2. 瑞安市人民医院骨科, 温州 325200
2. Department of Orthopaedics, Ruian People's Hospital, Wenzhou 325200, Zhejiang, China
颈椎前路融合内固定术自1958年Smith等[1]报道以来,经过半个多世纪的发展,已经成为治疗颈椎退行性疾病、外伤、肿瘤、感染等的重要手术方式。同时,颈椎融合术后发生邻椎病(ASD)的病例逐渐增多,受到国内外学者的关注[2]。对于临床症状、体征明显,影像学表现典型且非手术治疗无效的ASD患者,手术是有效的治疗方式。由于瘢痕粘连及原内固定材料暴露、拆除困难等问题,ASD的前路翻修手术一直是脊柱外科中的难点。Solis融合器因其无需拆除原内固定器、无需在椎体前方增加内固定及零切迹等天然优势,可以极大降低ASD前路翻修手术的难度及风险。本研究通过回顾性分析使用Solis融合器行颈椎前路翻修术的12例ASD患者的临床资料,总结Solis融合器在颈椎前路翻修术中的优势,现报告如下。
1 资料与方法 1.1 一般资料2007年4月—2016年6月,本院脊柱外科收治因颈椎前路减压固定融合术后发生ASD的患者12例,所有患者均使用Solis融合器行前路翻修手术,其中男9例、女3例,年龄41 ~ 72(62.2±7.1)岁;翻修手术节段为C3/C4 6例,C4/C5 2例,C5/C6 2例,C6/C7 2例。所有患者均为单节段ASD,且不伴有严重后纵韧带骨化及黄韧带肥厚、骨化。所有患者术前均行颈椎正侧位、过伸过屈位X线片,颈椎CT与三维重建及颈椎MRI检查。
1.2 手术方法手术均采用颈椎前路右侧横切口,经颈动脉鞘与气管-食管间隙显露至椎前间隙,旋出前路钛板近发生ASD椎间隙侧螺钉1枚,无需拆除原固定钛板,置入撑开器螺钉,上好撑开器,行单间隙减压后置入Solis融合器(史赛克,美国),主要成分为聚醚醚酮(PEEK),为4°楔形、中空盒状,带有齿状表面及钛钉,有自体稳定功能。融合器内均置入自体髂骨。术后嘱患者3周内坐立时严格佩戴颈托,卧床时无需佩戴。
1.3 疗效评价记录手术时间、术中出血量;术后3、6个月门诊随访,记录术前及末次随访时颈椎功能障碍指数(NDI)[3]、日本骨科学会(JOA)评分[4]、吞咽困难等情况,并行颈椎正侧位X线检查评估融合情况。融合标准:X线片可见融合器与椎体界面有骨小梁通过,融合器与上下椎体界面间无透亮带,颈椎侧位、过伸过屈位X线片示棘突无异常活动[5]。
1.4 统计学处理采用SPSS 17.0软件对数据进行统计学分析,数据以x±s表示,术前、术后NDI及JOA评分比较采用重复测量资料的方差分析;以P < 0.05为差异有统计学意义。
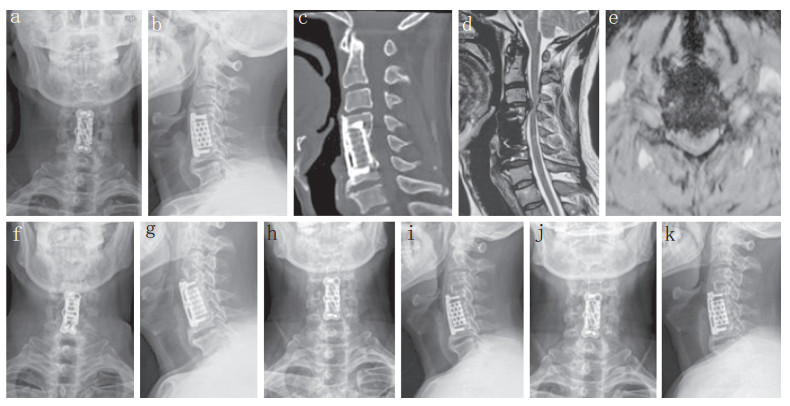
2 结果所有患者随访4 ~ 114(61.8±29.3)个月。手术时间80 ~ 135(106.4±18.1)min,术中出血量20 ~ 100(61.7±22.9)mL。所有患者术中未出现食管、气管、血管等重要脏器和组织损伤,均未发生创口感染、脑脊液漏等并发症。术后3个月、末次随访时NDI、JOA评分均较术前改善,差异有统计学意义(P < 0.05,表 1)。所有患者末次随访时X线片示植骨融合,未出现融合器沉降、移位等情况。末次随访时均未出现吞咽困难。典型病例影像学资料见图 1。
|
|
表 1 术前、术后各时间点NDI和JOA评分 Table 1 NDI and JOA score at before and all time points after operation |
|
a,b:术前正侧位X线片示首次前路术后植骨完全融合 c:术前矢状位CT示首次前路手术植骨融合,钛网位置良好 d,e:术前MRI示融合节段上方C3/C4椎间盘突出,脊髓受压 f,g:术后即刻正侧位X线片示Solis融合器位置良好 h,i:术后1个月正侧位X线片示Solis融合器位置良好,无沉降、移位 j,k:术后3个月正侧位X线片示Solis融合器位置良好,植骨融合 a, b:Preoperative anteroposterior and lateral roentgenographs show bone graft fusion after first anterior approach c:Preoperative sagittal CT shows bone graft fusion and titanium mesh cage in good position d, e:Preoperative MRIs show C3/C4 intervertebral disc herniation above fusion segment and spinal cord compression f, g:Anteroposterior and lateral roentgenographs immediately after surgery show Solis cage in good position h, i:Anteroposterior and lateral roentgenographs at postoperative 1 month show Solis cage in good position without migration or subsidence j, k:Anteroposterior and lateral roentgenographs at postoperative 3 months show Solis cage in good position and bone graft fusion 图 1 典型病例影像学资料 Figure 1 Imaging data of a typical case |
