2. 延安大学医学院研究生院, 延安 716000;
3. 宁夏医科大学总医院脊柱外科, 银川 750004
2. Graduate School, Medical College of Yan'an University, Yan'an 716000, Shaanxi, China;
3. Department of Spinal Surgery, General Hospital of Ningxia Medical University, Yinchuan 750004, Ningxia Hui Autonomous Region, China
脊柱退行性疾病是引起慢性腰腿痛的常见原因,近年脊柱矢状位结构在疾病诊治中逐渐得到关注[1-2],了解脊柱矢状位结构可指导脊柱退行性疾病的治疗并有助于评估疗效[3-6]。目前临床上用于评估脊柱矢状位结构的参数系统主要有骨盆投射角(PI)系统和骨盆半径(PR)技术,在退行性腰椎滑脱(DLS)与退行性腰椎椎管狭窄症(DSS)患者脊柱矢状位结构及代偿机制的研究中运用较为广泛的是PI系统,但Jackson等[7]提出PR技术中的总腰椎骨盆前凸角(PR-T12)参数用于评估脊柱-矢状位平衡,比基于铅垂线的脊柱矢状面平衡(SVA)参数更可靠。本研究主要应用PR技术分析DLS与DSS患者脊柱-骨盆参数的特点,比较DLS与DSS患者的脊柱矢状位结构差异并探讨其代偿机制。
1 资料与方法 1.1 一般资料对2015年9月—2017年8月宁夏医科大学总医院脊柱外科收治的DLS和DSS患者的临床、影像学资料进行回顾性分析。纳入标准:①临床诊断为DLS或DSS;②影像学资料完整。排除标准:①合并其他脊柱疾病,如脊柱外伤、结核、肿瘤、侧凸、峡部裂伴/不伴滑脱等;②有脊柱手术史;③下肢严重的骨关节炎或残疾。DLS诊断标准:上下椎体间发生相对滑移,但椎弓未发生断裂[8]。DSS诊断标准:影像学资料示腰椎椎管狭窄(椎管矢状径 < 10 mm和/或侧隐窝前后径 < 3 mm)[9-10],结合临床症状(神经源性间歇性跛行),同时排除脊髓和血管源性间歇性跛行。
根据以上标准,共纳入患者71例。DLS组36例,男2例、女34例,年龄46 ~ 83(61.1±8.6)岁,L4椎体滑脱32例(Ⅰ度31例、Ⅱ度1例)、L5椎体滑脱4例(Ⅰ度3例、Ⅱ度1例);DSS组35例,男22例、女13例,年龄40 ~ 81(60.5±9.6)岁。
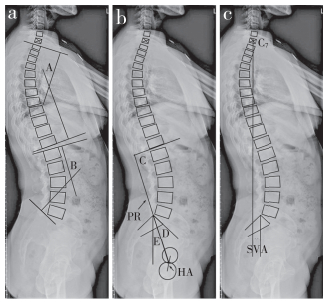
1.2 影像学测量在站立位全脊柱侧位X线片上测量各参数。脊柱参数:SVA、腰椎前凸(LL)和胸椎后凸(TK);PR参数:PR-T12、骨盆形态(PR-S1)和骨盆角(PA);并与健康国人脊柱-骨盆参数进行比较。比较PR-T12与各参数间的相关性,明确DLS和DSS患者脊柱矢状位结构的代偿机制。
国人健康脊柱-骨盆矢状位参数值参考文献[12]。所有参数均由3位医师独立测量,取平均值,具体测量方法见图 1。SVA,即经C7椎体中点的纵垂线与骶骨后上角之间的水平距离,垂线在骶骨后上角前为正值,| SVA |≥50 mm为矢状面失衡[13]。LL,即L1椎体上终板切线与骶骨终板切线间的夹角。TK,即T1椎体上终板切线与T12椎体下终板切线间的夹角。髋轴(HA),即双侧股骨头中心连线的中点;骨盆半径(PR),即HA和骶骨后上角的连线;PR-T12,即PR与T12下终板切线间的夹角;PR-S1,即PR与骶骨终板切线间的夹角;PA,即PR与纵垂线间的夹角。
|
a:TK(∠A)和LL(∠B)测量b:PR-T12(∠C),PR-S1(∠D)和PA(∠E)测量c:SVA测量 a:Measurement of TK(∠A) and LL(∠B) b:Measurement of PR-T12(∠C), PR-S1(∠D) and PA(∠E) c:Measurement of SVA 图 1 脊柱-骨盆矢状位参数测量 Figure 1 Measurement of sagittal spinopelvic parameters |
所有数据均采用SPSS 17.0软件进行统计学分析,采用独立样本t检验比较2组病例脊柱-骨盆参数与健康国人参数的差异,采用Pearson相关分析研究2组病例脊柱-骨盆参数之间的相关性;以P < 0.05为差异有统计学意义。
2 结果DLS组中4例矢状面失衡,DSS组中8例矢状面失衡。DLS组与DSS组中的SVA、PA均明显大于正常参考值,差异有统计学意义(P < 0.05,表 1)。DSS组PR-T12明显小于正常参考值,DLS组的PR-S1明显小于正常参考值,差异均有统计学意义(P < 0.05,表 1)。DLS组PR-T12与PA的相关性强于与LL、TK的相关性,DSS组PR-T12与LL、TK的相关性强于与PA的相关性(表 2);且DLS组PR-S1与PA呈负相关,DSS组PR-S1与PA无相关性(表 3)。
|
|
表 1 2组脊柱-骨盆矢状位参数与国内正常值比较 Table 1 Comparison of sagittal spinepelvic parameters between 2 groups and normal population |
|
|
表 2 PR-T12与各参数间相关性比较 Table 2 Comparison of correlation between PR-T12 and sagittal parameters |
|
|
表 3 PR-S1与各参数间相关性比较 Table 3 Comparison of correlation between PR-S1 and sagittal parameters |
