2. 上海市静安区闸北中心医院骨科, 上海 200070
2. Department of Orthopaedics, Jing'an District Zhabei Central Hospital, Shanghai 200070, China
青少年特发性脊柱侧凸(AIS)包括冠状面弯曲,矢状面胸、腰椎后凸或前凸不足以及水平面椎体旋转的三维脊柱畸形。随着内固定器械的发展和手术技术的进步,多数AIS患者可以获得良好的冠状面及矢状面畸形矫正。近年来,椎体旋转在畸形进展、术后矫形效果丢失以及腰背部隆起残留中的作用备受重视[1-2],理想的椎体去旋转可以获得更好的临床疗效。和万向椎弓根螺钉相比,单平面椎弓根螺钉头端仅在矢状面活动,理论上可获得更好的去旋转效果[3-5]。本研究对应用万向椎弓根螺钉和单平面椎弓根螺钉行后路三维矫形植骨融合内固定术的Lenke 5型AIS患者的临床资料进行回顾性研究,比较2种螺钉的顶椎去旋转效果。
1 资料与方法 1.1 一般资料纳入标准:①10 ~ 20岁Lenke 5型AIS;②腰椎侧凸Cobb角45° ~ 70°;③行单一后路胸腰椎三维矫形植骨融合内固定术;④术前、术后2周及术后1年有完整的站立位全脊柱正位X线片;⑤万向螺钉或单平面椎弓根螺钉使用比例 > 80%。2010年1月—2013年12月,根据以上标准共纳入患者72例,其中使用万向椎弓根螺钉治疗(A组)43例,使用单平面椎弓根螺钉治疗(B组)29例。A组男6例,女37例,年龄(14.8±2.1)岁,固定融合节段(7.6±1.3)个;B组男4例,女25例,年龄(15.1±2.0)岁,固定融合节段(7.8±1.1)个。
1.2 手术方法所有患者均在全麻下行后路三维矫形植骨融合内固定术,内固定器械为山东威高Upass系统或美国强生Expedium系统。椎弓根螺钉均为徒手置入,术中采用旋棒、平移、去旋转及原位弯棒等矫形技术,同种异体骨和咬碎自体骨混合后作为植骨材料。手术全程在体感诱发电位(sSEP)和运动诱发电位(MEP)监护下完成。
1.3 评价指标术前、术后2周首次站立时及术后1年拍摄站立位全脊柱正位X线片,分别测量腰椎侧凸Cobb角及腰椎前凸角。术前使用Nash-Moe法[6]评估顶椎旋转程度:Ⅰ级,双侧椎弓根对称、椎体无旋转;Ⅱ级,凸侧椎弓根开始向椎体中线偏移,凹侧椎弓根与椎体凹侧缘重叠;Ⅲ级,凸侧椎弓根移至椎体中线与凸侧缘之间2/3处,凹侧椎弓根正在消失;Ⅳ级,凸侧椎弓根移至椎体中线处,凹侧椎弓根完全消失;Ⅴ级,凸侧椎弓根移位超过椎体中线,凹侧椎弓根完全消失。术后采用Upasani等[1]提出的正位X线片上椎弓根螺钉和连接棒的位置来评估顶椎去旋转程度:0级,双侧椎弓根螺钉的尖部位于两连接棒的内侧,椎体旋转 > 0且 < 9°;1级,一侧椎弓根螺钉的尖部被同侧连接棒遮挡,椎体旋转≥9°且 < 13°;2级,一侧椎弓根螺钉的尖部在同侧连接棒的外侧,椎体旋转≥13°。
1.4 统计学处理采用SPSS 13.0软件对数据进行统计学分析。计量资料采用χ2分析,计数资料采用t检验,以P < 0.05为差异有统计学意义。
2 结果所有患者均顺利完成手术。2组患者术前腰椎侧凸Cobb角及腰椎前凸角差异无统计学意义(P > 0.05,表 1);2组术后2周及1年腰椎侧凸Cobb角及腰椎前凸角均较术前显著改善,差异有统计学意义(P < 0.05,表 1);A组术后1年腰椎侧凸矫正率为79.2%,B组为81.4%,差异无统计学意义(P > 0.05)。2组患者术前顶椎旋转程度差异无统计学意义(P > 0.05);术后2周及1年顶椎去旋转程度B组优于A组,差异有统计学意义(P < 0.05,表 2)。
|
|
表 1 手术前后腰椎侧凸Cobb角及前凸角 Table 1 Lumbar scoliosis Cobb's angle and lordosis angle at pre- and post-operation |
|
|
表 2 术前顶椎旋转Nash-Moe分级及术后顶椎去旋转程度 Table 2 Preoperative Nash-Moe grade and postoperative derotation degree of apical vertebra |
|
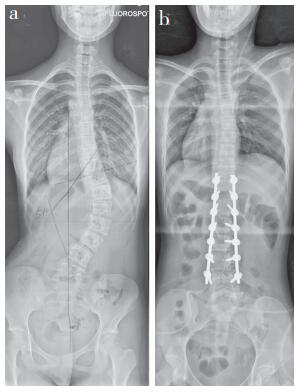
a:术前全脊柱正位X线片示Cobb角51°,Nash-Moe顶椎(L1)旋转Ⅳ级 b:术后1年站立位全脊柱X线片示顶椎(L1)去旋转程度为0级 a:Preoperative entire spine anteroposterior roentgenograph shows Cobb's angle is 51° with apical vertebra(L1) rotation Nash-Moe grade Ⅳ b:Entire spine anteroposterior roentgenograph at postoperative 1 year shows derotation of apical vertebra(L1) is grade 0 图 1 使用单平面椎弓根螺钉病例影像学资料 Figure 1 Radiologic data of a typical case using uniplanar pedicle screw |

