胸腰椎爆裂性骨折主要表现为脊柱前中柱损伤,常伴有骨折块椎管内占位[1],20% ~ 40%伤者伴有不同程度神经损伤[2]。传统开放性椎管减压内固定术治疗胸腰椎爆裂性骨折能获得满意临床疗效,但并发症多,已引起学者们广泛关注[3-5]。随着微创技术的发展,出现了小切口、通道下、镜下等微创减压技术联合经皮内固定治疗伴有神经损伤的胸腰椎爆裂性骨折[6-7],具有与开放手术相似的临床疗效,但相比传统开放手术具有创伤小、出血量少、术后疼痛轻、可早期进行康复功能锻炼等优点[8-9],从而在临床上得到广泛应用。然而,目前椎管减压程度与神经功能预后改善的相关性仍存在一定争议[10-12]。Miyashita等[11]的研究表明,椎管减压程度与神经功能改善的相关性不明确,从而对椎管直接减压的必要性提出了质疑。盲目地追求椎管内彻底减压反而增加了神经血管损伤和医源性脊柱不稳的风险[13]。为了减少手术创伤及避免对椎管内脊髓神经的干扰,本院于2015年6月起开展了后路经皮间接减压内固定术治疗伴有神经损伤的胸腰椎爆裂性骨折患者,取得了较好临床疗效,现报告如下。
1 资料与方法 1.1 一般资料2015年6月—2017年6月,本院采用后路经皮间接减压内固定术治疗伴有神经损伤的胸腰椎爆裂性骨折患者25例,其中男17例,女8例;年龄20~60岁,平均33.7岁;骨折节段T112例、T1210例、L111例、L22例;Frankel分级C级9例,D级16例。
1.2 手术方法患者气管插管全身麻醉后俯卧于透X线的手术台上,胸前和两侧髂前上棘下放置软垫使腹部悬空。透视定位并体表标记伤椎及上下相邻椎体双侧椎弓根影,术区常规皮肤消毒、铺无菌巾。经皮穿刺定位采用Wiesner等[14]提出的方法:侧位透视下穿刺针方向应与椎体上下终板平行,正位透视下穿刺针应到达椎弓根影外上缘;当穿刺针达到椎体后缘时,正位透视下穿刺针针尖应不突破椎弓根影内侧壁,最好不超过椎弓根影横轴的外3/4。确认穿刺位置满意后建立置钉通道,结合术前CT影像沿导针置入适当长度和直径的长臂空心椎弓根螺钉(厦门大博颖精医疗器械有限公司)。根据骨折节段生理曲度,将2根连接棒预弯后分别插入双侧螺钉的“U”形头中,透视确认位置满意后锁紧一端螺帽,另外一端上下螺钉尾部分别放置延长套筒,纵向撑开复位后再逐步锁紧螺帽,根据术中侧位透视图像观察椎体后缘骨折块复位及后凸畸形矫正情况,两侧交替复位。对于复位后椎体内空隙较大者予以经皮椎弓根同种异体骨(山西奥瑞生物材料有限公司)植骨。伤口止血冲洗后逐层缝合。
1.3 术后处理术后常规使用抗生素1 d预防感染,术后1周内酌情静脉使用脱水、激素、营养神经药物减轻神经水肿,加速神经功能恢复。合理膳食,加强营养支持,术后1周内床上进行腰背肌、下肢功能锻炼,1周后佩戴支具下床进行功能锻炼,支具佩戴 > 3个月。
1.4 评价指标记录手术时间、皮肤切口长度、术中出血量、术后住院时间及手术相关并发症。所有患者术前均行平卧位正侧位X线、CT、MRI检查,术后3 d摄平卧位正侧位X线片,术后3个月、6个月、1年复查正侧位X线片、CT,测量矢状位Cobb角、伤椎椎体前缘高度百分比、伤椎楔形角、椎管占位率及椎管重塑百分比等影像学指标。矢状位Cobb角为伤椎上位椎体上终板线与伤椎下位椎体下终板线之间的夹角。伤椎椎体前缘高度百分比(%)=(伤椎前缘实际高度×2)/(伤椎上位椎体前缘高度+伤椎下位椎体前缘高度)×100%。伤椎楔形角为侧位X线片伤椎上终板线与下终板线之间的夹角;椎管占位率(%)=(1-伤椎水平正中矢状位椎管直径/伤椎上下相邻椎体正中矢状位椎管直径的平均值)×100%。椎管重塑百分比(%)=(1-末次随访椎管占位率/术后3 d椎管占位率)×100%。
术前、术后3 d及末次随访时采用Frankle分级法[15]评估患者神经功能等级,采用疼痛视觉模拟量表(VAS)评分[16]评估患者腰背部疼痛程度。
1.5 统计学处理采用SPSS 16.0软件对数据进行统计学分析,数据以x±s表示。术前、术后3 d及末次随访的测量指标两两比较采用配对t检验;多组定量资料比较采用单因素方差分析;应用Spearman秩相关进行相关性分析;以P < 0.05为差异有统计学意义。
2 结果所有患者均顺利完成手术,随访6 ~ 24(12.6± 5.6)个月,手术时间75 ~ 120(91.0±12.6)min,皮肤切口长度7.5 ~ 10.5(8.6±0.8)cm,术中出血量20 ~ 150(61.5±31.1)mL,术后住院时间3 ~ 10(5.1± 1.8)d。
术后3 d及末次随访时矢状位Cobb角、伤椎椎体前缘高度百分比、伤椎楔形角、椎管占位率及VAS评分与术前相比均显著改善,差异均有统计学意义(P < 0.05,表 1);且末次随访时椎管占位率与术后3 d相比亦显著改善,差异有统计学意义(P < 0.05,表 1)。末次随访时9例Frankle分级C级患者有2例恢复至D级、7例恢复至E级,16例D级患者均恢复至E级。术前、末次随访神经功能分别与术前、末次随访椎管占位率无明显相关性(表 2),同时神经功能改善程度与椎管重塑百分比亦无明显相关性(表 3)。
|
|
表 1 评价指标 Table 1 Evaluation index |
|
|
表 2 神经功能和椎管占位率关系 Table 2 Relationship between nerve function and spinal canal occupying rate |
|
|
表 3 神经功能改善程度与椎管重塑百分比关系 Table 3 Relationship between improvement of neurological function and spinal canal remodeling rate |
