随着智能设备的广泛使用,颈椎病已成为危及人类健康的常见病、多发病。目前颈椎病手术治疗的经典术式有前路颈椎椎间盘切除融合术(ACDF)、前路颈椎椎体次全切除融合术(ACCF)及后路颈椎椎管扩大椎板成形术等。随着颈椎融合器的发展及手术技术的不断完善,ACDF得到广泛应用,成为治疗颈椎病的金标准[1-2]。传统的ACDF使用融合器并钛板固定,以增加减压节段的稳定性、提高融合率[3-4]。但钛板可增加术后吞咽困难、邻近节段骨化的发生率[5-7]。为了减少此类并发症的发生,零切迹自稳型颈椎融合器(ROI-C)应运而生。本研究回顾性分析了2013年5月—2015年5月本院在ACDF中应用ROI-C或融合器并钛板固定患者的临床资料,比较两种处理方式临床疗效、术后吞咽困难和邻近节段骨化的发生率,为ACDF选择合适的固定方式提供参考。
1 资料与方法 1.1 研究对象纳入标准:①MRI等影像学检查提示脊髓或神经根受压;②伴明显的相应临床症状,如颈肩上肢疼痛麻木、胸部束带感、四肢乏力、行走不稳、脚踩棉花感等;③经正规非手术治疗 > 6个月,症状无明显缓解,影响正常生活;④采用ACDF治疗;⑤随访数据资料完善,随访时间 > 24个月。排除标准:①术中联合使用ROI-C、融合器并钛板;②严重的颈椎不稳、颈椎骨折脱位、椎管狭窄、肿瘤等;③术前已有吞咽困难及邻近节段骨化。根据以上标准,共纳入颈椎病患者108例,其中59例术中应用ROI-C固定(A组),49例术中应用融合器并钛板固定(B组)。2组患者基本资料差异无统计学意义,具有可比性(P > 0.05,表 1)。
|
|
表 1 一般资料 Table 1 General information |
所有患者手术均由同一位主任医师完成。患者麻醉成功后取仰卧位,做颈前右侧横切口,切开皮肤、皮下及颈阔肌,分离颈深筋膜,沿气管、食管鞘和血管鞘间隙分离至椎体前缘,手动拉钩将气管、食管鞘拉向左侧,间歇性松开一段时间,纵行切开颈前筋膜,将颈长肌拉向两侧。透视下定位相应椎间隙,经C形臂X线机透视无误后,咬除相应椎体前缘骨赘,置入椎体撑开螺钉,用撑开器适当撑开椎体,摘除椎间盘及髓核组织,切除后纵韧带,彻底减压至硬膜囊及神经根无明显压迫。处理相应上下终板后,A组采用大小合适的ROI-C(LDR公司,法国)固定,B组采用充填有同种异体骨条的融合器(威高,山东)、椎体前置钛板、螺钉(威高,山东)固定。透视确认融合器位置良好。彻底止血,清点器械、敷料无误后,颈部切口置负压引流管1根,逐层缝合切口。术中诱发电位监测未见异常。术后予以补液、镇痛等支持治疗,2 d后拔除引流管,佩戴颈托下床活动,术后佩戴颈托3个月。
1.3 临床评估术前术后采用日本骨科学会(JOA)评分[8]、颈椎功能障碍指数(NDI)[9]进行功能评估。计算JOA评分改善率,JOA评分改善率(%)=(术后JOA评分-术前JOA评分)/(17-术前JOA评分)×100%。将JOA评分改善率分为4个等级:极好(≥75%)、好(≥50%且 < 75%)、一般(≥25%且 < 50%)、差(< 25%)。采用Odom法[10]对手术疗效进行判定:优,术后症状、体征近乎消失;良,症状、体征大部分缓解,可正常工作;可,症状、体征部分好转,无法正常工作;差,症状、体征与术前基本相同。术后3 ~ 48个月评估吞咽困难情况,根据Bazaz评分[11]将术后吞咽困难程度分为无(无吞咽问题)、轻度(很少发生吞咽困难)、中度(偶尔发生吞咽困难)、重度(频繁发生吞咽困难)。
1.4 影像学评估所有患者术前、术后3个月及末次随访时均拍摄颈椎标准正侧位X线片。测量颈椎C2~7 Cobb角[12]、颈椎弓深及上位邻近节段椎间隙高度。Cobb角为C2与C7椎体下终板连线的垂线之间的夹角。颈椎弓深为各椎体后缘连接成的弧线到齿突后上缘与C7椎体后下缘连线的最远垂直距离。上位邻近节段椎间隙高度为该间隙下位椎体上终板中点与上位椎体下终板中点连线的距离(下位椎间隙易受锁骨的遮挡,故本研究只测量上位椎间隙高度)。依据Vaccraro标准[13]评估椎间植骨融合情况,融合标准:颈椎动力位X线片示邻近椎体位移角度≤2°;椎间隙高度恢复,无塌陷;骨小梁与上下椎体骨性连接;植骨区与椎体上下缘间无透亮线。邻近节段骨化分级:0级,邻近节段无骨化形成;1级,有骨化形成,但骨赘未超过椎间隙的1/2;2级,骨化超过椎间隙的1/2,但未跨越椎间隙;3级,骨化跨越椎间隙,形成连续骨桥[6]。2位独立观察者在2次不同情况下确定邻近节段骨化等级,4次测量的平均值作为最终等级。
1.5 统计学处理应用SPSS 20.0软件对数据进行统计学分析。计量资料以x±s表示,组间比较采用两样本t检验,组内比较采用配对t检验;计数资料以例数和百分比表示,组间比较采用χ2检验;以P < 0.05为差异有统计学意义。
2 结果所有手术顺利完成,术中无气管、食管、硬膜、脊髓损伤发生,术后无声音嘶哑、饮水呛咳、呼吸困难等情况发生,切口均Ⅰ/甲级愈合,无下肢深静脉血栓等并发症。所有患者均于术后3 ~ 5 d出院,随访期内脊髓、神经受压症状较术前明显缓解。
2组患者术后3个月及末次随防颈椎Cobb角和弓深均较术前明显改善,差异有统计学意义(P < 0.05,表 2),上位邻近节段椎间隙高度与术前相比无明显变化(P > 0.05,表 2);末次随访时2组颈椎Cobb角、弓深及上位邻近节段椎间隙高度均获得良好维持,与术后3个月相比差异无统计学意义(P > 0.05,表 2)。
