2. 海军总医院放射科, 北京 100048;
3. 海军总医院计算机管理中心, 北京 100048;
4. 海军总医院耳鼻喉科, 北京 100048
2. Department of Radiology, Navy General Hospital, Beijing 100048;
3. Department of Computer Management Center, Navy General Hospital, Beijing 100048;
4. Department of Otorhinolaryngology, Navy General Hospital, Beijing 100048
颈椎前路手术时,如有颈椎节段的准确体表标志帮助确定切口部位,可避免不必要的延长切口,有助于手术野理想显露和操作,切口美观[1]。颈椎节段的体表标志有多种,如舌骨、环状软骨、甲状软骨、颈动脉结节等[2],但都只是大致定位,并不精准。近年有报道下颌角(MDA)恒定指向C2/C3椎间隙,且不因性别、颈部屈伸而变化,提出MDA可作为颈椎节段的准确体表标志[3]。也有报道指出颈部屈伸变化时83.3%的病例MDA相对C2上下移动≤ 1个椎体[4]。本研究对57例男性及66例女性颈椎的影像学资料进行测量,以核实上述观点的可信性。
1 材料和方法 1.1 一般资料2014年2月—2017年1月,选取在本院行颈椎正侧、双斜、过伸过屈位数字摄影(DR)检查且排除骨性畸形的123例患者的影像学资料。其中,男57例,年龄12~84(45.9±15.0)岁;女66例,年龄21~81(49.0±15.4)岁。男女间年龄差异无统计学意义,具有可比性。选取站立标准侧位(中立位)、过伸及过屈位DR图像进行测量。
1.2 摄片要求中立位:站立右侧位,上下齿咬合,右肩紧靠影像接收器,颈椎正中矢状面平行于接收器,瞳间线垂直于接收器,双眼平视正前方,头、颈和躯干正中矢状面重合。源像距100~120 cm,照射野含全部颈椎及下颌骨。曝光条件65~75 kV,自动曝光控制。摄片时患者呼气后摒气,肩部向下放松,以助显露C7。过伸、过屈位侧立同前,自然用力头颈屈、伸至极限位摄片。
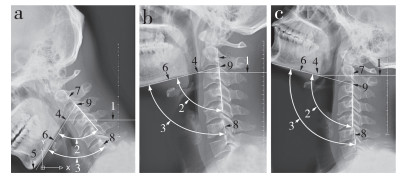
1.3 图像处理原始图像在工作屏幕上观察,照射野含全部颈椎及下颌骨者以dicom格式存盘。测量前在Image Viewer软件中打开,选择目标区域,另存为jpg格式(图 1) [5]。将jpg图像以光栅图像在AutoCAD 2007中打开。标记MDA,经MDA下缘画MDA的水平线,上颈椎角(AUCS),全颈椎角(ACS),C2椎体后缘线,C6椎体后缘线,颏隆突底,连接MDA下缘与颏隆突下界的下颌底线[6](图 2)。
|
1,缩略图;2,选中图片 1, sketch images; 2, selected image 图 1 在ImageViewer中打开源图像 Figure 1 Raw images opened at ImageViewer interface |
|
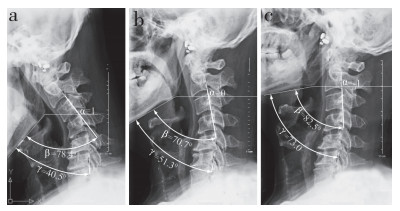
a:过屈 b:中立 c:过伸 1,MDA水平线;2,AUCS;3,ACS;4,MDA;5,颏隆突底;6,下颌底线;7,C2椎体后缘线;8,C6椎体后缘线;9,AUCS即时旋转中心 a: Hyperflexion b: Neutral c: Hyperextension 1, horizontal line passing through MDA; 2, AUCS; 3, ACS; 4, MDA; 5, base of mental protuberance; 6, inferior edge of mandible; 7, posterior edge of C2 vertebral body; 8, posterior edge of C6 vertebral body; 9, instantaneous rotation center of AUCS 图 2 在AutoCAD中打开颈椎侧位DR图像 Figure 2 Lateral DR images of cervical spine opened at AutoCAD interface |
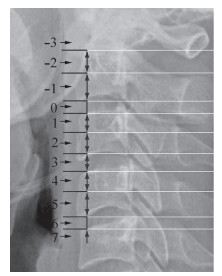
半定量测量过屈位、中立位、过伸位下MDA与颈椎节段的对应关系。以MDA水平线与椎体前缘的交叉点为依据,将颈椎节段数字化,0代表C2/C3椎间隙,每往上1/2个椎体或1个椎间隙则减1,反之则加1(图 3)。
|
图 3 颈椎节段及其对应值 Figure 3 Cervical spinal level and its assigned number |
测量不同体位下AUCS及ACS角度。AUCS即下颌底线与C2椎体后缘的夹角;ACS即下颌底线与C6椎体后缘的夹角(因为部分C7椎体显示不清,难以测得下颌底线与C7椎体后缘夹角)。利用AutoCAD 2007标注菜单中的“角度测量”功能,精度为0.1°(图 4)。

|
a:过屈 b:中立 c:过伸 α,MDA水平线;β,AUCS;γ,ACS a: Hyperflexion b: Neutral c: Hyperextension α, horizontal line passing through MDA; β, AUCS; γ, ACS 图 4 利用AutoCAD 2007完成数据测量 Figure 4 Data measurement based on AutoCAD 2007 interface |
