2. 上海交通大学医学院附属第六人民医院骨科, 上海 200233
2. Department of Orthopaedics, Sixth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200233, China
多节段脊髓型颈椎病(MCSM)是脊柱外科常见疾病,但有效处理MCSM仍较为困难[1-2]。目前,后路单开门椎管扩大椎板成形术是MCSM首选治疗方法[3]。传统的单开门手术是通过缝线捆绑以维持椎板的开门状态,但这一方法可能出现软组织撕裂或缝线断裂导致门轴侧骨不连及椎板再关门等现象,影响疗效[4-5]。为了防止术后椎板再关门,本研究采用后路单开门椎管扩大椎板成形术联合Neulen钛板内固定治疗MCSM,疗效满意,现报告如下。
1 资料与方法 1.1 一般资料回顾性分析2012年7月—2016年7月,在上海交通大学医学院附属第六人民医院接受后路单开门椎管扩大椎板成形术联合Neulen钛板内固定治疗且随访资料完整的MCSM患者61例,其中男40例、女21例,年龄42 ~ 75(57.4±13.9)岁;病程1 ~ 3(1.4±0.6)年。病变节段:C3~5 9例、C3~6 7例、C4~7 7例、C3~7 38例。所有患者均表现为双侧上肢无力、步态不稳、颈肩部疼痛;59例步态蹒跚、肌张力高、腱反射亢进、双手Hoffmann征(+);34例双侧Babinski征(+)。所有患者术前X线、CT及MRI检查均与临床症状、体征相符。X线片示患者均存在退行性颈椎椎管狭窄,MRI及CT示多节段椎间盘突出、脊髓多节段受压,黄韧带增生肥厚45例、后纵韧带骨化13例。所有患者均为初次手术,无脊髓炎。
1.2 手术方法患者气管插管全身麻醉,俯卧于特制石膏床上,维持颈椎伸展中立位。术野常规消毒,铺无菌巾单,常规做后正中切口,逐层切开,显露C3~7椎板、小关节突,咬除相应节段1/3上棘突。以症状重的一侧作为开门侧,对侧为门轴侧。用磨钻沿双侧小关节突内缘2.5 mm处开槽,门轴侧仅磨除外层骨皮质,开门侧磨透内外层骨皮质;缓慢、轻柔地将椎板向门轴侧掀起,掀起过程中用神经剥离子解除粘连;用枪钳咬除黄韧带,以获得完全开门,切断开门节段上下两端椎板及黄韧带,以彻底减压(可见硬膜囊后移搏动明显)。根据开门大小选择合适的Neulen钛板固定在掀开的椎板和对应的侧块处,每枚Neulen钛板均采用4枚螺钉固定。观察切口内无活动性出血后冲洗切口,放置负压引流管1根,逐层缝合切口。
1.3 围手术期处理切皮前30 min及术后1 d静脉注射五水头孢唑啉钠2 g。术后常规应用甲泼尼龙、脱水及神经营养药物3 ~ 6 d。根据引流情况,一般术后48 h拔除引流管,鼓励患者在颈托制动下离床活动,行四肢功能锻炼,颈托制动4周后适度行颈部功能锻炼。
1.4 观察指标记录出血量(术中出血量及术后引流量)、手术时间、日本骨科学会(JOA)评分(17分法)[6]、神经功能改善率[(术后JOA评分-术前JOA评分)/(17-术前JOA评分)×100%]、颈椎椎管矢状径(C5椎管矢状径)、椎管扩大率[(术后椎管矢状径-术前椎管矢状径)/术前椎管矢状径×100%]、门轴侧骨愈合情况、颈椎轴性症状(包括颈后部疼痛、颈后部僵硬、肩部疼痛、肩部僵硬等4项,满分12分,1 ~ 3分为优、4 ~ 6分为良、7 ~ 9分为可、10 ~ 12分为差,可、差提示存在颈椎轴性症状[7])及围手术期并发症。
1.5 统计学处理应用SPSS 18.0软件对数据进行统计学分析,计量资料以x±s表示,手术前后比较采用配对t检验;以P < 0.05为差异有统计学意义。
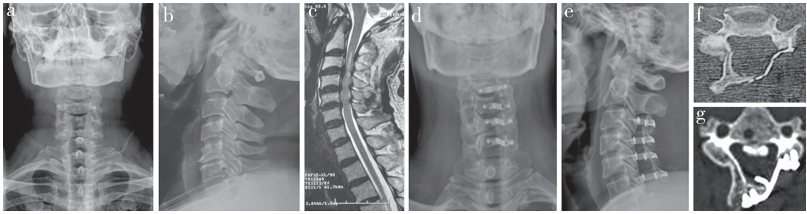
2 结果所有手术均顺利完成,无切口感染、脑脊液漏、脊髓损伤、C5神经根麻痹等并发症。所有患者随访2 ~ 5(3.4±1.9)年,手术时间为80 ~ 145(112.4±22.8)min,出血量为280 ~ 650(322.8±92.8)mL。JOA评分由术前的7 ~ 13(9.8±2.8)分提高到末次随访时的11 ~16(15.2±1.9)分;末次随访时神经功能改善率为58.2% ~ 81.5%[(75.3±9.7)%]。术后6个月时轴性症状评分为1 ~ 10(5.7±3.1)分,优31例、良23例、可5例、差2例;末次随访时轴性症状评分为1 ~ 7(3.2±1.5)分,优35例、良25例、可1例。颈椎椎管矢状径由术前的6 ~ 11(8.5±1.4)mm扩大到术后的12.6 ~ 17.9(15.1±2.3)mm,椎管扩大率为68.2% ~ 83.1%[(77.6±6.8)%]。所有患者门轴侧椎板均获得骨愈合,无内固定断裂、松动及再关门现象发生。典型病例影像学资料见图 1。
|
