近年来,Zero-P椎间融合器被广泛应用于颈椎前路融合术中。与传统融合器并钛板组合相比,Zero-P可在改善患者症状、有效维持术后颈椎稳定性的同时,降低吞咽困难发生率,缩短手术时间,减少术中出血量,并减缓邻近节段退变(ASD)发生[1-4]。诸多文献报道Zero-P治疗颈椎退变性疾病近、中期疗效满意[1, 4-5],然而对于三节段Zero-P颈椎融合术后中期影像学变化与传统融合器并钛板组合相比有何差异,目前研究较少。本研究拟通过中期随访,从手术疗效、颈椎曲度、C4~7 Cobb角、吞咽困难发生率、ASD发生率等方面与传统融合器并钛板融合术式进行对比,揭示Zero-P治疗C4/C5/C6/C7三节段颈椎退变性疾病的中期疗效及影像学变化,以更全面地认识、评价两种术式。
1 资料与方法1.1 病例纳入和排除标准纳入标准:① 根据颈椎X线片、MRI及CT影像诊断为脊髓型颈椎病、混合型颈椎病,且非手术治疗无效;② 接受颈前路C4/C5/C6/C7三节段减压融合术,使用Zero-P(A组)或传统椎间融合器并钛板(B组)。排除标准:① 因颈椎感染、结核、肿瘤及创伤等原因行C4/C5/C6/C7减压融合内固定术;② 涉及椎体切除;③ 接受C4~7翻修手术;④ 病例资料欠完整。根据以上纳入和排除标准,共纳入2009年7月—2013年5月接受C4/C5/C6/C7颈椎融合手术的患者72例,其中A组30例,B组42例。
1.2 手术方法所有患者均由同一名高年资脊柱外科医师主刀,采用标准Smith-Robinson颈椎融合技术。在手术节段切除椎间盘,为脊髓及神经根彻底减压后,A组置入大小合适、填充自体骨和人工骨混合物的Zero-P椎间融合器,并用螺钉锁定。B组则置入大小合适、填充自体骨和人工骨混合物的传统椎间融合器,同时用螺钉将合适长度的钛板固定于椎体前缘。术中透视显示两组患者椎间融合器均大小合适、位置良好。所有患者均于术后第2天下床活动,颈部均用费城颈托固定2个月。2个月后摘除颈托,恢复正常生活。
1.3 观察指标和随访对所有患者于术前、术后采用日本骨科学会(JOA)评分[6]、颈椎功能障碍指数(NDI)[7]评价功能改善情况,术后48 h、2个月、6个月采用Bazaz系统[8]评估是否存在吞咽困难,术前及术后2个月、6个月、1年、2年及近期随访复查颈椎正侧位及过伸过屈位X线片,术后6个月及末次随访时加行颈椎CT三维重建。影像学指标包括颈椎曲度、C4~7 Cobb角、融合率、ASD发生率。颈椎曲度、C4~7 Cobb角于颈椎侧位X线片上测量,颈椎曲度为C2椎体上终板与C7椎体下终板间的角度,C4~7 Cobb角为C4椎体上终板与C7椎体下终板间的角度。如C7显影不清,则选用最下位显影清晰的椎体下终板作为颈椎曲度或C4~7 Cobb角测量标志。由高年资脊柱外科医师根据术后随访时的颈椎CT检查结果判定颈椎是否融合,是否存在ASD。
1.4 统计学处理采用SPSS 18.0软件对数据进行统计学分析。其中JOA评分、NDI、颈椎曲度、C4~7 Cobb角为计量资料,采用x±s描述,并用独立样本t检验进行比较。吞咽困难发生率、融合率及ASD发生率为计数资料,采用χ2检验或Fisher精确概率检验进行比较。以P < 0.05为差异有统计学意义。
2 结果A组30例,男18例、女12例,年龄(50.4±4.9)岁,随访时间(56.6±14.6)个月;B组42例,男24例、女18例,年龄(51.0±5.1)岁,随访时间(58.6±13.7)个月。两组患者年龄、性别、随访时间差异无统计学意义,术前JOA评分、NDI、颈椎曲度、C4~7 Cobb角等差异也无统计学意义(表 1),具有可比性。
|
|
表 1 统计数据 Table 1 Statistical data |
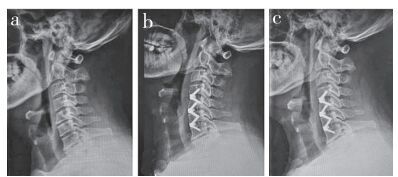
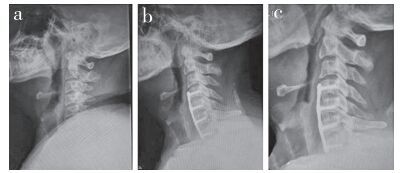
两组患者术后JOA评分、NDI改善差异无统计学意义(表 1)。典型病例影像学资料见图 1,2。术后两组患者颈椎曲度呈缓慢减小趋势,术后2个月、1年及2年随访时,两组患者颈椎曲度差异无统计学意义;末次随访时B组颈椎曲度大于A组,差异有统计学意义(P < 0.05,表 1)。术后B组C4~7 Cobb角维持良好,而A组呈缓慢降低趋势,并于术后2年及末次随访时显著低于B组,差异有统计学意义(P < 0.05,表 1)。A组患者颈椎曲度及C4~7 Cobb角丢失趋势虽快于B组,但随访过程中两组患者JOA评分、NDI并无显著差异,说明这部分丢失并未导致患者出现症状及阳性体征。
|
a:术前X线片示多节段脊髓型颈椎病b:术后1年X线片示C4~7 Cobb角15.5°,邻近节段与术前相仿c:术后3年X线片示C4~7 Cobb角11.5°,邻近节段未见明显退变加速 a:Preoperative roentgenograph shows multi-level cervical spondylotic myelopathy b:Roentgenograph at postoperative 1 year show C4-7 Cobb's angle is 15.5°, adjacent segment is similar to pre-operation c:Roentgenograph at postoperative 3 years show C4-7 Cobb's angle is 11.5°, and no obvious accelerated degeneration is found at adjacent segment 图 1 A组典型病例影像学资料 Figure 1 Imaging data of a typical case in group A |
|
