20世纪以来,经Wiltse肌间隙入路经椎间孔腰椎椎间融合术(TLIF)越来越多地应用于临床,相较于传统后正中入路,该入路保留了脊柱后方复合体结构,创伤小,出血少,产生更少的术后疼痛,术后恢复快,有效缩短了住院时间[1-2]。然而,随着大量临床研究报道,其缺点也备受脊柱外科医生关注,如融合术后不能早期活动,需3~4个月支具外固定;术后假关节的形成[3];内固定器械的失败和融合器的移位[4];脊柱固定节段活动度(ROM)的丧失和邻近节段退变(ASD)的加剧[5-6]。Dynesys内固定是由Stoll等[7]对Graf固定系统改良而成的新的椎弓根后路动态固定系统,即脊柱非融合技术,通过尽量保留脊柱固定节段的正常运动,理论上能够减轻ASD,在一定程度上减少了融合手术的不良影响[8]。近年来,经Wiltse入路Dynesys内固定术治疗腰椎退行性疾病越来越多地应用于临床并取得了良好的临床疗效[9],但是在老年腰椎椎管狭窄中的实际应用还较少。鉴于上述情况,本研究对2013年1月—2015年1月本院采用Wiltse入路Dynesys内固定及Wiltse入路TLIF治疗的35例老年单节段腰椎椎管狭窄症患者的临床资料进行分析,现报告如下。
1 临床资料 1.1 一般资料回顾性分析2013年1月—2015年1月本院收治的35例老年单节段腰椎椎管狭窄患者的临床资料,其中采用Wiltse入路Dynesys内固定术(Dynesys组)15例,Wiltse入路TLIF(TLIF组)20例。所有老年患者均有相应的临床症状,如腰腿痛、下肢麻木、下肢肌力减退及典型的腰源性间歇性跛行等,术前均经腰椎正侧位及过伸过屈位X线、CT、MRI检查,影像学诊断为腰椎椎管狭窄,经3个月以上非手术治疗无效,手术指征明确,需行腰椎后路减压内固定治疗。
1.2 纳入标准及排除标准纳入标准:①年龄60~75岁;②单节段腰椎椎管狭窄伴/不伴Ⅰ度腰椎滑脱;③腰椎椎管狭窄引起一侧或双侧下肢症状;④术前Oswestry功能障碍指数(ODI)[10] > 30%;⑤下肢症状疼痛视觉模拟量表(VAS)评分[11] > 4.0分;⑥经严格非手术治疗超过3个月仍无效。
排除标准:①既往接受腰椎融合术者;②伴有脊柱肿瘤、感染、骨折;③严重骨质疏松患者,T值 > -2.5并伴有≥1个椎体的脆性骨折;④肥胖,体质量指数 > 40%;⑤全身性疾病和/或接受免疫抑制药物治疗[12-13]。
1.3 手术方法对所有患者均行全身麻醉,取俯卧位,腹部悬空以避免腹腔受压而导致术中出血过多,C形臂X线机透视下确定手术节段并做标记,常规碘酊消毒铺巾后贴保护膜。
Dynesys组(Zimmer Spine,USA):取后正中线旁开3~4 cm做手术切口,且选择患者主要症状侧。切开皮肤及腰背筋膜,暴露多裂肌及最长肌间隙,显露关节突及横突结合部,并拧入合适的螺钉(螺钉长度取决于患者椎体尺寸,尽可能选取最长最粗的螺钉),螺钉头中心点与骨面高度应 < 10 mm,置入过程必须保证小关节完好,病变间隙上下椎弓根各置入一枚螺钉。同法于对侧切开置钉。选择症状明显或影像学改变明显的一侧,于椎板间隙的部分行椎板切除(单侧入路双侧减压),在神经监护及光源和视野良好的基础上,保护关节突,直视下切除同侧关节突关节、侧隐窝、棘突基底,对侧关节突关节及侧隐窝等处增生的骨赘及黄韧带,扩大中央椎管及两侧侧隐窝,术中保留棘突、棘间韧带、棘上韧带、黄韧带及大部分椎板,显露硬膜囊及神经根管,用神经剥离子保护好行走根和出口根,摘除突出的椎间盘。在保持脊柱前凸的基础上,适度撑开两椎弓根螺钉,测量其间距,截取长度合适的间隔器并穿过连接器,将连接器穿过第二枚螺钉头,拉紧连接器以使间隔器完全到位。在对侧实施同样操作。最后两侧收紧并锁紧螺塞。于两侧各放置一根引流管,用盐水冲洗后逐层缝合切口。
TLIF组(Zimmer Spine,USA):切口的具体操作同Dynesys组。切开置钉后,选择症状明显或影像学改变明显的一侧上下关节突予以切除,显露椎间孔,用椎板咬骨钳进一步完成减压,具体减压操作同Dynesys组。用刮刀刮除软组织和软骨终板,保留终板下骨。取术中减压的骨质(或适量自体髂骨),于椎间隙置入大小合适的肾形椎间融合器一枚及自体骨。C形臂X线机透视满意后选取合适的钛棒进行双侧加压固定。取足量自体髂骨,仔细处理成小骨块后填充于准备好的骨床内,完成270°或360°植骨融合。于两侧各放置一根引流管,用盐水冲洗后逐层缝合切口。
1.4 疗效评价记录两组患者围手术期指标(手术时间、术中出血量及术后引流量)。术后1个月、2个月、3个月、6个月、1年及随后每年到门诊复查,由脊柱外科医生记录术前及术后各次随访时的VAS评分、ODI。门诊复查时均在放射科医师指导下摄取标准的腰椎正侧位及功能位X线片,每张X线片均测量2次,由本研究组2名脊柱外科医师分别独立测量,取2次结果平均值。腰椎ROM=过伸位角度-过屈位角度。
1.5 统计学处理应用SPSS 17.0软件对数据进行统计学分析。计量资料以x±s表示,组间比较应用两独立样本t检验。计数资料组间比较采用χ2检验。以P < 0.05为差异有统计学意义。
