2. 镇江瑞康医院麻醉科, 镇江 212001
2. Department of Anesthesiology, Zhenjiang Ruikang Hospital, Zhenjiang 212001, Jiangsu, China
自Kambin三角[1]被首次报道后, 经椎间孔入路经皮内窥镜技术在椎间盘突出症的治疗中得到广泛应用, 并在实践中证实了其安全性、有效性[2-4]。经椎间孔入路和经椎板间入路是内窥镜技术常用的2种入路。L5/S1节段由于高髂嵴、肥大横突等特殊解剖结构使侧路经椎间孔入路存在一定的困难和风险, 而L5/S1椎板间宽大的解剖间隙使经椎板间入路成为内窥镜技术的有益补充[5-7]。由于经椎板间入路需要经过椎管, 难以避免对神经根产生刺激, 导致患者术中疼痛明显, 因此, 术中麻醉方式的选择很重要。为探讨术中采用不同麻醉方式是否会影响术后疗效, 2012年12月—2015年12月, 本院骨科采用经椎板间入路经皮内窥镜下椎间盘切除术(PEID)治疗L5/S1椎间盘突出症患者63例, 术中分别采用局部浸润麻醉和连续硬膜外麻醉, 对比术后疗效, 现报告如下。
1 资料与方法 1.1 一般资料纳入标准:L5/S1单节段椎间盘突出症; 非手术治疗1个月无效。排除标准:极外侧突出, 肿瘤, 腰椎失稳、滑脱, 背部皮肤软组织感染, 急性马尾综合征。所有患者术前均签署手术和麻醉知情同意书, 本研究通过本院伦理委员会批准。按照上述标准纳入L5/S1椎间盘突出症患者63例, 均行PEID治疗, 31例术中采用局部浸润麻醉(A组), 其中男12例、女19例, 年龄17 ~ 61(36.0±13.6)岁, 症状侧为左侧15例、右侧16例; 32例术中采用连续硬膜外麻醉(B组), 其中男15例、女17例, 年龄18 ~ 67(39.5±14.2)岁, 症状侧为左侧13例、右侧19例。2组患者术前一般情况相当, 具有可比性。
1.2 手术方法2组手术均由具备内窥镜手术经验的同一组医师完成。A组在透视定位后, 采用1.0%盐酸利多卡因注射液10 mL分层浸润麻醉, 药物须深入椎板间, 避免穿破黄韧带。应用间接破黄方式, 在黄韧带打开后, 神经探钩清理硬膜外脂肪, 暴露神经根或硬膜囊, 抽出手术通道内的生理盐水, 在硬膜外腔注入2.0%利多卡因注射液2 mL, 等待5 min后再行椎间盘探查和处理。B组患者选择L1/L2或L2/L3椎间隙采用0.5%罗哌卡因进行连续硬膜外麻醉, 透视定位后采用间接破黄法进入椎管, 处理椎间盘, 进行后续手术操作, 完成手术后拔出硬膜外管。2组患者术后6 h后可酌情佩戴腰围下床活动, 给予脱水及营养神经药物治疗3 d后出院, 指导卧床行直腿抬高锻炼, 4周内禁止久坐、弯腰, 4周后行腰背肌功能锻炼。
1.3 观察指标记录2组患者手术时间、透视时间、术中满意度以及并发症发生情况。采用疼痛视觉模拟量表(VAS)评分[8]、Oswestry功能障碍指数(ODI)[9]评价手术疗效。术中满意度根据患者术中疼痛程度评定, 分为完全无痛、轻度疼痛、中度疼痛(可忍受)及重度疼痛(需暂停手术给予对症处理), 完全无痛及轻度疼痛为满意, 中重度疼痛为不满意。
1.4 统计学处理采用SPSS 22.0软件对数据资料进行统计学分析, 采用t检验进行差异比较; 以P < 0.05为差异有统计学意义。
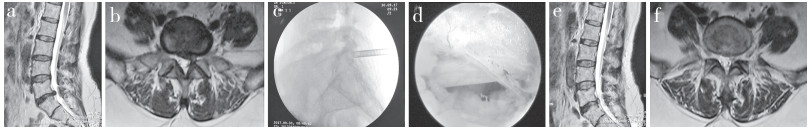
2 结果所有手术顺利完成, 随访18 ~ 24(20.0±2.5)个月。2组患者末次随访时VAS评分、ODI均较术前显著改善, 差异均有统计学意义(P < 0.05, 表 1), 但组间比较差异无统计学意义(P > 0.05);2组患者手术时间、透视时间相比差异无统计学意义(P > 0.05, 表 1)。A组患者中完全无痛13例, 轻度疼痛13例, 中度疼痛3例, 重度疼痛2例; B组患者中完全无痛25例, 轻度疼痛5例, 中度疼痛1例, 重度疼痛1例; B组患者术中满意度明显优于A组, 差异有统计学意义(P < 0.05)。2组均无脑脊液漏、硬膜囊损伤、感染等并发症发生, 且随访期间无复发。典型病例影像学资料见图 1。
|
|
表 1 统计资料 Table 1 Statistical information |
|
a, b:术前T2WI MRI示L5/S1椎间盘突出, 神经根及硬膜囊受压c:工作套管置于黄韧带表面d:镜下可见S1神经根压迫解除e, f:术后1个月MRI示突出椎间盘摘除后, 神经根、硬膜囊压迫解除 a, b:Preoperative T2WI MRIs show L5/S1 disc herniation and compression of nerve root and dural sac c:Cannula is placed to ligamentum flavum surface d:S1 nerve root compression is relieved under endoscope e, f:MRIs at postoperative 1 month show that compression of nerve root and dural sac is relieved after herniated intervertebral disc is removed 图 1 典型病例影像学资料 Figure 1 Imaging data of a typical case |