近年来,颈椎前路手术后邻近节段退行性变越发常见[6],有荟萃分析报道称颈椎术后影像学上的邻近节段退行性变发生率为28.28%,有临床症状的ASD发生率为13.34%,需要再次手术的邻近节段占5.78%[7]。目前ASD的发生原因仍不明确,公认的危险因素有术前邻近节段已存在退行性变、钢板位置不良、颈椎曲度恢复不佳、定位针误入相邻间隙等[8-11]。对于临床症状、体征明显且非手术治疗无效的ASD患者,应考虑行翻修手术治疗,手术方式主要包括前路减压融合内固定术、前路人工椎间盘置换术、后路减压椎管成形术、后路减压融合内固定术等[12-14]。一般认为,对邻近节段退行性变节段≤2个且不伴严重后纵韧带或黄韧带骨化的患者,应选择前路减压融合术[15]。
颈椎前路手术后行前路翻修术存在以下难点。①需拆除原手术钢板,手术步骤繁琐,手术时间相对延长,暴露范围大,需延长切口。②原切口存在瘢痕粘连,暴露时容易出血,瘢痕粘连在长时间手术暴露下容易损伤前方相邻的气管、食管等重要脏器,且术后由于创口大、出血量大,容易形成创口血肿。③前路钛板的应用还会增加吞咽困难,钛板螺钉松动,食管、气管损伤的可能;已有研究证实,前路钛板的应用与ASD的发生密切相关[16-17]。
Solis融合器在前路翻修术中的天然优势:①无需拆除原内固定器,可避开瘢痕粘连区域,降低损伤气管、食管等重要脏器组织的概率;减少手术步骤,明显缩短手术时间;减少术中损伤及出血量,降低术后血肿的发生率。②无需额外钛板固定,为零切迹融合,对前方食管刺激小,术后不易发生吞咽困难等并发症,也降低了再次发生ASD的概率[16-17]。③Solis融合器外观呈椎间盘状,与终板接触面积大,且融合器两侧配有钛合金钉针,结合上下缘的锯齿状边缘,可使手术节段获得即刻稳定性。本研究中患者均未发生融合器松动、移位,末次随访时均获得骨性愈合,证实Solis融合器应用于ASD的翻修手术中效果良好。
综上所述,Solis融合器应用在颈椎前路手术后ASD翻修术中安全有效,无需拆除原手术内固定器,减少暴露损伤,简化手术步骤,且无需额外前路钛板固定,减少吞咽困难的发生。但Solis融合器仅靠2枚钛合金钉针固定,稳定性及融合率与前路钛板相比是否有差异尚不明确,仍需长期临床随访及多中心大样本的随机对照研究来证实其远期疗效。
| [1] | Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion[J]. J Bone Joint Surg Am, 1958, 40-A(3): 607–624. |
| [2] | van Eck CF, Regan C, Donaldson WF, et al. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion:a study of 672 consecutive patients[J]. Spine(Phila Pa 1976), 2014, 39(26): 2143–2147. DOI:10.1097/BRS.0000000000000636 |
| [3] | Vernon H, Mior S. The neck disability index:a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409–415. |
| [4] | Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890–1895. DOI:10.1097/00007632-200109010-00014 |
| [5] | Wang JC, Mcdonough PW, Endow K, et al. The effect of cervical plating on single-level anterior cervical discectomy and fusion[J]. J Spinal Disord, 1999, 12(6): 467–471. |
| [6] | 逄川, 海涌, 杨晋才, 等. 颈椎融合术后邻近节段退变的研究现状[J]. 脊柱外科杂志, 2013, 11(2): 112–114. DOI:10.3969/j.issn.1672-2957.2013.02.012 |
| [7] | Kong L, Cao J, Wang L, et al. Prevalence of adjacent segment disease following cervical spine surgery:a PRISMA-compliant systematic review and meta-analysis[J]. Medicine (Baltimore), 2016, 95(27): e4171. DOI:10.1097/MD.0000000000004171 |
