2. 中国医科大学附属盛京医院影像科, 辽宁 110004;
3. 中国医科大学附属盛京医院临床流行病学教研室, 辽宁 110004
2. Department of Radiology, Shengjing Hospital, China Medical University, Shenyang 110004, Liaoning, China;
3. Department of Clinical Epidemiology, Shengjing Hospital, China Medical University, Shenyang 110004, Liaoning, China
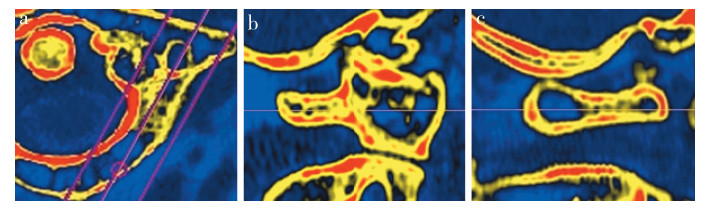
随着老龄化社会的到来和医疗技术手段的不断发展,临床上需要通过手术内固定治疗的寰枢椎不稳病例逐年增多[1]。寰枢椎椎弓根螺钉固定是目前被广泛接受的治疗寰枢椎不稳的理想手术方式[2-5]。由于寰椎骨性结构不规则、个体差异较大,临床上常出现由于寰椎椎弓根钉入钉点过于狭小而无法完成螺钉置入的情况,需要术前改变钉道规划或术中临时更换其他方式固定[6-10]。钉棒固定具有优异的生物力学性能及良好的临床效果,成为各种常规固定和替代固定的首选方法[11-16]。笔者所在研究团队通过对寰椎CT影像的研究发现,后弓-横突皮质骨包绕的髓腔存在着由后内侧向前外侧的自然腔道,该腔道后内侧入钉点更靠近中线,暴露和操作更容易,同时该腔道内CT灰度值反映出的骨量比其他位置更大(图 1),更大的骨量意味着能够为螺钉提供更好的把持力。本研究通过对寰椎后弓-横突髓腔相关解剖学参数的测量,为临床寻求寰椎替代固定方案提供依据。
|
a:后弓-横突横断面 b:后弓-横突矢状面 c:寰椎后弓-横突髓腔矢状面 a: Transverse section of posterior arch-transverse process b: Sagittal section of posterior arch-transverse process c: Sagittal section of medullary cavity of posterior arch-transverse process of atlas 图 1 寰椎后弓-横突髓腔内CT灰度值反映的骨量高于其他部位 Figure 1 Bone mass reflected by medullary cavity grey value on CT scan of posterior arch-transverse process of atlas is higher than that of other parts of atlas |
选择2016年1月—2017年6月本院影像归档和通信系统(PACS)中18~70岁患者颈椎三维CT数据,排除骨折、畸形、感染等情况。共纳入200例,其中男100例,女100例;全组年龄(54.95±11.93)岁,男(53.58±12.30)岁,女(56.33±11.45)岁,男女年龄差异无统计学意义(P>0.05)。
1.2 扫描方法所有患者均于本院影像科完成颈椎三维CT扫描,所用设备为德国Siemens公司Siemens sensation 64层CT机。扫描参数:120 kV,250~300 mA,层厚1 mm。患者取仰卧位,头颅居中,人体正中矢状面与检查床正中线位于同一平面,颈部自然位。CT扫描基线与椎管横径平行,从头侧向足侧扫描,扫描范围为C0~T1。扫描完成后进行薄层重建,重建间隔为0.4 mm。将薄层数据传输至PACS,完成多角度重建,利用系统自带软件对解剖学参数进行测量。
1.3 测量方法在寰椎横断面像上,选取后弓-横突髓腔中心线最长轴切面为测量截面(图 2a),并在该截面的矢状面(图 2b)和横断面角度重建图像上对相关解剖学参数进行测量。所有参数的测量由2名脊柱外科医师和1名影像科医师完成,将3人对同一参数的测量值取平均值作为最终结果。入钉点与后结节距离:横断面上后弓-横突髓腔中心线最长轴与同侧后弓后方皮质骨交点至后结节后方皮质骨中心点的距离(图 2c)。入钉角度与矢状面夹角:横断面上后弓-横突髓腔中心线最长轴与正中矢状面的夹角(图 2c)。入钉角度与横断面夹角:矢状面上后弓-横突髓腔中心线最长轴与侧位像横断面夹角(图 2d)。钉道长度:矢状面上后弓-横突髓腔中心线延长线与前方横突孔后内侧皮质及后弓后外侧皮质骨交点之间的距离(图 2d)。椎动脉沟狭窄处髓腔高度:矢状面上椎动脉沟狭窄处上下皮质骨之间的最小垂直距离(图 2d)。入钉点髓腔最大高度的测量:矢状面上后方入钉点髓腔上下皮质骨之间的最大垂直距离(图 2d)。

|