矢状位平衡是机体在最小的肌肉能量消耗下维持稳定站立的一种状态,衡量全脊柱矢状位平衡较为常用的参数是SVA[14-17]。DLS组和DSS组的SVA值均明显大于国内正常参考值,表明DLS和DSS患者与健康国人相比,均有躯干前倾的表现。因为脊柱与骨盆相连接,脊柱矢状位序列的变化势必引起骨盆空间位置的改变[18]。Chanplakorn等[19]认为PA可以描述骨盆的空间位置,本研究也发现DLS和DSS患者的PA值较国内正常参考值均明显增大,表明DLS和DSS患者与健康国人相比,均有骨盆后倾的表现。因此推测,随着脊柱退行性改变逐渐加重,脊柱稳定性逐渐降低,为了维持矢状位的平衡,DLS与DSS患者通过躯干前倾及骨盆后倾使脊柱稳定。
脊柱参数及骨盆参数在维持脊柱矢状位平衡中是密不可分的[20],单独考虑脊柱或者骨盆参数容易忽视脊柱与骨盆相互之间的代偿作用。PR-T12反映总腰椎-骨盆前凸,在健康个体中是一个相对稳定的参数[11]。Sergides等[11]提出PR-T12在评估脊柱-骨盆矢状位平衡时患者胸腰曲度比值应为0.15 ~ 0.75,本研究所有的病例均符合该标准(DLS组胸腰曲度比值0.62±0.13,DSS组胸腰曲度比值0.64±0.10)。本研究发现,DLS组PR-T12与国内正常参考值相比,差异无统计学意义,而DSS组PR-T12与国内正常参考值相比明显减小,提示DLS与DSS患者虽然都通过躯干前倾和骨盆后倾来维持脊柱-骨盆矢状位平衡,但其脊柱-骨盆矢状位结构表现并不完全相同。
本研究发现,在DLS组中PR-T12与PA的相关性强于与LL、TK的相关性,而在DSS组中PR-T12与LL、TK的相关性强于与PA的相关性,所以推测DLS患者主要通过骨盆后倾维持脊柱矢状位平衡,DSS患者主要通过改变胸腰椎曲度维持脊柱矢状位平衡。Chanplakorn等[19]认为,PR-S1与骶股距(HA与骶骨后上角之间的水平距离)呈负相关,当PR-S1减小时,骶股距增加,PA增大;PR-S1增大时,PA相对减小。本研究发现,DLS患者PR-S1明显小于DSS患者及国内正常参考值,且与PA呈负相关;DSS患者PR-S1与国内正常参考值差异无统计学意义,且与PA无相关性,推测DLS患者主要通过骨盆后倾维持脊柱-骨盆矢状位平衡,而在DSS患者中骨盆后倾维持脊柱矢状位平衡的作用较小,进而推测改变胸腰椎曲度可能是DSS患者维持脊柱矢状位平衡的主要代偿机制。
综上所述,为了维持脊柱矢状位的平衡,DLS与DSS患者脊柱-骨盆矢状面参数的代偿过程中可能具有不同的机制。DLS患者可能主要通过骨盆后倾维持脊柱矢状位平衡,DSS患者可能主要通过改变胸腰椎曲度维持脊柱矢状位平衡。但研究样本量较小,未进行性别匹配,同时DLS病例为轻度滑脱;因此,本研究结论有待于进一步研究来验证。
| [1] |
王亮, 卢旭华, 王海滨, 等. 退变性腰椎侧凸脊柱-骨盆参数测量及临床意义[J]. 脊柱外科杂志, 2016, 14(1): 39-43. DOI:10.3969/j.issn.1672-2957.2016.01.009 |
| [2] |
马振江, 赵长清, 田建平, 等. 改良腰骶角评估骨盆前倾复位技术在儿童重度L5滑脱治疗中的应用[J]. 脊柱外科杂志, 2016, 14(1): 21-25. DOI:10.3969/j.issn.1672-2957.2016.01.005 |
| [3] |
Gille O, Challier V, Parent H, et al. Degenerative lumbar spondylolisthesis:cohort of 670 patients, and proposal of a new classification[J]. Orthop Traumatol Surg Res, 2014, 100(6 Suppl): S311-S315. |
| [4] |
Lee BH, Yang JH, Kim HS, et al. Effect of sagittal balance on risk of falling after lateral lumbar interbody fusion surgery combined with posterior surgery[J]. Yonsei Med J, 2017, 58(6): 1177-1185. DOI:10.3349/ymj.2017.58.6.1177 |
| [5] |
Ilharreborde B. Sagittal balance and idiopathic scoliosis:does final sagittal alignment influence outcomes, degeneration rate or failure rate?[J]. Eur Spine J, 2018, 27(Suppl 1): 48-58. |
| [6] |
Hikata T, Watanabe K, Fujita N, et al. Impact of sagittal spinopelvic alignment on clinical outcomes after decompression surgery for lumbar spinal canal stenosis without coronal imbalance[J]. J Neurosurg Spine, 2015, 23(4): 451-458. DOI:10.3171/2015.1.SPINE14642 |
| [7] |
Jackson RP, Kanemura T, Kawakami N, et al. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain[J]. Spine(Phila Pa 1976), 2000, 25(5): 575-586. DOI:10.1097/00007632-200003010-00008 |
| [8] |