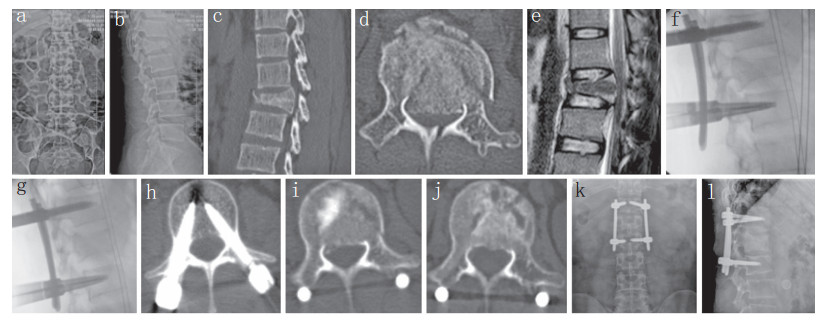
术后早期1例患者出现皮肤切口红肿,经定期换药及口服抗生素后切口愈合。未见内固定松动、断裂等并发症发生。典型病例影像学资料见图 1。
|
男,26岁,L1爆裂性骨折伴脊髓圆锥压迫出现双足肌力及会阴部感觉减退,排便费力感,术后早期排便功能好转,末次随访时神经功能基本恢复正常 a,b:术前正侧位X线片示L1爆裂性骨折伴后凸畸形 c,d:术前CT示骨折块后移侵犯椎管 e:术前MRI示前/后纵韧带完整,骨折块压迫脊髓圆锥 f:撑开复位前侧位透视 g:撑开后侧位透视示后凸畸形基本矫正 h,i:术后3 d CT示椎管占位明显减少,残留部分骨折块,内固定位置良好 j:术后6个月CT示椎管内残留骨折块基本消失,骨折愈合 k,l:术后1年正侧位X线片未见明显复位丢失及内固定失败 Male, 26 years old, L1 burst fracture combines with conus medullaris compression resulted in decreased lower extremity muscle strength and perineal sensation, laborious defecation and urination, defecation and urination function improved early after operation, and neurological function basically returned to normal at final follow-up a, b:Preoperative anteroposterior and lateral roentgenographs show L1 burst fracture with kyphosis c, d:Preoperative CTs show fracture block moved back to spinal canal e:Preoperative MRI shows anterior/posterior longitudinal ligaments are integrated, compression of conus medullaris by fracture block f:Lateral perspective before resetting g:Lateral perspective after resetting shows basic correction of kyphosis h, i:CTs at postoperative 3 d show a significant reduction in spinal canal occupying area, with some residual fractures and internal fixation in good position j:CT at postoperative 6 months shows that residual fragments in spinal canal disappeared and fracture healed k, l:Anteroposterior and lateral roentgenographs at postoperative 1 year show no significant loss of reduction and fixation failed 图 1 典型病例影像学资料 Figure 1 Radiologic data of a typical case |
不论传统开放手术还是微创椎管减压内固定术,治疗伴有神经损伤的胸腰椎爆裂性骨折,其目的都是重建脊柱稳定性,通过早期椎管减压增加神经轴浆流动、改善缺血,从而促进神经功能恢复[17]。Yang等[18]及孙兆云等[19]指出,只要后纵韧带完整,通过后路撑开整复韧带,同样可以实现椎管有效减压(间接减压),且避免了椎管内干扰,亦可获得满意疗效。Miyashita等[11]的研究表明,神经功能改善与原发神经损伤程度密切相关,而与椎管减压关系不明确,从而对椎管内神经直接减压的必要性提出了质疑。本研究结果表明,后路经皮间接减压内固定术治疗伴有神经损伤的胸腰椎爆裂性骨折安全有效,所有患者术后神经功能均获得不同程度改善,与既往文献报道开放减压的神经功能改善情况相当[20]。
3.2 经皮间接减压内固定的优缺点优点:①简单、安全、流程化。主要步骤有透视定位、穿刺扩孔、攻丝置钉、上棒复位固定,便于临床推广。②微创。手术切口小、出血量小、不剥离椎旁肌、不干扰椎管、不破坏椎体后方稳定结构。③伤椎整体复位、椎管间接减压。伤椎高度恢复的同时,恢复椎体周径和椎管前后径。④非融合固定,保留了脊柱节段的活动功能[21]。
缺点:①患者和医护人员的辐射暴露。②不适用于前/后纵韧带断裂及严重神经功能障碍患者。
3.3 手术适应证与禁忌证McCormack等[22]提出载荷分享评分(LSC)来指导手术入路的选择,3 ~ 6分可单独行后路手术,≥7分单独行前路手术。Yang等[18]研究指出,实现伤椎撑开复位、椎管间接减压的前提是前/后纵韧带的完整性。建议适应证:单节段胸腰椎爆裂性骨折,不完全神经损伤(Frankel分级C ~ D级),脊柱载荷评分≤6分,MRI证实前/后纵韧带完整性存在、椎管占位率≤50%。禁忌证:严重脊髓及马尾损伤致截瘫、多节段骨折、旋转或移位骨折、严重骨质疏松、不能耐受手术。