a:后弓-横突髓腔中心线最长轴横断面 b:后弓-横突髓腔中心线最长轴(3.04 mm)矢状面 c:横断面上对入钉点与后结节距离(10.57 mm)、入钉角度与矢状面夹角(42°)的测量 d:矢状面上对入钉角度与横断面夹角(5°)、钉道长度(20.49 mm)、椎动脉沟狭窄处髓腔高度(1.52 mm)以及入钉点髓腔最大高度(4.17 mm)的测量 a: Transverse section along longest axis of medullary cavity centerline of posterior arch-transverse process of atlas b: Sagittal section along longest axis of medullary cavity centerline of posterior arch-transverse process of atlas(3.04 mm) c: On transverse section, distance between entry point and posterior tubercle(10.57 mm), angle between trajectory and sagittal plane are measured(42°) d: On sagittal section, angle between trajectory and transverse section(5°), length of trajectory(20.49 mm), height of minimal medullary cavity of vertebral artery groove(1.52 mm) and height of maximal medullary cavity of entry poin(t 4.17 mm) are measured 图 2 寰椎后弓-横突髓腔的影像解剖学参数测量 Figure 2 Measurement of image anatomic parameters of medullary cavity of posterior arch-transverse process of atlas |
采用SPSS 16.0软件对数据进行统计学分析。检验数据样本为正态分布,数据采用x±s表示。男性和女性测量数据经过方差齐性检验,采用独立样本t检验比较组间差异。以P<0.05为差异有统计学意义。
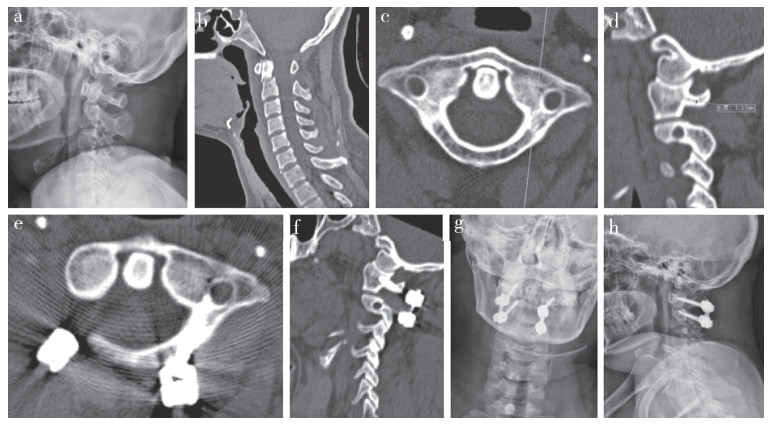
2 结果寰椎后弓-横突髓腔的影像解剖学参数测量结果见表 1。男性寰椎后弓-横突髓腔钉道在入钉点与后结节距离、钉道长度、椎动脉沟狭窄处髓腔高度和入钉点髓腔最大高度均大于女性,差异有统计学意义(P<0.05),不同性别之间入钉角度与矢状面夹角和入钉角度与横截面夹角差异无统计学意义(P>0.05)。经有限病例初步证实该置钉方式具有可行性(图 3)。
|
|
表 1 寰椎后弓-横突髓腔的影像解剖学参数测量结果 Table 1 Anatomical parameters of medullary cavity of posterior arch-transverse process of atlas |
|
女,40岁 a,b:术前X线片及三维CT示Ⅱ型齿突骨折 c,d:术前三维CT测量寰椎后弓左侧椎弓根螺钉入钉点髓腔仅1.17 mm e,f:经寰椎左侧后弓-横突髓腔置入螺钉 g,h:术后X线片示寰枢椎相对位置良好,齿突复位 Female, 40-year-old a, b: Preoperative roentgenograph and three-dimensional CT scan show type Ⅱ odontoid process fracture c, d: Preoperative three-dimensional CT scans show height of minimal medullary cavity of vertebral artery groove is 1.17 mm e, f: Screw is inserted via left medullary cavity of posterior arch-transverse process of atlas g, h: Postoperative roentgenographs show good atlantoaxial relative position and anatomical reduction of fractured odontoid process 图 3 Ⅱ型齿突骨折行寰枢椎后路固定患者影像学资料 Figure 3 Imaging data of a tapical case with type Ⅱ odontoid process fracture treated by atlantoaxial posterior fixation |
随着脊柱外科手术技术的不断提高和对疾病认识的不断深入,寰枢椎后路固定手术治疗寰枢椎不稳的病例逐年增多[1]。由于具有更好的生物力学性能、更少的并发症,后路钉棒固定系统已逐渐取代钢丝固定、钉板固定,成为应用最为广泛的后路固定方式[17]。寰枢椎后路经关节突螺钉技术一度被称为寰枢椎后路手术的“金标准”,虽然具有良好的稳定性,但其椎动脉损伤、舌下神经损伤、脊髓损伤等严重并发症不容忽视[15, 18]。为避免此类并发症,2001年Harms等[19]提出寰椎侧块螺钉固定技术。2002年Resnick等[20]在前人基础上提出了经寰椎后弓固定侧块的椎弓根螺钉技术,该技术使螺钉在骨性通道内走行距离更长,钉骨结合面更大,螺钉把持力更高,生物力学性能更优越,同时避免了置入Harms侧块螺钉时静脉丛出血和C2神经根刺激的问题。因此,寰椎椎弓根螺钉固定逐渐成为被广泛接受的治疗寰枢椎不稳的理想固定方式[21-24]。