采用SPSS 21.0软件对数据进行统计学分析。不同性别间MDA对应的颈椎节段比较采用2个独立样本t检验,不同体位下MDA对应的颈椎节段比较采用多个相关样本t检验。AUCS及ACS在性别间比较采用独立样本t检验;不同体位下AUCS及ACS比较采用随机单位组设计资料的方差分析,AUCS与ACS的比较采用配对t检验。数据采用x±s表示,以P<0.05为差异有统计意义。
2 结果 2.1 MDA对应的颈椎节段不同体位下MDA对应的颈椎节段见表 1。中立位时,女性MDA可对应范围为C2椎体上部至C3/C4椎间隙,男性为C2椎体下部至C3/C4椎间隙,中位数波动于C2/C3椎间隙及C3椎体上部(表 1)。从过屈位到中立位(男98.2%,女95.5%)、中立位到过伸位(男93.0%,女92.4%)及过屈位到过伸位(男45.6%,女50.0%)大部分MDA上下移动≤ 1个椎体。1例男性和7例女性过屈位时MDA平行C2椎体下部(图 5);4例男性和5例女性过伸位时MDA低于C2/C3椎间隙(图 6);统计结果见表 2。不同性别间比较,过屈位及中立位MDA对应的颈椎节段差异无统计学意义(P>0.05);过伸位时女性MDA对应的颈椎节段高于男性,差异有统计学意义(P<0.05)。MDA对应的颈椎节段在过屈位最低,随着向中立位及过伸位变化,MDA对应的颈椎节段逐渐升高。
|
|
表 1 不同体位下MDA对应的颈椎节段例数 Table 1 Samples of corresponding cervical spine level parallel to MDA at different postures |
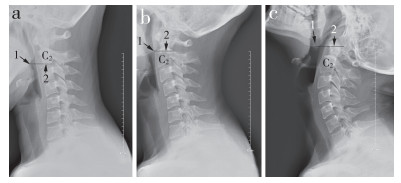
|
a:过屈 b:中立 c:过伸 1,MDA;2,MDA水平线 a: Hyperflexion b: Neutral c: Hyperextension 1, MDA; 2, horizontal line passing through MDA 图 5 过屈位时MDA平行于C2椎体上部 Figure 5 MDA is parallel to inferior portion of C2 at hyperflexion posture |

|
a:过屈 b:中立 c:过伸 1,MDA;2,MDA水平线 a: Hyperflexion b: Neutral c: Hyperextension 1, MDA; 2, horizontal line passing through MDA 图 6 过伸位时MDA仍低于C2/C3水平 Figure 6 MDA is lower than C2/C3 level at hyperextension posture |
|
|
表 2 不同体位下MDA对应的颈椎水平 Table 2 MDA and corresponding cervical spinal level at different postures |
同体位下,AUCS及ACS各自在不同性别间比较差异均无统计学意义(P>0.05);同性别同体位下,AUCS与ACS间比较差异有统计学意义(P<0.05);同性别下,AUCS及ACS各自在不同体位下比较差异有统计学意义(P<0.05),结果见表 3。过屈位向中立位及过伸位变换过程中,AUCS及ACS的角度变化见表 4。AUCS总的变化趋势和ACS一样,逐渐增大,但个别病例减小(图 7)。过屈位到中立位时AUCS及ACS的平均角度变化均小于中立位到过伸位的角度变化。颈椎体位变化时,AUCS的角度变化不及ACS角度变化的一半,且不同体位间变换时占比不一(表 5)。
|
|
表 3 不同体位下角度测量 Table 3 Angle measurement at different postures |
|
|
表 4 不同体位下角度变化 Table 4 Angle change range when posture changed |
|
a:过屈 b:中立 c:过伸 α,MDA水平线;β,AUCS;γ,ACS a: Hyperflexion b: Neutral c: Hyperextension α, horizontal line passing through MDA; β, AUCS; γ, ACS 图 7 中立位时AUCS角度较过屈位时减小 Figure 7 AUCS decreased when posture of neck changed to neutralization from hyperflexion posture |
|
|
表 5 不同体位变化中AUCS变化占ACS变化的比率 Table 5 Ratio of AUCS to ACS when posture changed |
普遍认为,颈椎前方的体表解剖标志多属大致判定[1-2]。环状软骨、甲状软骨及下颌骨下界等在颈部屈伸时位置会变化[1]。C6横突为颈动脉结节,位置恒定但深在,依靠术前透视及触摸颈动脉结节定位亦可能出现偏差[1]。根据颈动脉结节定位C6椎体及其紧邻的上下椎间隙准确性尚可,但如手术节段距C6较远,仍可能出现偏差;这是颈椎曲度多样性及解剖变异等的缘故,与术者经验亦有关。术前透视定位,受透视角度与切口方向的影响,到达椎体前缘时亦可能出现偏差。Liu等[3]解剖6例男性和4例女性尸体,报道MDA恒定对应C2/C3椎间隙,且不受颈部屈伸变化的干扰。亦有报道称MDA随颈椎屈伸可有上下≤ 1个椎体的变化[4]。本研究结果显示上述结论可信性欠佳,MDA不能作为准确判定颈椎节段的恒定体表标志。