|
a:术前全脊柱正位X线片示Cobb角47°,Nash-Moe顶椎(L2)旋转Ⅳ级 b:术后2周首次站立位全脊柱X线片示顶椎(L2)旋转1级c:术后1年全脊柱X线片示顶椎(L2)旋转2级 a:Preoperative entire spine anteroposterior roentgenograph shows Cobb's angle is 47° with apical vertebra(L2) rotation Nash-Moe grade Ⅳ b:Entire spine anteroposterior roentgenograph at postoperative 2 weeks shows derotation of apical vertebra(L2) is grade 1 c:Entire spine anteroposterior roentgenograph at postoperative 1 year shows derotation of apical vertebra(L2) is grade 2 图 2 使用万向椎弓根螺钉病例影像学资料 Figure 2 Radiologic data of a typical case using multiaxial pedicle screw |
AIS是一种三维空间畸形,而椎体旋转是最基本的一种畸形形态。椎体旋转程度越大,Cobb角、剃刀背等外观畸形越大,心血管系统及肺功能不全的发生率也会增加,并且椎体的旋转程度也被视为侧凸进展的危险因素[7-8]。因此,有效的去旋转治疗十分必要[9-11]。另有研究表明,有效的去旋转矫形可以减少需要融合的节段,从而保留患者的运动功能,减少长节段固定带来的出血、神经损伤等并发症;尤其对于腰椎侧凸的患者,可以最大程度保留其弯腰功能[12]。Tredwell等[13]和Cui等[14]研究发现,脊柱侧凸术后残留的椎体旋转角度越多,其术后远期发生并发症(如矫正效果丢失、邻近融合节段退行性变及曲轴效应)的可能性越大。故寻找一种既可以最大程度去旋转矫形又可以维持术后远期椎体去旋转效果的内固定器械势在必行。
目前广泛用于AIS矫形的椎弓根螺钉根据其尾端的活动程度分为3类:单轴椎弓根螺钉、单平面椎弓根螺钉以及万向椎弓根螺钉。前期许多研究表明,使用单平面椎弓根螺钉以及单轴椎弓根螺钉在椎体去旋转方面更有优势,Kuklo等[15]、Asghar等[16]和Kadoury等[17]研究了单轴椎弓根螺钉对于旋转椎的矫正效果,发现其矫正率均较高,分别为77.9%、60%以及74%。Kuklo等[15]通过评价采用单轴及万向椎弓根螺钉的胸椎去旋转效果的相关参数发现,单轴椎弓根螺钉去旋转效果更佳。Aliasgar等[16]发现在Lenke 1型AIS患者术后6周时,单平面椎弓根螺钉组顶椎旋转程度≤1级的患者占86%,而万向椎弓根螺钉组仅为49%。本研究对比了采用单平面椎弓根螺钉和万向椎弓根螺钉治疗的患者术后1年顶椎去旋转效果,发现单平面椎弓根螺钉组79.3%的患者顶椎旋转程度≤1级,而万向椎弓根螺钉组仅有41.8%的患者顶椎旋转程度≤1级,结果与上述研究一致。笔者猜测,单轴/平面椎弓根螺钉与万向椎弓根螺钉相比,可以更直接地将矫形力传导至椎体,从而达到更有效的去旋转作用。对于单轴椎弓根螺钉和单平面椎弓根螺钉,笔者推荐选择单平面椎弓根螺钉,这是由于在去旋转效果相同的前提下,单平面椎弓根螺钉具有可以在单平面活动的钉尾,降低了术者上棒的难度,从而使螺钉与棒更加贴合。Liu等[18]和Wang等[19]比较了3种不同螺钉在矫形过程中的生物力学差异,发现单轴椎弓根螺钉在椎骨与螺钉平面之间的应力载荷比单平面椎弓根螺钉高11% ~ 13%,更容易发生该平面的损伤、螺钉松动、拔出以及断钉断棒等并发症。因此,单平面椎弓根螺钉在矫形及椎体去旋转方面更具优势。
Nash-Moe法因其操作简便,常被用于评估AIS患者术前椎体旋转程度,但术后由于内固定的阻挡,骨性标志被遮盖,很难在X线片上采用其对椎体进行评估[20]。Asghar等[16]和Dalal等[21]提出的CT测量法增加了患者的辐射量,且仰卧位时侧凸形态与站立位有一定差异,因此寻找更加实用的评估替代方法十分必要。Upasani等[1]提出了一种通过X线片判断椎体旋转情况的方法,该方法通过评价术后内固定螺钉与连接棒的相对位置来判断椎体旋转程度。作者将该方法与CT评估结果相比较,发现二者具有高度一致性(r=0.98),二者对于椎体旋转角度的评估仅相差1.9°±2.0°,认为该方法可以替代CT评估术后椎体旋转程度。
虽然本研究的结论有前人的研究作为依据,但仍然存在一些不足。首先,本研究为回顾性研究,样本的同质性以及对照的选择存在一定的局限性,一定程度上会影响结果的信度及效度;其次,本研究样本量有限,一定程度上会影响结果的准确性;最后,本研究采用的术后椎体旋转评价方式并未得到广泛应用,也会使得结果有一定偏差。
4 结论单平面及万向椎弓根螺钉均可有效矫正Lenke 5型AIS患者冠状位失平衡并保持腰椎前凸,使用单平面椎弓根螺钉可更加有效地矫正顶椎的旋转畸形并维持其去旋转效果,从而使患者术后获得满意的外观,降低侧凸的远期复发率。