尽管如此,寰椎后弓解剖学形态显著的个体差异对置入椎弓根螺钉有着严重影响。通常认为,椎弓根高度<4 mm的患者无法置入椎弓根螺钉[6-10]。随着手术技术的不断进步,虽然一些椎弓根高度<4 mm的病例可以通过使用不同直径的弹性骨锥逐级扩髓的方法将椎弓根钉道周围皮质扩张,成功置入椎弓根螺钉[25],然而,临床上经常会出现在扩髓或置钉过程中椎弓根壁破裂的现象,而椎弓根壁的破裂将直接导致螺钉稳定性明显下降以及椎动脉损伤的风险明显增加,最终无法使用椎弓根螺钉固定。在不增加暴露范围、不改变手术体位、不更换手术器械、不增加出血量的前提下,寻找理想的替代方法完成手术是亟需解决的问题。
笔者所在研究团队通过对寰椎后弓的解剖学特点分析发现,寰椎后弓至横突之间的髓腔长轴截面呈现“喇叭口”形态,即后方入钉点髓腔和前方靠近横突孔后内侧壁髓腔相对膨大,中段椎动脉沟狭窄处狭小。该髓腔结构的后方入钉点髓腔最大高度为(4.93±0.37) mm,男性与女性之间差异虽有统计学意义,但最小值仍接近4 mm。选择从该髓腔结构的后方入钉点以椎弓根内壁为轴,横突孔后内侧壁为导向进钉,虽然需要经过椎动脉沟狭窄处[男性(2.48±0.91) mm,女性(1.71±0.42) mm],但从较为宽大的进钉点向较为狭窄的椎动脉沟髓腔逐级扩张钉道,技术要求更为简单,操作更为容易,能够明显降低皮质破裂、螺钉穿出的风险。同时,该髓腔结构的长轴能容纳长度12~28 mm的螺钉,椎动脉沟狭窄处不作为螺钉固定的起始段,仅是螺钉走行过程中的一部分,螺钉全长能够咬合更多周围骨质,无论椎动脉沟狭窄处皮质是否出现破裂,螺钉头尾端周围均有完整骨皮质包绕,整体稳定性将不会受到影响。因此,从解剖学角度,寰椎后弓-横突髓腔可以作为椎弓根螺钉进钉点狭小无法置钉或钉道破裂置钉失败时的替代钉道。
应用此种置钉方式时需要注意:术前需对钉道长度进行测量,术中在用骨锥寻找髓腔逐渐靠近横突孔时,应注意前方手感的变化,避免突然落空失手突破横突孔后内侧壁,造成椎动脉损伤。根据本研究组已完成的临床病例的经验,在术前对患者寰椎CT影像进行测量和钉道路径规划,术中先用球磨钻将入钉点皮质打磨便于寻找髓腔,利用骨锥在后弓-横突髓腔起始相对膨大处进入髓腔,利用术前测量的钉道长度、角度作为限制并通过骨锥向横突扩髓探出钉道,交替使用探针感受松质骨髓腔和前方横突孔后内侧壁皮质的手感变化,以骨锥探入髓腔深度减少约2 mm作为置入螺钉长度,在术中操作时能够明显感受出松质骨髓腔和前方皮质骨的手感差异。本组术中未出现落空感或进入横突孔等情况,术后CT复查证实螺钉位置良好。因此,术前对CT影像仔细测量和规划并配合术中精细操作及对手感的良好控制,能够有效地避免侵入横突孔和损伤椎动脉。
本研究的局限和不足:①虽然为了尽量避免测量者主观因素影响,本研究采用2名脊柱外科医师和1名影像科医师重复测量同一参数并取平均值作为最后数据,但测量轴线的标定、截面的选择以及角度的确定需要观察者主观判断,难以完全避免误差;②本研究仅从解剖学角度对寰椎后弓-横突髓腔置钉的可行性进行了分析,结合有限病例初步证实了其可行性,尚缺少生物力学相关测试以及临床病例随访对其可靠性进行系统验证。
| [1] | Elliott RE, Tanweer O, Boah A, et al. Atlantoaxial fusion with screw-rod constructs:meta-analysis and review of literature[J]. World Neurosurg, 2014, 81(2): 411–421. DOI:10.1016/j.wneu.2012.03.013 |
| [2] | Yeom JS, Kafle D, Nguyen NQ, et al. Routine insertion of the lateral mass screw via the posterior arch for C1 fixation:feasibility and related complications[J]. Spine J, 2012, 12(6): 476–483. DOI:10.1016/j.spinee.2012.06.010 |
| [3] | Elliott RE, Tanweer O, Frempong-Boadu A, et al. Impact of starting point and C2 nerve status on the safety and accuracy of C1 lateral mass screws:meta-analysis and review of the literature[J]. J Spinal Disord Tech, 2015, 28(5): 171–185. DOI:10.1097/BSD.0b013e3182898aa9 |
| [4] | Elliott RE, Tanweer O, Smith ML, et al. Impact of starting point and bicortical purchase of C1 lateral mass screws on atlantoaxial fusion:meta-analysis and review of the literature[J]. J Spinal Disord Tech, 2015, 28(7): 242–253. DOI:10.1097/BSD.0b013e31828ffc97 |