3.2 MDA不能作为准确定位颈椎节段的恒定体表标志本研究结果显示,中立位时,女性MDA可对应范围为C2椎体上部至C3/C4椎间隙,男性为C2椎体下部至C3/C4椎间隙,中位数波动于C2/C3椎间隙及C3椎体上部。中立位向过屈位变换时,男性MDA对应的颈椎节段会下降1.0~1.5个椎体高度,女性下降0~2.0个椎体高度;中立位向过伸位变换时,男性及女性均上升0~1.5个椎体高度。分析其机制如下。
中立位时MDA对应的颈椎节段波动来自个体差异,由于大多MDA对应C2/C3椎间隙或C3椎体上部,观察例数少时,MDA偏上或下的情形不易被捕捉到,可能造成MDA恒定对应C2/C3椎间隙的错觉。Liu等[3]仅观察了10例尸体标本,可能出现偏倚。
ACS由AUCS与C2~6成角共同形成。C2~6成角是4个椎间隙夹角的叠加[7]。颈椎屈伸时决定MDA位置的是MDA围绕AUCS旋转中心发生的角度变化。如MDA紧邻C2/C3椎间隙前缘,AUCS与MDA旋转中心重合,二者旋转半径相等,MDA与颈椎节段的对应关系则较为恒定。但实际上MDA与AUCS的旋转中心不重合,旋转半径亦不等,过屈位时MDA靠近颈椎前缘,过伸位时远离,旋转中心在变动(图 2),且屈伸伴位移变化[8],MDA很难维持与C2/C3椎间隙的对应位置(图 2)。屈伸活动后颈椎中立位置也可能变化[9],有颈部疾病的患者经过治疗后颈椎屈伸范围也可能变化[10],因此MDA对应的颈椎节段还可能变化。
Auerbach等[2]报道,用MDA判定颈椎节段比触摸颈动脉结节准确,且术前标准侧位与术中仰卧侧位时MDA对应的颈椎节段吻合。本研究未行该方面对比研究,在理论上分析,MDA与颈椎节段的对应关系随颈椎屈伸而变化,只有当站立标准侧位时与仰卧侧位时的头颈位置完全一致,MDA对应的颈椎节段才会吻合。为求术前定位尽量准确,本研究组建议在麻醉完毕、体位不再变动时先行透视定位(铺单完毕透视最佳),确定切口部位;手术暴露到椎体前缘插入定位针后再次透视核实,方可确保定位无误。
张口时旋转中心与AUCS旋转中心又不一致,MDA位置变动又趋复杂,颏隆突下降亦影响术野(图 8),因此本研究组建议术中经鼻插管麻醉,否则需将头部向一侧旋转,会影响侧方减压范围的判定[11]。

|
a:过屈闭口 b:中立张口 c:过伸闭口 α,MDA水平线;β,AUCS;γ,ACS;δ,张口角度 a: Hyperflexion with mouth closed b: Neutral with mouth opened c: Hyperextension with mouth closed α, horizontal line passing through MDA; β, AUCS; γ, ACS; δ, angle formed by opened mouth 图 8 张口导致MDA位置下降 Figure 8 Opened mouth led to MDA location descended |
专业书籍指出颈椎屈伸主要发生在寰枕关节,旋转主要发生于寰枢关节。后者为临床所证实[11],前者说法受到质疑。Park等[12]报道,颈椎屈伸时AUCS与C2~7节段的活动范围并无区别。Wang等[13]报道,颈椎屈伸时上下颈椎各自角度变化并不同步,ACS增加时,部分病例AUCS反减小。本研究发现颈椎体位变换时,AUCS角度变化只占ACS变化的23.5%~41.7%,不同体位间变换占比不一,提示颈椎屈伸并不主要发生在寰枕关节;从中立位到过伸位时AUCS角度变化占比加大,也提示AUCS与ACS角度变化不同步。同样,部分病例在ACS由屈向伸转变时,AUCS角反而减小,需C2~6成角加大补偿,显示出颈椎运动的复杂性(图 7)。
4 结论颈椎中立时,MDA并非恒定对应于C2/C3椎间隙,而是在C2椎体上部与C3/C4椎间隙间波动。颈椎屈伸时,MDA与颈椎节段的对应关系会发生波动,且不一定局限于1个椎体高度。颈椎屈伸运动并非主要发生在上颈椎。颈椎中立位并非颈椎屈伸运动的中点。综上所述,MDA不能作为颈椎体表定位的恒定参考。
| [1] | Lee JH, Lee JH, Lee HS, et al. The efficacy of carotid tubercle as an anatomical landmark for identification of cervical spinal level in the anterior cervical surgery:comparison with preoperative C-arm fluoroscopy[J]. Clin Orthop Surg, 2013, 5(2): 129–133. DOI:10.4055/cios.2013.5.2.129 |
| [2] | Auerbach JD, Weidner Z, Pill SG, et al. The mandibular angle as a landmark for identification of cervical spinal level[J]. Spine(Phila Pa 1976), 2009, 34(10): 1006–1011. DOI:10.1097/BRS.0b013e31819f2a03 |