2 结果两组患者性别、年龄、狭窄节段的差异无统计学意义(P > 0.05,表 1)。所有患者均获得随访,随访时间为12~18个月,平均16个月。随访期间两组患者均无感染、内固定松动等并发症发生,TLIF组植骨均融合。Dynesys组手术时间、术中出血量、术后引流量均优于TLIF组,组间差异有统计学意义(P < 0.05,表 1)。
|
|
表 1 一般资料 Table 1 General data |
两组间术前腰痛VAS评分、腿痛VAS评分及ODI差异均无统计学意义(P > 0.05,表 2)。术后5 d ODI及腰痛VAS评分Dynesys组优于TLIF组,组间差异有统计学意义(P < 0.05,表 2)。术后5 d腿痛VAS评分两组间差异无统计学意义(P > 0.05,表 2)。末次随访时两组患者腰痛和腿痛VAS评分及ODI均较术前明显改善,差异有统计学意义(P < 0.05,表 2);但两组间比较,差异无统计学意义(P > 0.05,表 2)。
|
|
表 2 各时间VAS评分及ODI Table 2 VAS scores and ODI at each time point |
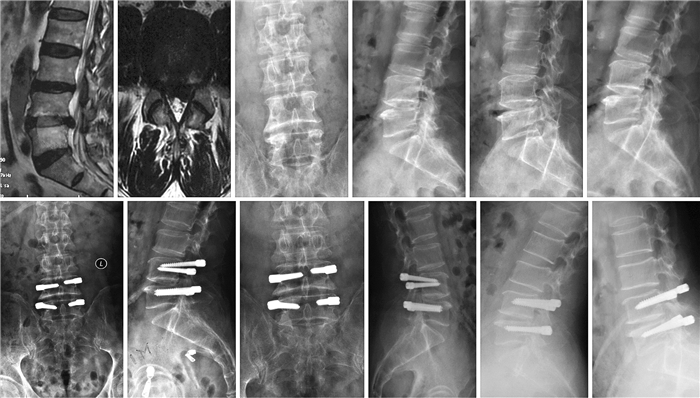
两组术前手术节段及邻近节段ROM差异无统计学意义(P > 0.05,表 3),末次随访时两组手术节段ROM均减小,TLIF组因行植骨融合ROM降至0°,明显低于Dynesys组,差异有统计学意义(P < 0.05,表 3)。Dynesys组末次随访时上位、下位邻近节段ROM与术前相比差异无统计学意义(P > 0.05,表 3),TLIF组末次随访时上位、下位邻近节段ROM较术前均增加,差异有统计学意义(P < 0.05,表 3)。典型病例影像学资料见图 1,2。
|
|
表 3 手术前后不同节段ROM Table 3 Pre-and post-operative ROM |
|
男,65岁,行Wiltse入路Dynesys动态内固定 a,b:术前MRI示L4,5椎间盘突出,双侧侧方椎管及隐窝狭窄 c~f:术前正侧位及过伸过屈位X线片示椎体稳定,腰椎活动受限 g,h:术后1个月正侧位X线片示Dynesys螺钉位置良好 i~l:术后末次随访时正侧位及过伸过屈位X线片示椎体稳定,Dynesys螺钉无松动,腰椎活动度较术前有所改善 Male, 65 years old, underwent Dynesys stabilization through Wiltse approach a, b:Preoperative MRI showing L4, 5 disc herniation, stenosis of both lateral canal and recess c-f:Preoperative anteroposterior, lateral, hyperextension and hyperflexion roentgenographs show vertebral bodies are stable, and movement of lumbar is restricted g, h:Anteroposterior and lateral roentgenographs at postoperative 1 month show positions of screws are good i-l:Anteroposterior, lateral, hyperextension and hyperflexion roentgenographs at final follow-up show vertebral bodies are stable, and screws have no loosening, and activity of lumbar spine was improved compared with that of pre-operation 图 1 Dynesys组典型病例影像学资料 Figure 1 Imaging data of a typical case in Dynesys group |

|
男,75岁,行Wiltse入路TLIF融合术 a,b:术前MRI示L4,5椎管狭窄 c~f:术前正侧位及过伸过屈位X线片 g,h:术后3个月CT三维重建 i~l:术后末次随访时正侧位及过伸过屈位X线片 Male, 75 years old, underwent TLIF through Wiltse approach a, b:Preoperative MRI showing L4, 5 stenosis c-f:Preoperative anteroposterior, lateral, hyperextension and hyperflexion roentgenographs g, h:3D-CT reconstruction at postoperative 3 month i-l:Anteroposterior, lateral, hyperextension and hyperflexion roentgenographs at final follow-up 图 2 TLIF组典型病例影像学资料 Figure 2 Imaging data of a typical case in TLIF group |