|
|
表 2 观察指标 Table 2 Observation indexes |
2组患者术后3个月及末次随访时JOA评分均较术前明显上升,NDI均较术前明显下降,差异均有统计学意义(P < 0.05,表 2);组间比较,同时间点JOA评分和NDI差异均无统计学意义(P > 0.05,表 2)。末次随访时,A组JOA评分改善率评价优13例、良34例、可12例,B组优10例、良31例、可7例、差1例,组间差异无统计学意义(P > 0.05,表 2)。手术治疗效果按Odom法进行判定,A组优良率为93.2%(55/59),B组为91.8%(45/49),组间差异无统计学意义(P > 0.05)。术后3个月时,A组融合率为96.6%(57/59),B组为93.9%(46/49),差异无统计学意义(P > 0.05);末次随访时所有患者均获得骨性融合,无插片断裂,融合器下沉、松动、退出等情况。
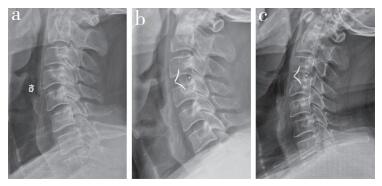
A组术后出现2例轻度吞咽困难,对症处理3 ~ 5 d后消失;B组术后出现4例轻度吞咽困难,3例中度吞咽困难,随访3个月时仍有3例存在轻度吞咽困难,至末次随访时全部消失。在颈椎侧位X线片上,由于部分患者手术下位邻近节段影像受到锁骨影的影响,A组观察到104个节段,B组观察到88个节段。A组中7个节段发生邻近节段骨化(6.7%),其中头端4个、尾端3个,1级5个、2级2个;B组中14个节段发生邻近节段骨化(15.9%),其中头端6个、尾端8个,1级4个、2级10个。A组邻近节段骨化发生率低于B组,差异有统计学意义(P < 0.05)。2组患者典型病例影像学资料见图 1,2。
|
a:术前X线片 b:术后3个月X线片示无邻近节段骨化形成 c:术后48个月X线片示无邻近节段骨化形成 a:Preoperative roentgenograph b:Roentgenograph at postoperative 3 months shows no adjacent segmental ossification development c:Roentgenograph at postoperative 48 months shows no adjacent segmental ossification development 图 1 A组典型病例影像学资料 Figure 1 Radiologic data of a typical case in group A |

|
a:术前X线片 b:术后3 d X线片示无邻近节段骨化形成 c:术后3个月X线片示无邻近节段骨化形成d:术后24个月X线片示邻近节段骨化形成达2级(C3,4) a:Preoperative roentgenograph b:Roentgenograph at postoperative 3 d shows no adjacent segmental ossification development c:Roentgenograph at postoperative 3 months shows no adjacent segmental ossification development d:Roentgenograph at postoperative 24 months shows adjacent segmental ossification of grade 2(C3, 4) 图 2 B组典型病例影像学资料 Figure 2 Radiologic data of a typical case in group B |
ACDF是治疗颈椎病的经典术式,能够直接去除致压物减压,通过椎间隙的撑开有效恢复颈椎生理曲度,重建病变节段的稳定性,临床疗效满意。传统的颈前路手术中融合器并钛板固定的使用较为广泛,钛板的使用可增加颈椎稳定性、减少融合器松动及提高椎间融合率等[3-4]。但钛板的使用也扩大了前纵韧带剥离范围,增加了食管、气管、神经损伤风险,同时也会增加吞咽困难发生的可能性[5-7]。ROI-C上方弧形部分遵循自然的解剖形态,前缘高于后缘,使骨与置入物紧密接触;横截面积大,外周承重面大,增加了植骨与上下椎体的接触面积[14-15]。本研究2组患者术后3个月及末次随访时JOA评分均较术前明显上升,NDI均较术前明显下降,与文献报道一致[16-17];且组间JOA评分改善率和手术治疗效果优良率差异均无统计学意义,说明2种融合器疗效相当。
使用ROI-C能够简化ACDF手术步骤,无需前路钛板手术中螺钉钻孔、攻丝等步骤,节约了手术时间,减少了手术出血量[18]。无需椎体前方钛板固定,具有更小的手术暴露范围,减少了对气管、食管和神经的牵拉,降低了相关临床并发症发生率[19]。同时,在生物力学稳定性方面,ROI-C与融合器并钛板具有相同功效[20]。本研究中2组手术时间、出血量无明显差异,可能与样本量较小、术者操作水平及缝合技术熟练程度等有关。