a:术前X线片示多节段脊髓型颈椎病b:术后1年X线片示Cx Cobb角12.3°,上位邻近节段间隙狭窄,椎体前缘骨质增生c:术后3年X线片示Cx Cobb角11.5°,上位邻近节段骨质增生明显加速 a:Preoperative roentgenograph shows multi-level cervical spondylotic myelopathy b:Roentgenograph at postoperative 1 year show Cx Cobb's angle is 12.3°, stenosis and vertebral bone hyperplasia in upper adjacent segment space c:Roentgenograph at postoperative 3 years show Cx Cobb's angle is 11.5°, and bone hyperplasia of upper adjacent segment significantly accelerated 图 2 B组典型病例影像学资料 Figure 2 Imaging data of a typical case in group B |
术后48 h时,两组患者吞咽困难发生率差异无统计学意义;术后2个月时,A组患者吞咽困难发生率低于B组,差异有统计学意义(P < 0.05,表 1);术后6个月时两组患者吞咽困难发生率差异无统计学意义。两组患者均达到有效骨性融合,且末次随访时融合率均达100%(表 1)。两组患者ASD发生率差异亦无统计学意义(表 1)。
3 讨论颈椎前路椎间盘切除减压植骨融合内固定术被广泛应用于治疗需要手术干预的颈椎退变性疾病。其中,颈椎前路椎间盘切除、椎间融合器置入及钛板内固定术至今仍被认为是治疗无法进行人工椎间盘置换手术颈椎退变性疾病患者的金标准[3-4, 9]。该术式通过有效的减压融合,不仅可缓解颈椎退行性疾病患者颈肩部疼痛、肢体麻木及行走不稳等症状,而且可长期维持颈椎稳定性[10-11]。但该术式存在气管食管损伤、术后吞咽困难及加速ASD等缺点,其中,术后吞咽困难是该术式最常见的术后并发症[3, 12]。Zero-P颈椎椎间融合器被广泛认为可有效降低术后吞咽困难发生率,且节段越长,效果越显著[13-14]。本研究通过对Zero-P治疗C4/C5/C6/C7三节段颈椎退行性疾病的中期随访,并与传统融合器并钛板融合进行比较,全面分析其临床疗效及影像学变化,以更全面地认识两种术式,为临床决策提供依据。
JOA评分和NDI是评价手术疗效、选择术式的重要参考指标。一项对33个临床随机对照研究、2267例颈椎融合术患者资料的系统回顾分析显示,不同术式之间,术后JOA评分的改善及颈肩部疼痛缓解并无显著差异[1]。有学者认为,年龄大、病程长、致压节段长、合并后纵韧带骨化、脊髓高信号及减压不彻底等是颈椎退行性疾病患者术后JOA评分改善有限的重要因素[9]。近年有文献报道,Zero-P椎间融合器与传统颈椎前路椎间盘切除融合术比较,短期及中期随访的JOA评分、NDI无显著差异[11]。本研究发现,随访期间,采用Zero-P椎间融合器组与传统融合器并钛板组术后JOA评分、NDI差异均无统计学意义,说明两种术式均能在C4/C5/C6/C7节段的颈椎融合中取得满意疗效。
术后有效、长期的颈椎曲度维持是防止术后远期再出现颈肩部疼痛及神经压迫症的重要因素,而手术节段Cobb角的减少是造成术后颈椎曲度变直的重要原因。据报道,使用Zero-P椎间融合器患者术后远期更易于出现手术节段Cobb角的丢失,且手术节段越长,Cobb角丢失速度越快[13, 15]。传统椎间融合器并钛板的组合,因融合器支撑及钛板锚定的双重固定作用,手术节段Cobb角相对不易丢失,且手术节段越长,丢失速度越慢[16-17]。本研究发现,传统椎间融合器并钛板组C4~7 Cobb角在随访期间相对平稳,而Zero-P椎间融合器组则呈缓慢减少趋势,并于术后2年时明显低于传统椎间融合器并钛板组,从而导致末次随访时颈椎曲度亦显著低于传统椎间融合器并钛板组。然而,两组患者影像学上的差异并未导致患者在中期随访中出现症状或阳性体征,两组临床疗效相似,但进一步的变化还有待于更长时间的随访予以揭示。Zero-P融合器组手术节段曲度的丢失可能与置入融合器偏小、融合器缓慢下沉、手术节段微动等因素相关。因此,对于用Zero-P进行C4/C5/C6/C7融合的患者,术后2年后应加强随访及康复指导力度,以尽可能维持颈椎曲度。
术后吞咽困难是颈椎前路手术早期常见的并发症。传统融合器并钛板融合患者中,钛板置于椎体前缘,紧贴食管后壁,不可避免对食管产生刺激,且钛板越厚,折弯曲度越大,长度越长,对食管刺激作用越大;同时,术后钛板周围会形成一层瘢痕包裹,容易与食管后壁粘连,从而引发吞咽困难[8, 10, 19]。Zero-P作为一种零切迹融合器,可有效消除颈前置入物对食管后壁的刺激,降低术后吞咽困难发生率,且手术节段越长,其优势越明显[8, 18]。本研究结果支持上述观点。两组患者在术后48 h时,吞咽困难发生率无明显差异,Zero-P组患者由于没有颈前钛板刺激,术后2个月时吞咽困难迅速得以改善,而传统融合器并钛板组则改善有限,甚至有2例患者吞咽困难持续 > 6个月。
ASD是颈椎融合术后中期常见并发症。传统融合器并钛板融合术被认为具有较高的ASD发生率,其主要的原因包括钛板头尾两端对邻近节段椎间盘和椎体的机械刺激,融合后邻近节段椎间隙负荷增加、活动度增大等[5, 15, 20]。Zero-P没有钛板对邻近节段的刺激,且融合间隙的微动可部分缓解邻近节段压力,因而能一定程度上保护邻近节段[21]。然而,本研究发现,对于C4/C5/C6/C7三节段融合患者,两种手术的中期ASD发生率并无显著差异,其长期影响仍有待进一步观察。
在融合器相关并发症方面,融合器下沉被认为是Zero-P最常见的并发症,文献报道其发生率高达32.3%[4, 14],但本研究中的30例患者均未发生融合器下沉、移位等并发症,融合率达100%。理论上,多节段Zero-P中,中间的椎体被置入4枚螺钉,颈椎屈伸活动时应力大,易发生骨折,然而本研究随访的患者中无一例发生椎体骨折。本研究结果显示应用Zero-P进行C4/C5/C6/C7融合术后并发症相对较少。