| [1] | Upasani VV, Chambers RC, Dalal AH, et al. Grading apical vertebral rotation without a computed tomography scan:a clinically relevant system based on the radiographic appearance of bilateral pedicle screws[J]. Spine(Phila Pa 1976), 2009, 34(17): 1855–1862. DOI:10.1097/BRS.0b013e3181abf797 |
| [2] | Kim YJ, Lenke LG, Cho SK, et al. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis[J]. Spine (Phila Pa 1976), 2004, 29(18): 2040–2048. DOI:10.1097/01.brs.0000138268.12324.1a |
| [3] | Lykissas MG, Jain VV, Nathan ST, et al. Mid-to longterm outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion:a meta-analysis[J]. Spine(Phila Pa 1976), 2013, 38(2): E113–E119. DOI:10.1097/BRS.0b013e31827ae3d0 |
| [4] | Akçali O, Alici E, Koşay C. Apical instrumentation alters the rotational correction in adolescent idiopath scoliosis[J]. Eur spine J, 2003, 12(2): 124–129. |
| [5] | Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis[J]. Spine(Phila Pa 1976), 2006, 31(3): 291–298. DOI:10.1097/01.brs.0000197865.20803.d4 |
| [6] | Nash CL Jr, Moe JH. A study of vertebral rotation[J]. J Bone Joint Surg Am, 1969, 51(2): 223–229. DOI:10.2106/00004623-196951020-00002 |
| [7] | Aronsson DD, Stokes IA, Ronchetti PJ, et al. Surgical correction of vertebral axial rotation in adolescent idiopathic scoliosis:prediction by lateral bending films[J]. J Spinal Disord, 1996, 9(3): 214–219. |
| [8] | Behensky H, Cole AA, Freeman BJ, et al. Fixed lumbar apical vertebral rotation predicts spinal decompensation in Lenke type 3C adolescent idiopathic scoliosis after selective posterior thoracic correction and fusion[J]. Eur Spine J, 2007, 16(10): 1570–1578. DOI:10.1007/s00586-007-0397-8 |
| [9] | Takahashi S, Suzuki N, Asazuma T, et al. Factors of thoracic cage deformity that affect pulmonary function in adolescent idiopathic thoracic scoliosis[J]. Spine(Phila Pa 1976), 2007, 32(1): 106–112. DOI:10.1097/01.brs.0000251005.31255.25 |
| [10] | Cimić M, Kovac V, Smiljanić I, et al. Relationship between clinical contourometric measurements and vertebral rotation in adolescent idiopathic scoliosis[J]. Coll Antropol, 2009, 33(Suppl 2): 127–133. |
| [11] | Soultanis K, Pyrovolou N, Karamitros A, et al. The use of thoracoplasty in the surgical treatment of idiopathic scoliosis[J]. Stud Health Technol Inform, 2006, 123: 327–333. |