吞咽困难是一种与颈椎前路钛板相关的术后并发症。颈椎前路融合术中应用钛板的术后吞咽困难发生率为1% ~ 62%[21-22]。可能的原因包括椎前软组织肿胀、食管受牵拉、血肿压迫和钛板与周围组织粘连等[23-24]。Lee等[5]认为较薄的颈椎前路钛板能显著减少吞咽困难的发生率。虽然目前钛板比早期的设计更薄,但仍会导致术后吞咽困难的发生。ROI-C可插入椎间隙中,无需钛板固定,避免了直接刺激食管并减轻食管粘连,可减少吞咽困难的发生,但临床疗效有待长期随访研究。本研究随访时间内2组吞咽困难的发生率分别为3.39%(A组)和14.3%(B组),A组吞咽困难的发生率和严重程度更低、持续时间更短,与既往研究结果一致[5, 25-26]。
邻近节段骨化通常被认为是异位骨化的一种类型,其发生可能与钛板对相邻水平前纵韧带的刺激和剥离过多有关,但具体机制目前尚不明确。钛板上下缘与相邻椎间盘的距离(PDD)是邻近节段骨化发生的关键风险因素,PDD越小,发生骨化的可能性越大,骨化的程度也会增高。Park等[6]认为,PDD ≥ 5 mm时骨化发生的可能性明显降低。当PDD < 5 mm,邻近节段骨化的风险是PDD≥5 mm时的2 ~ 5倍[23, 27]。Lee等[28]认为,使用较长的螺钉,头尾端分别从椎体前缘靠近椎间盘的点进钉,向远离椎间盘的方向成角打入,以尽量缩短钛板的长度,最大限度地扩大与相邻节段的距离,能够明显降低邻近节段骨化发生率和严重程度。本研究B组中未见3级骨化形成,与既往研究结果[6]不完全一致,可能与本研究术中尽可能选用较短钛板和减少前纵韧带的剥离有关。ROI-C避免了钛板的使用,不受PDD的影响,本研究中A组邻近节段骨化发生率为6.73%,明显低于融合器并钛板组的15.91%。该结果与Bucci等[25]的报道一致,进一步证实了ROI-C能够降低邻近节段骨化的发生率。
ROI-C置入相对简单,但也有局限性。其不适用于严重颈椎不稳及骨折脱位患者,此类患者韧带及骨性结构受损,无法保证颈椎责任节段的稳定性;严重骨质疏松的老年患者也禁用,术后易出现融合器松动及下沉;其齿状结构的双插片设计给术后翻修带来一定困难。
综上所述,在ACDF中应用ROI-C治疗颈椎病安全、有效。与融合器并钛板固定相比,ROI-C能减少术后吞咽困难和邻近节段骨化的发生率。本研究的不足:①样本量较小;②随访时间相对较短,未对邻近节段骨化展开进一步研究;③为回顾性研究,不可避免存在一些偏倚。因此,在今后的工作中需要多中心、大样本、长期随访的研究,以提高研究结果的可靠性。
| [1] | Schroeder GD, Kurd MF, Millhouse PW, et al. Performing an anterior cervical discectomy and fusion[J]. Clin Spine Surg, 2016, 29(5): 186–190. DOI:10.1097/BSD.0000000000000383 |
| [2] | Guan L, Hai Y, Yang JC, et al. Anterior cervical discectomy and fusion may be more effective than anterior cervical corpectomy and fusion for the treatment of cervical spondylotic myelopathy[J]. BMC Musculoskeletal Disord, 2015, 16: 29. DOI:10.1186/s12891-015-0490-9 |
| [3] | Sugawara T. Anterior cervical spine surgery for degenerative disease:a review[J]. Neurol Med Chir (Tokyo), 2015, 55(7): 540–546. DOI:10.2176/nmc.ra.2014-0403 |
| [4] | Matz PG, Ryken TC, Groff MW, et al. Techniques for anterior cervical decompression for radiculopathy[J]. J Neurosurg Spine, 2009, 11(2): 183–197. DOI:10.3171/2009.2.SPINE08721 |
| [5] | Lee MJ, Bazaz R, Furey CG, et al. Influence of anterior cervical plate design on dysphagia:a 2-year prospective longitudinal follow-up study[J]. J Spinal Disord Tech, 2005, 18(5): 406–409. DOI:10.1097/01.bsd.0000177211.44960.71 |
| [6] | Park JB, Cho YS, Riew KD. Development of adjacentlevel ossification in patients with an anterior cervical plate[J]. J Bone Joint Surg Am, 2005, 87(3): 558–563. DOI:10.2106/JBJS.C.01555 |