3.4 椎管重塑的发生与意义早期研究发现,椎体骨折后椎管内占位骨块在3 ~ 4周时明显减少[11],多在1年内自发吸收,出现椎管重塑[10-11],数年后重塑效果与外科直接减压相当[23]。有学者发现,后路器械撑开可以实现良好的间接减压,同时有助于椎管重塑,但并不能改善神经功能预后,因神经功能预后主要取决于受伤时神经损伤严重程度[11, 24],但椎管重塑可避免神经功能恶化。
本研究结果证实术前、术后神经功能状态分别与术前、术后椎管占位率无明显相关性,椎管重塑程度与神经功能改善程度也无明显相关性。椎管重塑机制仍不明确,有研究认为与硬膜囊及其前外侧血管丛的搏动有关[25]。本研究结果显示,后路经皮间接减压可有效及时扩大椎管容积,从而改善血管丛及脑脊液循环通畅度,进而恢复硬膜囊搏动的生理节律,改善脊髓局部缺血状态,促进残留骨折块的重塑和神经功能的恢复。
综上所述,后路经皮间接减压内固定术可避免椎管内直接减压操作,保护脊柱后方结构,减少手术创伤,临床疗效满意,严格掌握手术适应证下对于伴有不完全神经损伤的胸腰椎爆裂性骨折的治疗是一种微创、安全、有效的选择。
| [1] | Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries[J]. Spine (Phila Pa 1976), 1983, 8(8): 817–831. DOI:10.1097/00007632-198311000-00003 |
| [2] | Katsuura Y, Osborn JM, Cason GW. The epidemiology of thoracolumbar trauma:a meta-analysis[J]. J Orthop, 2016, 13(4): 383–388. DOI:10.1016/j.jor.2016.06.019 |
| [3] | Charles YP, Steib JP. Management of thoracolumbar spine fractures with neurologic disorder[J]. Orthop Traumatol Surg Res, 2015, 101(1 Suppl): S31–S40. |
| [4] | Ge CM, Wang YR, Jiang SD, et al. Thoracolumbar burst fractures with a neurological deficit treated with posterior decompression and interlaminar fusion[J]. Eur Spine J, 2011, 20(12): 2195–2201. DOI:10.1007/s00586-011-1875-6 |
| [5] | 曾忠友, 籍剑飞, 严卫锋, 等. 270°或360°椎管减压并一期椎弓根螺钉固定及椎体重建治疗严重胸腰椎骨折的疗效对比[J]. 脊柱外科杂志, 2016, 14(6): 345–351. DOI:10.3969/j.issn.1672-2957.2016.06.006 |
| [6] | 潘健, 高浩然, 马舟涌, 等. 微创通道下减压结合经皮螺钉复位固定治疗伴有神经根损伤的胸腰椎骨折[J]. 脊柱外科杂志, 2015, 13(6): 337–341. DOI:10.3969/j.issn.1672-2957.2015.06.005 |
| [7] | 李长青, 张伟, 常献, 等. 小切口减压结合经皮椎弓根螺钉内固定治疗伴神经功能损害的胸腰椎骨折[J]. 中国脊柱脊髓杂志, 2014, 24(5): 395–399. DOI:10.3969/j.issn.1004-406X.2014.05.04 |
| [8] | 张伟, 李海音, 李杰, 等. 微创减压联合经皮固定与传统开放手术治疗伴神经损害胸腰椎骨折的疗效比较[J]. 中国脊柱脊髓杂志, 2015, 25(5): 420–426. DOI:10.3969/j.issn.1004-406X.2015.05.08 |
| [9] | 雷亮, 尚剑, 韩昕光, 等. 胸腰椎爆裂骨折的间接减压与直接减压疗效比较的Meta分析[J]. 中华创伤骨科杂志, 2012, 14(12): 1065–1071. DOI:10.3760/cma.j.issn.1671-7600.2012.12.011 |
| [10] | Mohanty SP, Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise?[J]. Spinal Cord, 2002, 40(6): 295–299. DOI:10.1038/sj.sc.3101283 |
| [11] | Miyashita T, Ataka H, Tanno T. Clinical results of posterior stabilization without decompression for thoracolumbar burst fractures:is decompression necessary?[J]. Neurosurg Rev, 2012, 35(3): 447–454. DOI:10.1007/s10143-011-0363-0 |
| [12] | Mohanty SP, Bhat SN, Ishwara-Keerthi C. The effect of posterior instrumentation of the spine on canal dimensions and neurological recovery in thoracolumbar and lumbar burst fractures[J]. Musculoskelet Surg, 2011, 95(2): 101–106. DOI:10.1007/s12306-011-0111-1 |