| [12] | Suk SI, Lee SM, Chung ER, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis[J]. Spine(Phila Pa 1976), 2003, 28(5): 484–491. |
| [13] | Tredwell SJ, Sawatzky BJ, Hughes BL, et al. Rotations of a helix as a model for correction of the scoliotic spine[J]. Spine(Phila Pa 1976), 1999, 24(12): 1223–1227. DOI:10.1097/00007632-199906150-00009 |
| [14] | Cui G, Watanabe K, Nishiwaki Y, et al. Loss of apical vertebral derotation in adolescent idiopathic scoliosis:2-year follow-up using multi-planar reconstruction computed tomography[J]. Eur Spine J, 2012, 21(6): 1111–1120. DOI:10.1007/s00586-012-2274-3 |
| [15] | Kuklo TR, Potter BK, Polly DW Jr, et al. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis[J]. Spine(Phila Pa 1976), 2005, 30(18): 2113–2120. DOI:10.1097/01.brs.0000179260.73267.f4 |
| [16] | Asghar J, Samdani AF, Pahys JM, et al. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis. A comparison of an all pedicle screw construct versus a hook-rod system[J]. Spine(Phila Pa 1976), 2009, 34(8): 804–807. DOI:10.1097/BRS.0b013e3181996c1b |
| [17] | Kadoury S, Cheriet F, Beauséjour M, et al. A threedimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis[J]. Eur Spine J, 2009, 18(1): 23–37. DOI:10.1007/s00586-008-0817-4 |
| [18] | Liu PY, Lai PL, Lin CL. A biomechanical investigation of different screw head designs for vertebral derotation in scoliosis surgery[J]. Spine J, 2017, 17(8): 1171–1179. DOI:10.1016/j.spinee.2017.04.010 |
| [19] | Wang X, Aubin CE, Crandall D, et al. Biomechanical analysis of 4 types of pedicle screws for scoliotic spine instrumentation[J]. Spine(Phila Pa 1976), 2012, 37(14): E823–E835. DOI:10.1097/BRS.0b013e31824b7154 |
| [20] | Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation:does higher implant density improve correction?[J]. Spine(Phila Pa 1976), 2010, 35(5): 562–567. DOI:10.1097/BRS.0b013e3181b4af34 |
| [21] | Dalal A, Upasani VV, Bastrom TP, et al. Apical vertebral rotation in adolescent idiopathic scoliosis comparison of uniplanar and polyaxial pedicle screws[J]. J Spinal Disord Tech, 2011, 24(4): 251–257. DOI:10.1097/BSD.0b013e3181edebc4 |
 2018, Vol.16
2018, Vol.16  Issue(6): 327-330, 336
Issue(6): 327-330, 336