| [7] | Yang JY, Song HS, Lee M, et al. Adjacent level ossification development after anterior cervical fusion without plate fixation[J]. Spine (Phila Pa 1976), 2009, 34(1): 30–33. DOI:10.1097/BRS.0b013e318190d833 |
| [8] | Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890–1895. DOI:10.1097/00007632-200109010-00014 |
| [9] | Vernon H, Mior S. The neck disability index:a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409–415. |
| [10] | Odom GL, Finney W, Woodhall B. Cervical disk lesions[J]. J Am Med Assoc, 1958, 166(1): 23–28. DOI:10.1001/jama.1958.02990010025006 |
| [11] | Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery:a prospective study[J]. Spine (Phila Pa 1976), 2002, 27(22): 2453–2458. DOI:10.1097/00007632-200211150-00007 |
| [12] | Mummaneni PV, Burkus JK, Haid RW, et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion:a randomized controlled clinical trial[J]. J Neurosurg Spine, 2007, 6(3): 198–209. DOI:10.3171/spi.2007.6.3.198 |
| [13] | Vaccaro AR, Carrino JA, Venger BH, et al. Use of a bioabsorbable anterior cervical plate in the treatment of cervical degenerative and traumatic disc disruption[J]. J Neurosurg, 2002, 97. |
| [14] | Ferguson SJ, Visser JM, Polikeit A. The long-term mechanical integrity of non-reinforced PEEK-OPTIMA polymer for demanding spinal applications:experimental and finite-element analysis[J]. Eur Spine J, 2006, 15(2): 149–156. DOI:10.1007/s00586-005-0915-5 |
| [15] | Kulkarni AG, Hee HT, Wong HK. Solis cage(PEEK) for anterior cervical fusion:preliminary radiological results with emphasis on fusion and subsidence[J]. Spine J, 2007, 7(2): 205–209. |
| [16] | Burkhardt JK, Mannion AF, Marbacher S, et al. A comparative effectiveness study of patient-rated and radiographic outcome after 2 types of decompression with fusion for spondylotic myelopathy:anterior cervical discectomy versus corpectomy[J]. Neurosurg Focus, 2013, 35(1): E4. |
| [17] | Liu J, Chen X, Liu Z, et al. Anterior cervical discectomy and fusion versus corpectomy and fusion in treating two-level adjacent cervical spondylotic myelopathy:a minimum 5-year follow-up study[J]. Arch Orthop Trauma Surg, 2015, 135(2): 149–153. DOI:10.1007/s00402-014-2123-4 |
