持腰椎稳定的重要因素,髓核摘除使得椎间盘与上下椎体所形成的一体结构受损,病变间隙高度下降,前后纵韧带松弛,小关节突内聚、增加,进而影响腰椎稳定性。一般认为DID应≥2 mm[15]。FL组DID和DFJA较术前减小,而且部分患者DID<2 mm,这可能与FL组髓核清除更加彻底,上位椎体小关节整体下移幅度更大,使得两侧小关节对合相对于术前贴合更紧密有关。
FL和PTED对脊柱运动单位的影响不同,因此应严格把握2种术式的适应证。术前应精确定位突出髓核的位置和性质,以及椎间孔骨质增生的情况,进行全面的影像学检查,CT和MRI是精确定位髓核大小、位置和性质的重要手段。对于合并腰椎不稳的患者,更应仔细分析各影像学指标,确定最佳手术方案。
综上所述,本研究认为对于单节段腰椎椎间盘突出,FL和PTED都是有效、可靠的治疗方法,PTED技术在ISH、FH和手术节段ROM的保留方面较FL技术更好;DID和DFJA方面,FL技术较PTED技术的表现更为优秀。因此本研究为腰椎椎间盘突出症患者治疗方式的选择和预防中远期并发症提供一定依据,对降低手术并发症、减少再手术和预防脊柱退变等具有临床意义。但是,本研究还存在以下不足:①本研究并非前瞻性对照研究,单节段椎间盘突出的病例数相对较少,将来需进行大样本前瞻性研究;②随访时间较短,尚无远期随访结果,不足以观察小关节炎等方面的变化;③对于多节段椎间盘突出本研究未给出相关结论。以上不足还需要将来进一步研究。
| [1] | Wei MG, He Y, Wang BS, et al.Mini-incision posterior laminectomy by fenestration in the treatment of huge lumbar disc herniation[J].Zhongguo Gu Shang, 2010, 23(6):456-458. |
| [2] | Lew SM, Mehalic TF, Fagone KL.Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations[J].J Neurosurg,2001,94(2 Suppl):216-220. |
| [3] | Choi G, Kang HY, Modi HN, et al. Risk of developing seizure after percutaneous endoscopic lumbar discectomy[J].J Spinal Disord Tech, 2011, 24(2):83-92. |
| [4] | Hoogland T, Schubert M, Miklitz B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain:a prospective randomized study in 280 consecutive cases[J].Spine (Phila Pa 1976), 2006, 31(24):E890-897. |
| [5] | Lee SH, Chung SE, Ahn Y, et al.Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy:a matched cohort analysis[J].Mt Sinai J Med, 2006, 73(5):795-801. |
| [6] | Park H, Zhang HY, Cho BY, et al.Change of lumbar motion after multi-level posterior dynamic stabilization with bioflex system :1 year follow up[J].J Korean Neurosurg Soc, 2009, 46(4):285-291. |
| [7] | Eubanks JD, Toy JO, Messerschmitt P, et al.Anatomic variance of interfacet distance and its relationship to facet arthrosis and disk degeneration in the lumbar spine[J].Orthopedics, 2009, 32(12):893. |
| [8] | Celik SE, Celik S, Kara A, et al.Lumbar facet joint angle and its importance on joint violation in lumbar microdiscectomy[J].Neurosurgery, 2008, 62(1):168-172. |
| [9] | CCook JR Jr. Decompressive procedures. Indications and techniques[J].Vet Clin North Am Small Anim Pract, 1992, 22(4):917-921. |
| [10] | Orpen NM, Corner JA, Shetty RR, et al.Micro-decompression for lumbar spinal stenosis:the early outcome using a modified surgical technique[J].J Bone Joint Surg Br, 2010, 92(4):550-554. |
| [11] | Choi G, Lee SH, Lokhande P, et al.Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope[J].Spine (Phila Pa 1976), 2008, 33(15):E508-515. |
| [12] | 于滨生,刘少喻,李佛保.脊柱稳定重建的解剖及生物力学特点[J].脊柱外科杂志,2005,3(1):40-42. |
| [13] | Mak AS, Jones BL. Separation and characterisation of chymotryptic peptides from alpha-and beta-purothionins of wheat[J].J Sci Food Agric, 1976, 27(3):205-213. |
| [14] | Yan DL, Pei FX, Li J, et al.Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis[J].Eur Spine J, 2008, 17(10):1311-1316. |
| [15] | Chung SB, Lee S, Kim H, et al.Significance of interfacet distance, facet joint orientation, and lumbar lordosis in spondylolysis[J].Clin Anat, 2012, 25(3):391-397. |
 2015, Vol.13
2015, Vol.13 