| [13] | Ataka H, Tanno T, Yamazaki M. Posterior instrumented fusion without neural decompression for incomplete neurological deficits following vertebral collapse in the osteoporotic thoracolumbar spine[J]. Eur Spine J, 2009, 18(1): 69–76. DOI:10.1007/s00586-008-0821-8 |
| [14] | Wiesner L, Kothe R, Ruther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine[J]. Spine (Phila Pa 1976), 1999, 24(15): 1599–1603. DOI:10.1097/00007632-199908010-00015 |
| [15] | Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia[J]. Paraplegia, 1969, 7(3): 179–192. |
| [16] | Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127–1131. |
| [17] | Riska EB, Myllynen P, Böstman O. Anterolateral decompression for neural involvement in thoracolumbar fractures. A review of 78 cases[J]. J Bone Joint Surg Br, 1987, 69(5): 704–708. |
| [18] | Yang H, Shi J, Ebraheim M, et al. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion[J]. Eur Spine J, 2011, 20(3): 380–386. DOI:10.1007/s00586-010-1542-3 |
| [19] | 孙兆云, 陈伯华, 郭新银, 等. 后路间接减压治疗不同椎管侵占率的胸腰椎爆裂骨折的效果观察[J]. 中华骨与关节外科杂志, 2015, 8(2): 135–139. |
| [20] | Zahra B, Jodoin A, Maurais G, et al. Treatment of thoracolumbar burst fractures by means of anterior fusion and cage[J]. J Spinal Disord Tech, 2012, 25(1): 30–37. DOI:10.1097/BSD.0b013e31820bb0a9 |
| [21] | Toyone T, Ozawa T, Inada K, et al. Short-segment fixation without fusion for thoracolumbar burst fractures with neurological deficit can preserve thoracolumbar motion without resulting in post-traumatic disc degeneration:a 10-year follow-up study[J]. Spine (Phila Pa 1976), 2013, 38(17): 1482–1490. DOI:10.1097/BRS.0b013e318297bdb7 |
| [22] | McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures[J]. Spine (Phila Pa 1976), 1994, 19(15): 1741–1744. DOI:10.1097/00007632-199408000-00014 |
| [23] | 潘俊, 王根林, 史金辉, 等. 间接复位治疗胸腰椎爆裂型骨折术后椎管重塑形[J]. 脊柱外科杂志, 2012, 10(2): 72–75. DOI:10.3969/j.issn.1672-2957.2012.02.003 |
| [24] | Moon YJ, Lee KB. Relationship between clinical outcomes and spontaneous canal remodeling in thoracolumbar burst fracture[J]. World Neurosurg, 2016, 89: 58–64. DOI:10.1016/j.wneu.2016.02.010 |
| [25] | Herndon WA, Galloway D. Neurologic return versus cross-sectional canal area in incomplete thoracolumbar spinal cord injuries[J]. J Trauma, 1988, 28(5): 680–683. DOI:10.1097/00005373-198805000-00022 |
 2019, Vol.17
2019, Vol.17  Issue(1): 1-5
Issue(1): 1-5