内窥镜技术已成为治疗椎间盘突出症的有效手段, 并逐渐普及, 其软组织损伤小, 恢复快, 并发症少等优势已被多数医师所认可。内窥镜技术常分为经椎间孔入路和经椎板间入路, 在L5/S1节段, 部分高髂嵴、宽大横突、髓核向下游离等特殊病例中[10-12], 椎板间入路有其特殊的优势, 即使遇到中央型大块突出或侧隐窝处突出, 也可用扩大小关节突内侧缘来完成手术[13-14]。
在术中麻醉方式选择方面, 有全身麻醉、硬膜外麻醉、腰麻、局部浸润麻醉等[15]; 由于基层医院需考虑麻醉费用及术中神经根损伤的可控性, 往往不选择全身麻醉和腰麻[16]。连续硬膜外麻醉和局部浸润麻醉相对安全[17], 且行之简便。本研究中, 2组患者末次随访时VAS评分、ODI均较术前显著改善, 且均无手术并发症发生, 2组疗效相当, 说明术中采用不同麻醉方式并不影响PEID的临床疗效。
本研究中, A组患者术中满意度为83.87%(26/31), B组为93.75%(30/32), 考虑原因可能为B组采用0.5%罗哌卡因注射液阻断手术操作区域的感觉, 保留下肢活动, 术中可监控神经根的损伤情况, 及时调整手术操作; 但也可能是患者对疼痛耐受程度, 术中对神经根刺激的程度, 椎管内容积, 椎间盘突出类型, 麻醉类型、方式, 麻醉药物用量及手术时间等个体差异原因。为了缓解患者疼痛, 增加术中满意度, 在行黄韧带开窗后, 可采用2.0%利多卡因注射液2 mL注入硬膜外腔隙, 5 min后再次开始手术, 以缓解神经根对外来手术工具的刺激和充分减压[18]; 也可配合静脉使用右美托咪定0.5μg/(kg·h-1), 改善患者紧张、恐惧情绪。
综上, PEID能彻底取出突出的椎间盘, 使神经根得到充分减压[19-20], 且术中采用局部浸润麻醉或连续硬膜外麻醉不影响其术后疗效, 只要处理得当, 皆可获得满意的手术效果。但本研究样本量较小, 且患者本身对疼痛耐受程度存在个体差异, 不同麻醉医师硬膜外麻醉控制水平也有差异, 可能会导致本研究存在一定局限性, 尚需大样本、多中心研究进一步进行验证。
| [1] |
Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results[J]. Clin Orthop Relat Res, 1986, 207: 37-43. |
| [2] |
Sencer A, Yorukoglu AG, Akcakaya MO, et al. Fully endoscopic interlaminar and transforaminal lumbar discectomy:short-term clinical results of 163 surgically treated patients[J]. World Neurosurg, 2014, 82(5): 884-890. DOI:10.1016/j.wneu.2014.05.032 |
| [3] |
Phan K, Xu J, Schultz K, et al. Full-endoscopic versus micro-endoscopic and open discectomy:a systematic review and meta-analysis of outcomes and complications[J]. Clin Neurol Neurosurg, 2017, 154: 1-12. DOI:10.1016/j.clineuro.2017.01.003 |
| [4] |
Li ZZ, Hou SX, Shang WL, et al. The strategy and early clinical outcome of full-endoscopic L5/S1 discectomy through interlaminar approach[J]. Clin Neurol Neurosurg, 2015, 133: 40-45. DOI:10.1016/j.clineuro.2015.03.003 |
| [5] |
Li XC, Zhong CF, Deng GB, et al. Full-endoscopic procedures versus traditional discectomy surgery for discectomy:a systematic review and meta-analysis of current global clinical trials[J]. Pain Physician, 2016, 19(3): 103-118. |
| [6] |
Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation:transforaminal versus interlaminar approach[J]. Pain Physician, 2013, 16(6): 547-556. |
| [7] |
Min JH, Kang SH, Lee JB, et al. Morphometric analysis of the working zone for endoscopic lumbar discectomy[J]. J Spinal Disord Tech, 2005, 18(2): 132-135. DOI:10.1097/01.bsd.0000159034.97246.4f |
| [8] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [9] |
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271-273. |
| [10] |