Gologorsky等[3]报道,腰椎融合术因植骨量不足、植骨区处理不仔细等原因往往会导致假关节形成,尽管假关节形成的病例中50%没有临床症状,但仍有部分疼痛的假关节需手术翻修。老年患者自身体质弱,心肺功能较差并伴有多系统并发症,手术和麻醉风险较年轻人要高,在有效进行减压内固定治疗时,应遵循微创外科和精准外科尽量缩短手术时间、减少手术创伤的原则。Liu等[9]认为Dynesys内固定保留了腰椎后纵韧带、棘突、棘突间韧带等结构,能够较好地维持脊柱中线结构,增强脊柱稳定性,有效减轻患者术后疼痛。通过结合Wiltse入路的手术方式,可以更好地保护脊柱中线结构,同时减少因椎旁肌过度剥离及牵拉引起的术后腰背痛。相对于腰椎后路融合术,Dynesys内固定因不需植骨融合,避免了因融合而带来的各种并发症,如假关节的形成,各种内固定的松动、断裂、位移,椎间融合的松动、位移,自体取骨引起的术后取骨区长期疼痛,使用异体骨带来的潜在感染风险,术后需长期的外固定等[15-16]。
本研究对Wiltse入路Dynesys内固定与TLIF进行比较,观察发现,Dynesys组手术时间、术中出血量及术后引流量均小于TLIF组,对于心肺代偿功能较差的老年腰椎椎管狭窄患者,更有利于术中麻醉的控制,降低手术和麻醉的风险及并发症的发生率。两组患者均在术后2~3 d下床活动,Dynesys组需佩戴软腰围2~3周,TLIF组因植骨融合需佩戴腰部支具3~4个月,而长期佩戴支具会导致患者对支具产生依赖性,减少腰部肌肉的锻炼,出现腰椎过度保护,导致腰部肌肉萎缩、腰部僵硬。两组患者术后5 d的ODI及VAS评分显示Dynesys组优于TLIF组,提示相较于TLIF,Dynesys内固定创伤更小,减轻了患者术后慢性腰痛的发生,利于患者早期恢复的同时降低了手术后的炎症和应激反应,而这些反应会导致内分泌系统及免疫系统失衡,促使高血压、心率失常、心肌梗死等并发症的发生。两组患者术后末次随访时ODI及VAS评分较术前均明显改善,表明两种手术方法均可取得良好的临床疗效,但Dynesys系统在老年腰椎椎管狭窄症中的应用更体现了微创和精准的现代外科理念,有利于老年患者的早期康复,降低了术中及术后并发症的发生率。
3.2 两种术式对腰椎ROM及邻近节段的影响TLIF一直是治疗腰椎退行性变的有效方法,但近年来,有文献指出TLIF可引起腰背部肌肉萎缩、正常脊柱功能丧失及ADS[5],而Dynesys内固定越来越多地应用于临床当中。有研究表明,Dynesys内固定可以保护腰椎的稳定性,保留腰椎的部分功能,同时防止ADS的发生,在一些腰椎退行性变中,较TLIF是一种更好的选择[17]。Dynesys内固定允许恢复椎间盘的高度,使得椎体在运动时可以恢复适当的位置。在生物力学特性上,Schulte等[18]证明了Dynesys内固定除了减压外可以更好地限制固定节段的后伸和侧曲。Gédet等[19]提出Dynesys内固定分别减少固定节段在后伸、侧曲和旋转上的ROM至正常参数的26%、33%和76%。而且,相较于TLIF,Dynesys系统因未行后路植骨融合,避免了因置入物阻止在不稳定节段的伴生运动而导致的ROM的减少。
以上研究更多的是以非老年患者为研究样本,但Dynesys系统对老年腰椎椎管狭窄患者腰椎ROM的影响则较少报道。本研究中两组均为老年腰椎椎管狭窄患者,对比两组患者术前及末次随访时的腰椎ROM发现,Dynesys组固定节段ROM由术前的7.4°±0.5°降至5.2°±0.4°,而TLIF组固定节段的ROM因植骨融合而完全丧失。Dynesys组上位邻近节段ROM由术前的8.0°±0.6°改变为末次随访时的8.1°±0.6°,下位邻近节段ROM由术前的8.1°±0.6°改变为末次随访时的8.3°±0.6°,并未发生明显改变;TLIF组上位邻近节段ROM由术前的7.9°±0.5°升高至末次随访时的9.2°±0.9°,下位邻近节段ROM由术前的8.3°±0.6°升高至末次随访时的9.7°±0.7°;可能是因为Dynesys内固定部分保留了固定节段的ROM,避免了邻近节段因代偿融合节段的功能导致ROM的增加,表明在保留椎间ROM方面Dynesys内固定更具优势。
Dynesys内固定可以防止ASD与其更接近腰椎正常生理活动有关。Dynesys内固定在限制腰椎后伸及侧曲的同时,可以更好地保留腰椎的前屈及旋转功能,保留了固定节段的部分运动功能,降低了邻近椎间盘的压力,从而防止ASD的发生。而TLIF术后造成的有限的腰椎运动及假关节的形成会加速ASD的发生。Zhang等[12]通过4年随访研究得出,与后路腰椎椎间融合术(PLIF)相比,Dynesys内固定术后ASD的发生更少,因ASD行二次手术的发生率更低。而老年腰椎椎管狭窄患者本身体质较弱,内科疾病复杂,且骨质条件较差,二次手术将会更加困难,且风险更高,在患者手术指征同时满足融合术与Dynesys内固定术时,后者更符合微创外科的理念。本研究中,两组均没有因ASD行二次手术的患者,可能与本研究随访时间较短有关。