| [5] | Ma C, Wu J, Zhao M, et al. Treatment of upper cervical spine instability with posterior fusion plus atlantoaxial pedicle screw[J]. Cell Biochem Biophys, 2014, 69(3): 693–697. DOI:10.1007/s12013-014-9854-2 |
| [6] | Tan M, Wang H, Wang Y, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass[J]. Spine(Phila Pa 1976), 2003, 28(9): 888–895. |
| [7] | Ma XY, Yin QS, Wu ZH, et al. Anatomic considerations for the pedicle screw placement in the first cervical vertebra[J]. Spine(Phila Pa 1976), 2005, 30(13): 1519–1523. DOI:10.1097/01.brs.0000168546.17788.49 |
| [8] | Lee MJ, Cassinelli E, Riew KD. The feasibility of inserting atlas lateral mass screws via the posterior arch[J]. Spine(Phila Pa 1976), 2006, 31(24): 2798–2801. DOI:10.1097/01.brs.0000245902.93084.12 |
| [9] | Christensen DM, Eastlack RK, Lynch JJ, et al. C1 anatomy and dimensions relative to lateral mass screw placement[J]. Spine(Phila Pa 1976), 2007, 32(8): 844–848. DOI:10.1097/01.brs.0000259833.02179.c0 |
| [10] | Lin JM, Hipp JA, Reitman CA. C1 lateral mass screw placement via the posterior arch:a technique comparison and anatomic analysis[J]. Spine J, 2013, 13(11): 1549–1555. DOI:10.1016/j.spinee.2013.06.006 |
| [11] | Melcher RP, Puttlitz CM, Kleinstueck FS, et al. Biomechanical testing of posterior atlantoaxial fixation techniques[J]. Spine(Phila Pa 1976), 2002, 27(22): 2435–2340. DOI:10.1097/00007632-200211150-00004 |
| [12] | Hott JS, Lynch JJ, Chamberlain RH, et al. Biomechanical comparison of C1-2 posterior fixation techniques[J]. J Neurosurg Spine, 2005, 2(2): 175–181. DOI:10.3171/spi.2005.2.2.0175 |
| [13] | Jeon SW, Jeong JH, Choi GH, et al. Clinical outcome of posterior fixation of the C1 lateral mass and C2 pedicle by polyaxial screw and rod[J]. Clin Neurol Neurosurg, 2012, 114(6): 539–544. DOI:10.1016/j.clineuro.2011.11.001 |
| [14] | Jin GX, Wang H, Li L, et al. C1 posterior arch crossing screw fixation for atlantoaxial joint instability[J]. Spine (Phila Pa 1976), 2013, 38(22): E1397–1404. DOI:10.1097/BRS.0b013e3182a40869 |
| [15] | Elliott RE, Tanweer O, Boah A, et al. Outcome comparison of atlantoaxial fusion with transarticular screws and screw-rod constructs:meta-analysis and review of literature[J]. J Spinal Disord Tech, 2014, 27(1): 11–28. DOI:10.1097/BSD.0b013e318277da19 |