Choi G, Lee SH, Raiturker PP, et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigidworking channel endoscope[J]. Neurosurgery, 2006, 58(1 Suppl): 59-68. |
| [11] |
Ruetten S, Komp M, Merk H, et al. Use of newly developed instrumentsand endoscopes:full-endoscopic resec-tion of lumbar disc herniations via theinterlaminar and lateral transforaminal approach[J]. J Neurosurg Spine, 2007, 6(6): 521-530. DOI:10.3171/spi.2007.6.6.2 |
| [12] |
Ruetten S, Komp M, Merk H, et al. Recurrent lumbar disc herniation after conventional discectomy:a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision[J]. J Spinal Disord Tech, 2009, 22(2): 122-129. DOI:10.1097/BSD.0b013e318175ddb4 |
| [13] |
Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation:transforaminal versus inter-laminar approach[J]. Pain Physician, 2013, 16(6): 547-556. |
| [14] |
Ruetten S, Komp M, Merk H, et al. Full-endoscopic in terlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique:a prospective, randomized, controlled study[J]. Spine(Phila Pa 1976), 2008, 33(9): 931-939. DOI:10.1097/BRS.0b013e31816c8af7 |
| [15] |
Wang SJ, Chen BH, Wang P, et al. The effect of percutaneous endoscopic lumbar discectomy under different anesthesia on pain and immunity of patients with prolapse of lumbar intervertebral disc[J]. Eur Rev Med Pharmacol Sci, 2017, 21(12): 2793-2799. |
| [16] |
Chen HT, Tsai CH, Chao SC, et al. Endoscopic discectomy of L5-S1 disc herniation via an interlaminar approach:prospective controlled study under local and general anesthesia[J]. Surg Neurol Int, 2011, 2: 93. DOI:10.4103/2152-7806.82570 |
| [17] |
Fang G, Ding Z, Song Z. Comparison of the effects of epidural anesthesia and local anesthesia in lumbar transforaminal endoscopic surgery[J]. Pain Physician, 2016, 19(7): E1001-E1004. |
| [18] |
蒋虎山, 曾建成, 王亮, 等. 黄韧带劈开与开窗在经椎板间入路经皮内窥镜下椎间盘切除术中的比较[J]. 脊柱外科杂志, 2015, 13(6): 327-332. DOI:10.3969/j.issn.1672-2957.2015.06.003 |
| [19] |
Ruetten S, Komp M, Godolias G. A new full-endoscopic technique for the interlaminar operation of lumbar disc hernia-tions using 6-mm endoscopes:prospective 2-year results of 331 patients[J]. Minim Invas Neurosur, 2006, 49(2): 80-87. DOI:10.1055/s-2006-932172 |
| [20] |
刘郁林, 常跃文, 刘粤, 等. 改良经椎板间入路经皮内窥镜下减压术治疗退行性腰椎椎管狭窄[J]. 脊柱外科杂志, 2016, 14(6): 340-344. DOI:10.3969/j.issn.1672-2957.2016.06.005 |
 2019, Vol.17
2019, Vol.17  Issue(4): 248-251
Issue(4): 248-251