| [8] | Chung JY, Kim SK, Jung ST, et al. Clinical adjacentsegment pathology after anterior cervical discectomy and fusion:results after a minimum of 10-year follow-up[J]. Spine J, 2014, 14(10): 2290–2298. DOI:10.1016/j.spinee.2014.01.027 |
| [9] | Litrico S, Lonjon N, Riouallon G, et al. Adjacent segment disease after anterior cervical interbody fusion:a multicenter retrospective study of 288 patients with long-term follow-up[J]. Orthop Traumatol Surg Res, 2014, 100(6 Suppl): S305–S309. |
| [10] | Alhashash M, Shousha M, Boehm H, et al. Adjacent segment disease after cervical spine fusion:evaluation of a 70 patient long-term follow-up[J]. Spine (Phila Pa 1976), 2018, 43(9): 605–609. |
| [11] | Park MS, Kelly MP, Lee DH, et al. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis[J]. Spine J, 2013, 14(7): 1228–1234. |
| [12] | Bin S, Xiangwang H, Sheng X, et al. Artificial cervical disk replacement for the treatment of adjacent segment disease after anterior cervical decompression and fusion[J]. Clin Spine Surg, 2017, 30(5): E587–E591. DOI:10.1097/BSD.0000000000000173 |
| [13] | O'Neill KR, Wilson RJ, Burns KM, et al. Anterior cervical discectomy and fusion for adjacent segment disease:clinical outcomes and cost utility of surgical intervention[J]. Clin Spine Surg, 2016, 29(6): 234–241. DOI:10.1097/BSD.0b013e31828ffc54 |
| [14] | Wang F, Wang P, Miao DC, et al. Different surgical approaches for the treatment of adjacent segment diseases after anterior cervical fusion:a retrospective study of 49 patients[J]. Medicine(Baltimore), 2017, 96(23): e7042. |
| [15] | 王洪立, 姜建元, 吕飞舟, 等. 颈椎前路融合术后邻近节段退变性疾病的原因分析及治疗策略[J]. 中华骨科杂志, 2014, 34(9): 915–922. DOI:10.3760/cma.j.issn.0253-2352.2014.09.005 |
| [16] | Ahn SS, Paik HK, Chin DK, et al. The fate of adjacent segments after anterior cervical discectomy and fusion:the influence of an anterior plate system[J]. World Neurosurg, 2016, 89: 42–50. DOI:10.1016/j.wneu.2016.01.013 |
| [17] | Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease[J]. Spine J, 2013, 13(3): 342–351. |
 2019, Vol.17
2019, Vol.17  Issue(1): 25-27, 36
Issue(1): 25-27, 36