综上所述,Zero-P用于颈椎C4/C5/C6/C7融合时中期疗效满意,并发症少,其可有效降低术后2个月吞咽困难发生率,但对术后颈椎曲度及C4~7 Cobb角的维持作用较差。本研究为回顾性研究,且样本量较少,相关结论仍需大样本、多中心、更长时间随访的研究予以进一步验证。
| [1] | Shao H, Chen J, Ru B, et al. Zero-profile implantversus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis:a meta analysis[J].J Orthop Surg Res, 2015, 10: 148. DOI:10.1186/s13018-015-0290-9 |
| [2] | Wang Z, Zhu R, Yang H, et al. Zero-profile implant (Zero-p) versus plate cage benezech implant(PCB) in the treatment of single-level cervical spondylotic myelopathy[J].BMC Musculoskelet Disord, 2015, 16: 290. DOI:10.1186/s12891-015-0746-4 |
| [3] | Hofstetter CP, Kesavabhotla K, Boockvar JA. Zeroprofile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating[J].J Spinal Disord Tech, 2015, 28(5): E284–290. DOI:10.1097/BSD.0b013e31828873ed |
| [4] | Barbagallo GM, Romano D, Certo F, et al. Zero-P:a new Zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on Zero-profile devices[J].Eur Spine J, 2013, 22(Suppl 6): S868–878. |
| [5] | Ji GY, Oh CH, Shin DA, et al. Stand-alone cervical cages versus anterior cervical plates in 2-level cervical anterior interbody fusion patients:analysis of adjacent segment degeneration[J].J Spinal Disord Tech, 2015, 28(7): E433–438. DOI:10.1097/BSD.0b013e3182a355ad |
| [6] | Yonenobu K, Wada E, Tanaka T, et al. Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire(JOACMEQ):Part 2. Endorsement of the alternative item[J].J Orthop Sci, 2007, 12(3): 241–248. DOI:10.1007/s00776-007-1119-0 |
| [7] | Vernon H, Mior S. The Neck Disability Index:a study of reliability and validity[J].J Manipulative Physiol Ther, 1991, 14(7): 409–415. |
| [8] | Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery:a prospective study[J].Spine(Phila Pa 1976), 2002, 27(22): 2453–2458. DOI:10.1097/00007632-200211150-00007 |
| [9] | Zhang L, Wang J, Tao Y, et al. Outcome evaluation of Zero-profile implant compared with an anterior plate and cage used in anterior cervical discectomy and fusion:a two-year follow-up study[J].Turk Neurosurg, 2016, 26(3): 416–422. |
| [10] | Min Y, Kim WS, Kang SS, et al. Incidence of dysphagia and serial videofluoroscopic swallow study findings after anterior cervical discectomy and fusion:a prospective study[J].Clin Spine Surg, 2016, 29(4): E177–181. |
| [11] | Chang H, Baek DH, Choi BW. Efficacy of Zero-profile implant in anterior fusion to treat degenerative cervical spine disease:comparison with techniques using bone graft and anterior plating[J].J Neurol Surg A Cent Eur Neurosurg, 2015, 76(4): 268–273. DOI:10.1055/s-00000180 |