3.3 结论本研究结果显示,经Wiltse入路Dynesys内固定及经Wiltse入路TLIF在治疗老年单节段腰椎椎管狭窄上均可获得良好疗效。Dynesys内固定在减轻术后疼痛及术后早期恢复上较TLIF更具优势,同时降低了老年患者的手术风险及并发症发生率,避免了假关节的形成和因内固定失败而导致的翻修手术,而且能更好地保留腰椎固定节段的ROM,减少邻近节段因代偿其功能引起的ROM的增加,但对其是否能有效防止ASD发生,还需长期的随访观察。
| [1] | Zhou C, Tian YH, Zheng YP, et al. Mini-invasive transforaminal lumbar interbody fusion through Wiltse approach to treating lumbar spondylolytic Spondylolisthesis[J]. Orthop Surg, 2016, 8(1): 44–50. DOI:10.1111/os.12224 |
| [2] | Olivier E, Beldame J, Ould Slimane M, et al. Comparison between one midline cutaneous incision and two lateral incisions in the lumbar paraspinal approach by Wiltse: a cadaver study[J]. Surg Radiol Anat, 2006, 28(5): 494–497. DOI:10.1007/s00276-006-0123-y |
| [3] | Gologorsky Y, Skovrlj B, Steinberger J, et al. Increased incidence of pseudarthrosis after unilateral instrumented transforaminal lumbar interbody fusion in patients with lumbar spondylosis: clinical article[J]. J Neurosurg Spine, 2014, 21(4): 601–607. DOI:10.3171/2014.6.SPINE13488 |
| [4] | Kettler A, Schmoelz W, Kast E, et al. In vitro stabilizing effect of a transforaminal compared with two posterior lumbar interbody fusion cages[J]. Spine (Phila Pa 1976), 2005, 30(22): E665–670. DOI:10.1097/01.brs.0000186466.01542.8c |
| [5] | Cakir B, Carazzo C, Schmidt R, et al. Adjacent segment mobility after rigid and semirigid instrumentation of the lumbar spine[J]. Spine (Phila Pa 1976), 2009, 34(12): 1287–1291. DOI:10.1097/BRS.0b013e3181a136ab |
| [6] | Lee SE, Jahng TA, Kim HJ. Clinical experiences of non-fusion dynamic stabilization surgery for adjacent segmental pathology after lumbar fusion[J]. Int J Spine Surg, 2016, 10: 8. |
| [7] | Stoll TM, Dubois G, Schmarzenhach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system[J]. Eur Spine, 2002, 11(Suppl 2): S170–178. |
| [8] | Maserati MB, Tormenti MJ, Panczykowski DM, et al. The use of a hybrid dynamic stabilization and fusion system in the lumbar spine: preliminary experience[J]. Neurosurg Focus, 2010, 28(6): E2. DOI:10.3171/2010.3.FOCUS1055 |
| [9] | Liu C, Wang L, Tian JW. Early clinical effects of the Dynesys system plus transfacet decompression through the Wiltse approach for the treatment of lumbar degenerative diseases[J]. Med Sci Monit, 2014, 20: 853–859. DOI:10.12659/MSM.890292 |