盛亚超, 孙旭, 朱泽章, 等. 退变性腰椎滑脱French分型和CARDS分型的可重复性与可信度研究[J]. 中国脊柱脊髓杂志, 2017, 27(3): 228-234. DOI:10.3969/j.issn.1004-406X.2017.03.06 |
| [9] |
Lee JKT.体部CT[M].周康荣, 程家文, 译.武汉: 湖北科学技术出版社, 1990: 35.
|
| [10] |
叶华, 段承祥. CT测量椎管的评价[J]. 第二军医大学学报, 1990, 11(1): 78. DOI:10.3321/j.issn:0258-879X.1990.01.032 |
| [11] |
Sergides IG, McCombe PF, White G, et al. Lumbopelvic lordosis and the pelvic radius technique in the assessment of spinal sagittal balance:strengths and caveats[J]. Eur Spine J, 2011, 20(Suppl 5): 591-601. |
| [12] |
尹刚辉, 金大地, 陈方尧, 等. 新的脊柱-骨盆矢状面测量参数:骶骨骨盆角的提出及意义[J]. 中国脊柱脊髓杂志, 2014, 24(8): 704-709. DOI:10.3969/j.issn.1004-406X.2014.08.07 |
| [13] |
Lamartina C, Berjano P, Petruzzi M, et al. Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis[J]. Eur Spine J, 2012, 21(Suppl 1): 27-31. |
| [14] |
Fechtenbaum J, Etcheto A, Kolta S, et al. Sagittal balance of the spine in patients with osteoporotic vertebral fractures[J]. Osteoporos Int, 2016, 27(2): 559-567. DOI:10.1007/s00198-015-3283-y |
| [15] |
Tamai K, Suzuki A, Takahashi S, et al. Validity and reproducibility of various measurement methods for craniocervical sagittal balance[J]. Clin Spine Surg, 2018, 31(2): 80-85. DOI:10.1097/BSD.0000000000000617 |
| [16] |
Theologis AA, Mundis GM Jr, Nguyen S, et al. Utility of multilevel lateral interbody fusion of the thoracolumbar coronal curve apex in adult deformity surgery in combination with open posterior instrumentation and L5-S1 interbody fusion:a case-matched evaluation of 32 patients[J]. J Neurosurg Spine, 2017, 26(2): 208-219. DOI:10.3171/2016.8.SPINE151543 |
| [17] |
Radovanovic I, Urquhart JC, Ganapathy V, et al. Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis[J]. J Neurosurg Spine, 2017, 26(4): 448-453. DOI:10.3171/2016.9.SPINE1680 |
| [18] |
Zhao Y, Shen CL, Zhang RJ, et al. Sagittal pelvic radius in low-grade isthmic lumbar spondylolisthesis of Chinese population[J]. J Korean Neurosurg Soc, 2016, 59(3): 292-295. DOI:10.3340/jkns.2016.59.3.292 |
| [19] |
Chanplakorn P, Wongsak S, Woratanarat P, et al. Lumbopelvic alignment on standing lateral radiograph of adult volunteers and the classification in the sagittal alignment of lumbar spine[J]. Eur Spine J, 2011, 20(5): 706-712. DOI:10.1007/s00586-010-1626-0 |
| [20] |
Makhni MC, Shillingford JN, Laratta JL, et al. Restoration of sagittal balance in spinal deformity surgery[J]. J Korean Neurosurg Soc, 2018, 61(2): 167-179. DOI:10.3340/jkns.2017.0404.013 |
 2019, Vol.17
2019, Vol.17  Issue(3): 207-210
Issue(3): 207-210