a,b:术前正侧位X线片示颈椎退行性变 c:术前MRI示C2~5后纵韧带骨化 d,e:术后正侧位X线片示内固定位置良好 f:术后CT示椎管扩大,内固定位置良好 g:末次随访时CT示门轴侧椎板融合,内固定无松动 a, b:Preoperative lateral and anteroposterior roentgenographs show cervical degeneration c:Preoperative MRI shows C2-5 ossification of posterior longitudinal ligament d, e:Postoperative lateral and anteroposterior roentgenographs show internal fixation in good position f:Postoperative CT shows enlargement of spinal canal and good position of internal fixation g:CT at final follow-up shows lateral lamina of portal axis is fused without loosening of internal fixation 图 1 典型病例影像学资料 Figure 1 Imaging data of a typical case |
手术治疗MCSM的目的是解除脊髓压迫,改善颈椎功能,维持正常的颈椎序列。颈椎后路单开门椎管扩大椎板成形术可扩大椎管前后径,增加椎管容积,通过“弓弦原理”使脊髓后移,缓解脊髓来自于前方的压迫,从而有效恢复脊髓血流灌注,改善脊髓功能,最终达到治疗MCSM的目的[8]。有研究表明,传统颈椎单开门椎管扩大椎板成形术治疗MCSM短期疗效较好,但长期随访可出现门轴侧椎板部分愈合或不愈合、术后再关门等并发症,影响疗效[9]。传统方法是采用粗线将掀起的椎板固定在小关节囊上,而缝线强度有限,在颈部肌肉收缩及颈后部外力作用下,可发生缝线断裂或软组织撕裂,使椎板处于不稳定状态,影响门轴侧椎板融合,导致“再关门”现象发生[10]。
本组病例均未发生再关门现象,门轴侧椎板均融合,神经功能改善率为(75.3±9.7)%,椎管扩大率为(77.6±6.8)%,证实后路单开门椎管扩大椎板成形术联合Neulen钛板内固定治疗MCSM可以增大椎管容积,解除脊髓压迫,防止“再关门”现象发生,临床疗效满意。既往研究也表明,相比传统后路单开门椎管扩大椎板成形术,联合钛板内固定具有为开门椎板提供即刻稳定及早期支撑作用,有利于门轴侧椎板融合,从而有效维持椎管扩张状态[5]。
轴性症状是颈椎后路单开门椎管扩大椎板成形术后常见并发症,有学者认为术后颈部制动时间过久、颈部肌肉活动不足,是引起颈椎轴性症状的重要原因[11]。本研究中7例患者出现轴性症状,至末次随访,6例轴性症状消失,1例获得缓解。Neulen钛板是特制固定钛板,不仅具有良好的强度和韧性,而且生物相容性较高,固定后可有效提高椎板的即刻稳定性,为门轴侧骨愈合提供了良好的条件,且缩短了颈部制动时间,有利于患者早期进行颈部功能锻炼,从而减少轴性疼痛等并发症的发生[12]。另外,Neulen钛板在开门侧的阻挡及支撑固定,既可避免瘢痕组织对脊髓造成压迫,又可避免“再关门”现象的发生[13]。Neulen钛板还可避免刺激损伤颈神经后支,且钉-板可有效固定同侧侧块与掀起的椎板,使同一节段的侧块和椎板成为一个整体,最终达到刚性固定的目的。
综上所述,采用后路单开门椎管扩大椎板成形术联合Neulen钛板内固定治疗MCSM,可获得满意的临床疗效,具有即刻稳定开门椎板、有利于门轴侧椎板融合、维持椎管扩张状态、防止“再关门”现象发生等优点。
| [1] |
Tong MJ, Hu YB, Wang XY, et al. The spinal cord line can predict postoperative recovery for multilevel cervical spondylotic myelopathy[J]. World Neurosurg, 2017, 104: 361-366. DOI:10.1016/j.wneu.2017.03.105 |
| [2] |
Lau D, Winkler EA, Than KD, et al. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy:influence of cervical alignment on outcomes[J]. J Neurosurg Spine, 2017, 27(5): 508-517. DOI:10.3171/2017.4.SPINE16831 |
| [3] |
Arrojas A, Jackson JB 3rd, Grabowski G. Trends in the treatment of single and multilevel cervical stenosis:a review of the american board of orthopaedic surgery database[J]. J Bone Joint Surg Am, 2017, 99(18): e99. DOI:10.2106/JBJS.16.01082 |