| [16] | Zheng Y, Hao D, Wang B, et al. Clinical outcome of posterior C1-C2 pedicle screw fixation and fusion for atlantoaxial instability:a retrospective study of 86 patients[J]. J Clin Neurosci, 2016, 32: 47–50. DOI:10.1016/j.jocn.2015.12.045 |
| [17] | Jacobson ME, Khan SN, An HS. C1-C2 posterior fixation:indications, technique, and results[J]. Orthop Clin North Am, 2012, 43(1): 11–18. DOI:10.1016/j.ocl.2011.09.004 |
| [18] | Ni B, Zhou F, Guo Q, et al. Modified technique for C1-2 screw-rod fixation and fusion using autogenous bicortical iliac crest graft[J]. Eur Spine J, 2012, 21(1): 156–164. DOI:10.1007/s00586-011-1958-4 |
| [19] | Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation[J]. Spine(Phila Pa 1976), 2001, 26(22): 2467–2471. DOI:10.1097/00007632-200111150-00014 |
| [20] | Resnick DK, Benzel EC. C1-C2 pedicle screw fixation with rigid cantilever beam construct:case report and technical note[J]. Neurosurgery, 2002, 50(2): 426–428. |
| [21] | Ma XY, Yin QS, Wu ZH, et al. C1 pedicle screws versus C1 lateral mass screws:comparisons of pullout strengths and biomechanical stabilities[J]. Spine(Phila Pa 1976), 2009, 34(4): 371–377. DOI:10.1097/BRS.0b013e318193a21b |
| [22] | Zarro CM, Ludwig SC, Hsieh AH, et al. Biomechanical comparison of the pullout strengths of C1 lateral mass screws and C1 posterior arch screws[J]. Spine J, 2013, 13(12): 1892–1896. DOI:10.1016/j.spinee.2013.06.015 |
| [23] | Fensky F, Kueny RA, Sellenschloh K, et al. Biomechanical advantage of C1 pedicle screws over C1 lateral mass screws:a cadaveric study[J]. Eur Spine J, 2014, 23(4): 724–731. DOI:10.1007/s00586-013-3143-4 |
| [24] | Du JY, Aichmair A, Kueper J, et al. Biomechanical analysis of screw constructs for atlantoaxial fixation in cadavers:a systematic review and meta-analysis[J]. J Neurosurg Spine, 2015, 22(2): 151–161. DOI:10.3171/2014.10.SPINE13805 |
| [25] | Huang DG, He SM, Pan JW, et al. Is the 4 mm height of the vertebral artery groove really a limitation of C1 pedicle screw insertion?[J]. Eur Spine J, 2014, 23(5): 1109–1114. DOI:10.1007/s00586-014-3217-y |
 2018, Vol.16
2018, Vol.16  Issue(2): 92-97
Issue(2): 92-97