| [10] | Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127–1131. |
| [11] | Lee CH, Jahng TA, Hyun SJ, et al. Dynamic stabilization using the Dynesys system versus posterior lumbar interbody fution for the treatment of degenerative lumbar spinal disease: a clinical and radiological outcomesbased meta-analysis[J]. Neurosurg Focus, 2016, 40(1): E7. DOI:10.3171/2015.10.FOCUS15426 |
| [12] | Zhang Y, Shan JL, Liu XM, et al. Comparison of the Dynesys dynamic stabilization system and posterior lumbar interbody fusion for lumbar degenerative disease[J]. PLoS One, 2016, 11(1): e0148071. DOI:10.1371/journal.pone.0148071 |
| [13] | Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271–273. |
| [14] | Khashan M, Lidar Z, Salame K, et al. Minimally invasive spinal decompression in patients older than 75 years of age: perioperative risks, complications, and clinical outcomes compared with patients younger than 45 years of age[J]. World Neurosurg, 2016, 89: 337–342. DOI:10.1016/j.wneu.2016.02.018 |
| [15] | Yu SW, Yang SC, Ma CH, et al. Comparison of Dynesys posterior stabilization and posterior lumbar interbody fusion for spinal stenosis L4L5[J]. Acta Orthop Belg, 2012, 78(2): 230–239. |
| [16] | Schaeren S, Broger I, Jeanneret B. Minimum fouryear follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization[J]. Spine (Phila Pa 1976), 2008, 33(18): E636–642. DOI:10.1097/BRS.0b013e31817d2435 |
| [17] | Lee SE, Jahng TA, Kim HJ. Facet joint changes after application of lumbar nonfusion dynamic stabilization[J]. Neurosurg Focus, 2016, 40(1): E6. DOI:10.3171/2015.10.FOCUS15456 |
| [18] | Schulte TL, Hurschler C, Haversath M, et al. The effect of dynamic, semi-rigid implants on the range of motion of lumbar motion segments after decompression[J]. Eur Spine J, 2008, 17(8): 1057–1065. DOI:10.1007/s00586-008-0667-0 |
| [19] | Gédet P, Haschtmann D, Thistlethwaite PA, et al. Comparative biomechanical investigation of a modular dynamic lumbar stabilization system and the Dynesys system[J]. Eur Spine J, 2009, 18(10): 1504–1511. DOI:10.1007/s00586-009-1077-7 |
 2017, Vol.15
2017, Vol.15  Issue(2): 82-88
Issue(2): 82-88