| [4] |
Minamide A, Yoshida M, Simpson AK, et al. Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy:5-year follow-up study[J]. J Neurosurg Spine, 2017, 27(4): 403-409. DOI:10.3171/2017.2.SPINE16939 |
| [5] |
鲍达, 于龙, 李大伟, 等. 两种固定方法在颈椎单开门椎管扩大椎板成形术中的比较研究[J]. 脊柱外科杂志, 2017, 15(5): 262-267. DOI:10.3969/j.issn.1672-2957.2017.05.002 |
| [6] |
Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890-1895. DOI:10.1097/00007632-200109010-00014 |
| [7] |
张仁赞, 张学利, 胡炜, 等. EOLP不同椎板固定方法对颈椎曲度及轴性症状的影响[J]. 重庆医学, 2016, 45(6): 782-786. DOI:10.3969/j.issn.1671-8348.2016.06.019 |
| [8] |
唐向盛, 谭明生, 移平, 等. 改良法单开门椎管扩大椎板成形术治疗颈椎后纵韧带骨化症合并颈椎不稳的疗效评价[J]. 脊柱外科杂志, 2018, 16(1): 3-7. DOI:10.3969/j.issn.1672-2957.2018.01.002 |
| [9] |
Li Z, Wang H, Tang J, et al. Comparison of three reconstructive techniques in the surgical management of patients with four-level cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976), 2017, 42(10): E575-E583. DOI:10.1097/BRS.0000000000001907 |
| [10] |
Michael KW, Neustein TM, Rhee JM. Where should a laminoplasty start? The effect of the proximal level on post-laminoplasty loss of lordosis[J]. Spine J, 2016, 16(6): 737-741. DOI:10.1016/j.spinee.2016.01.188 |
| [11] |
Tamai K, Suzuki A, Terai H, et al. Laminar closure after expansive open-door laminoplasty:fixation methods and cervical alignments impact on the laminar closure and surgical outcomes[J]. Spine J, 2016, 16(9): 1062-1069. DOI:10.1016/j.spinee.2016.04.018 |
| [12] |
Bai C, Li K, Guo A, et al. Indication for hypertrophy posterior longitudinal ligament removal in anterior decompression for cervical spondylotic myelopathy[J]. Medicine(Baltimore), 2017, 96(23): e7043. |
| [13] |
Takeshima Y, Matsuoka R, Nakagawa I, et al. Surgical outcome of laminoplasty for cervical spondylotic myelopathy in an elderly population-potentiality for effective early surgical intervention:a meta-analysis[J]. Neurol Med Chir(Tokyo), 2017, 57(7): 366-373. |
 2019, Vol.17
2019, Vol.17  Issue(3): 168-171
Issue(3): 168-171