| [18] | 鲍达, 马远征. 锚定式颈椎椎间融合器在颈椎前路再手术中的应用[J]. 脊柱外科杂志, 2014, 12(6): 363–366. DOI:10.3969/j.issn.1672-2957.2014.06.011 |
| [19] | 李国, 宫峰, 阮亮. 自锁双锚定融合器治疗颈椎病早期疗效[J]. 脊柱外科杂志, 2016, 14(1): 10–15. DOI:10.3969/j.issn.1672-2957.2016.01.003 |
| [20] | Scholz M, Reyes PM, Schleicher P, et al. A new stand-alone cervical anterior interbody fusion device:biomechanical comparison with established anterior cervical fixation devices[J]. Spine(Phila Pa 1976), 2009, 34(2): 156–160. DOI:10.1097/BRS.0b013e31818ff9c4 |
| [21] | Smith-Hammond CA, New KC, Pietrobon R, et al. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients:comparison of anterior cervical, posterior cervical, and lumbar procedures[J]. Spine(Phila Pa 1976), 2004, 29(13): 1441–1446. DOI:10.1097/01.BRS.0000129100.59913.EA |
| [22] | Wang ZD, Zhu RF, Yang HL, et al. The application of a zero-profile implant in anterior cervical discectomy and fusion[J]. J Clin Neurosci, 2014, 21(3): 462–466. DOI:10.1016/j.jocn.2013.05.019 |
| [23] | Joaquim AF, Murar J, Savage JW, et al. Dysphagia after anterior cervical spine surgery:a systematic review of potential preventative measures[J]. Spine J, 2014, 14: 2246–2260. DOI:10.1016/j.spinee.2014.03.030 |
| [24] | 马骏雄, 陈语, 项良碧, 等. 单节段和双/多节段颈椎前路减压融合术后椎前软组织肿胀及吞咽困难发生率的比较[J]. 脊柱外科杂志, 2015, 13(1): 41–44. DOI:10.3969/j.issn.1672-2957.2014.10.13 |
| [25] | Bucci MN, Oh D, Cowan RS, et al. The ROI-C zeroprofile anchored spacer for anterior cervical discectomy and fusion:biomechanical profile and clinical outcomes[J]. Med Devices (Auckl), 2017, 10: 61–69. |
| [26] | Yang H, Chen D, Wang X, et al. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system[J]. Arch Orthop Trauma Surg, 2015, 135(6): 781–787. DOI:10.1007/s00402-015-2212-z |
| [27] | Kim HJ, Kelly MP, Ely CG, et al. The risk of adjacentlevel ossification development after surgery in the cervical spine:are there factors that affect the risk? A systematic review[J]. Spine (Phila Pa 1976), 2012, 37(22 Suppl): S65–S74. |
| [28] | Lee DH, Lee JS, Yi JS, et al. Anterior cervical plating technique to prevent adjacent-level ossification development[J]. Spine J, 2013, 13(7): 823–829. DOI:10.1016/j.spinee.2013.03.009 |
 2019, Vol.17
2019, Vol.17  Issue(2): 73-78
Issue(2): 73-78