| [3] | Liu WM, Chen Q, Liang Y, et al. Surgical landmark of mandible angle in the identification of cervical spinal level[J]. J Craniofac Surg, 2017, 28(6): 1582–1585. DOI:10.1097/SCS.0000000000003703 |
| [4] | Liu JM, Du LX, Xiong X, et al. Radiographic evaluation of the reliability of neck anatomic structures as anterior cervical surgical landmarks[J]. World Neurosurg, 2017, 103: 133–137. DOI:10.1016/j.wneu.2017.03.129 |
| [5] | 侯黎升, 白雪东, 葛丰, 等. 下颈椎椎弓根前入口及前半四壁皮质厚度的影像学测量及应用分析[J]. 第二军医大学学报, 2017, 38(9): 1152–1157. |
| [6] | Zhang J, Lin W, Chi Y, et al. The error analysis of lobular and segmental division of right liver by volume measurement[J]. Clin Anat, 2017, 30(5): 585–590. DOI:10.1002/ca.v30.5 |
| [7] | Yu Y, Mao H, Li JS, et al. Ranges of cervical intervertebral disc deformation during an in vivo dynamic flexionextension of the neck[J]. J Biomech Eng, 2017, 139(6): 10.1115/1.4036311. |
| [8] | Marinković S, Milić I, Djorić I, et al. Morphometric multislice computed tomography examination of the craniovertebral junction in neck flexion and extension[J]. Folia Morpho(l Warsz), 2017, 76(1): 100–109. DOI:10.5603/FM.a2016.0037 |
| [9] | Wang X, Lindstroem R, Carstens NP, et al. Cervical spine reposition errors after cervical flexion and extension[J]. BMC Musculoskelet Disord, 2017, 18(1): 102. DOI:10.1186/s12891-017-1454-z |
| [10] | Moustafa IM, Diab AAM, Hegazy FA, et al. Does rehabilitation of cervical lordosis influence sagittal cervical spine flexion extension kinematics in cervical spondylotic radiculopathy subjects?[J]. J Back Musculoskelet Rehabil, 2017, 30(4): 937–941. DOI:10.3233/BMR-150464 |
| [11] | Russo A, Albanese E, Quiroga M, et al. Submandibular approach to the C2-3 disc level:microsurgical anatomy with clinical application[J]. J Neurosurg Spine, 2009, 10(4): 380–389. DOI:10.3171/2008.12.SPINE08281 |
| [12] | Park MS, Moon SH, Lee HM, et al. Age-related changes in cervical sagittal range of motion and alignment[J]. Global Spine J, 2014, 4(3): 151–156. DOI:10.1055/s-0034-1378140 |
| [13] | Wang X, Lindstroem R, Plocharski M, et al. Cervical flexion and extension includes anti-directional cervical joint motion in healthy adults[J]. Spine J, 2018, 18(1): 147–154. DOI:10.1016/j.spinee.2017.07.170 |
 2018, Vol.16
2018, Vol.16  Issue(2): 103-108
Issue(2): 103-108