| [12] | Rihn JA, Kane J, Albert TJ, et al. What is the incidence and severity of dysphagia after anterior cervical surgery?[J].Clin Orthop Relat Res, 2011, 469(3): 658–665. DOI:10.1007/s11999-010-1731-8 |
| [13] | Duan Y, Yang Y, Wang Y, et al. Comparison of anterior cervical discectomy and fusion with the Zeroprofile device versus plate and cage in treating cervical degenerative disc disease:a meta-analysis[J].J Clin Neurosci, 2016, 33: 11–18. DOI:10.1016/j.jocn.2016.01.046 |
| [14] | Cho HJ, Hur JW, Lee JB, et al. Cervical stand-alone polyetheretherketone cage versus Zero-profile anchored spacer in single-level anterior cervical discectomy and fusion:minimum 2-year assessment of radiographic and clinical outcome[J].J Korean Neurosurg Soc, 2015, 58(2): 119–124. DOI:10.3340/jkns.2015.58.2.119 |
| [15] | Matsumoto M, Okada E, Ichihara D, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration:comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study[J].Spine(Phila Pa 1976), 2010, 35(1): 36–43. DOI:10.1097/BRS.0b013e3181b8a80d |
| [16] | Alimi M, Njoku I, Hofstetter CP, et al. Anterior cervical discectomy and fusion(ACDF):comparison between Zero profile implants and anterior cervical plate and spacer[J].Cureus, 2016, 8(4): e573. |
| [17] | Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications[J].Spine(Phila Pa 1976), 2007, 32(21): 2310–2317. DOI:10.1097/BRS.0b013e318154c57e |
| [18] | Skeppholm M, Ingebro C, Engström T, et al. The Dysphagia Short Questionnaire:an instrument for evaluation of dysphagia:a validation study with 12 months' follow-up after anterior cervical spine surgery[J].Spine(Phila Pa 1976), 2012, 37(11): 996–1002. DOI:10.1097/BRS.0b013e31823a7a5b |
| [19] | Anderson KK, Arnold PM. Oropharyngeal dysphagia after anterior cervical spine surgery:a review[J].Global Spine J, 2013, 3(4): 273–286. DOI:10.1055/s-0033-1354253 |
| [20] | Luo J, Gong M, Huang S, et al. Incidence of adjacent segment degeneration in cervical disc arthroplasty versus anterior cervical decompression and fusion meta-analysis of prospective studies[J].Arch Orthop Trauma Surg, 2015, 135(2): 155–160. DOI:10.1007/s00402-014-2125-2 |
| [21] | Mattei TA, Teles AR, Dinh DH. Vertebral body fracture after anterior cervical discectomy and fusion with zeroprofile anchored cages in adjacent levels:a cautionary tale[J].Eur Spine J, 2016. |
 2017, Vol.15
2017, Vol.15  Issue(3): 129-133
Issue(3): 129-133


