后路颈椎椎板成形术是治疗多节段脊髓型颈椎病(CSM)的主要术式[1]。对于颈椎生理曲度尚存的颈椎病患者,椎板成形术可以使脊髓向后方充分漂移,解除脊髓前后方压迫[2-3]。传统椎板成形术选择C3~7为手术节段,手术效果良好,但对颈椎后部肌肉、韧带造成不同程度的破坏,导致术后出现颈椎活动度(ROM)降低、矢状位平衡(SVA)改变、C5神经根麻痹和轴性症状等并发症[4-7]。传统椎板成形术通常切开分离在C2棘突上附着的颈半棘肌和在C7棘突上附着的颈背部肌肉。有研究表明,虽然在关闭切口时对分离的肌肉进行缝合重建,但18%的患者术后存在颈半棘肌重建不良,导致颈半棘肌及颈背部肌肉萎缩及功能不全;剥离肌肉C7止点及项韧带导致轴性疼痛及颈椎SVA改变[8]。为减少术后并发症的发生,有学者提出选择性椎板成形术,在保证减压效果的前提下减少开门节段,减少对颈椎后部肌肉、韧带的损伤,尤其是对C2及C7棘突肌肉、韧带的保护,取得良好疗效[9]。本研究回顾性分析2010年9月—2015年12月采用选择性椎板成形术和传统椎板成形术治疗的CSM患者的临床资料,并对临床效果进行对比分析,现总结报告如下。
1 资料与方法 1.1 一般资料纳入标准:①非手术治疗 > 3个月无效;②CT或MRI检查确认≥2个节段颈椎椎管狭窄、脊髓受压且有相应症状;③术前颈椎动力位X线片未发现颈椎明显不稳。排除标准:①术前侧位X线片示颈椎后凸畸形(C2~7 Cobb角≤-12°);②前方巨大椎间盘突出或骨赘致脊髓严重受压(椎管占位率≥50%);③类风湿关节炎、肿瘤、外伤、感染、脊柱手术史、伴胸腰段脊柱疾病;④失访或影像学资料不全。
根据以上标准共纳入患者130例,其中67例采用选择性后路颈椎椎板成形术治疗(试验组),63例采用传统后路颈椎椎板成形术治疗(对照组)。试验组中20例为后纵韧带骨化所致;对照组中17例为后纵韧带骨化所致。2组一般资料差异无统计学意义,具有可比性(P > 0.05,表 1)。
|
|
表 1 一般资料 Tab. 1 General data |
对照组患者全身麻醉后取俯卧位,常规消毒铺巾,做颈后正中切口长约10 cm,依次显露C3至C7棘突分叉,于棘突分叉基底部剪断分叉,剥离双侧椎旁肌显露C3~7棘突及椎板。用直径为2 mm的高速磨钻正中劈开C3~7棘突,之后改用直径为5 mm的磨钻于C3~7两侧椎板侧块交界处开槽至内板,用棘突间撑开器向两侧撑开,行双侧开门并在被劈开的棘突上打孔。取合适型号(24或26号)的梯形珊瑚羟基磷灰石人工骨(意华健,北京),用双10号丝线穿过人工骨及棘突打孔处后,将人工骨交叉固定于棘突上。将被劈开的棘突分叉缝合固定后逐层关闭切口。
试验组手术方法以C3~7病变,行C3~6开门为例(图 1)进行介绍。患者全身麻醉后取俯卧位,常规消毒铺巾,做颈后正中切口长约5 cm,剥离双侧椎旁肌显露C3~6棘突及椎板(注意不要剥离颈椎半棘肌及项韧带在C2及C7棘突上起止点)。其他步骤同对照组。椎板成形范围选择:①病变节段头端为C2,行C2椎板潜行减压并C3至尾端下位椎板(C6以上节段)开门。如病变节段为C2~5,行C2潜行减压并C3~5开门;②病变节段头端为C3,行C3至尾端下位椎板(C6以上节段)开门;③病变节段为C7,则开门至C6并C7椎板潜行减压。

|
a:显露C3~6棘突、椎板 b:双侧开槽、劈开棘突 c:双侧开门,箭头示劈开的棘突 d:安放羟基磷灰石人工骨并用丝线固定 e:切口长度 a:Exposing C3-6 spinous processes and laminae b:Bilateral grooving and splitting of spinous processes c:Double door. Arrow indicates splitting of spinous processes d:Hydroxyapatite artificial bone is placed and fixed with silk thread e:Length of incision 图 1 选择性椎板成形术切口 Fig. 1 Selective laminoplasty incision |
记录并比较2组手术时间、术中出血量、并发症发生情况,以及术前、末次随访时双手10 s握拳次数、双手握力及日本骨科学会(JOA)[10]评分。颈后或肩胛上区域疼痛或僵硬诊断为轴性症状。JOA评分改善率(%)=(术后JOA评分-术前JOA评分)/(17-术前JOA评分)×100%。
采用Surgimap Spine(Nemaris Inc,USA)软件,在术前及末次随访侧位X线片上测量并比较2组C2~7 Cobb角、C2~5 Cobb角、C5~7 Cobb角、C7倾斜角、T1倾斜角、C2~7 SVA和K线角。①Cobb角为相应节段上位椎体上终板与下位椎体下终板延长线间的夹角。②SVA为C2中心垂线与C7椎体后上缘的距离。③C7或T1倾斜角是C7或T1上终板延长线和水平线间的夹角。④K线为C2与C7椎管中点的连线,骨化的后纵韧带未超过K线为(+),超过K线为(-)。K线角为K线与铅垂线间的夹角。
1.4 统计学处理采用SPSS 22.0软件对数据进行统计学分析,数据采用x±s表示,术前及末次随访比较采用配对样本t检验,2组之间比较采用独立样本t检验;以P < 0.05为差异有统计意义。
2 结果试验组19例潜行切除C2椎板下缘,2例潜行切除C6椎板上缘,35例潜行切除C7椎板上缘。试验组手术时间、术中出血量均少于对照组,差异有统计学意义(P < 0.05,表 2)。2组患者末次随访时双手10 s握拳次数、双手握力及JOA评分均较术前改善,差异有统计学意义(P < 0.05,表 2);组间比较差异均无统计学意义(P > 0.05,表 2)。2组患者末次随访时C2~5 Cobb角、C5~7 Cobb角、C7倾斜角、T1倾斜角及K线角与术前相比差异均无统计学意义(P > 0.05,表 2);组间比较差异也无统计学意义(P > 0.05,表 2)。末次随访时,对照组C2~7 Cobb角较术前减小,C2~7 SVA较术前增大,差异均有统计学意义(P < 0.05,表 2);末次随访时,试验组C2~7 Cobb角和C2~7 SVA与术前相比差异均无统计学意义(P > 0.05,表 2);末次随访时,试验组C2~7 Cobb角和C2~7 SVA与对照组相比,差异均有统计学意义(P < 0.05,表 2)。
|
|
表 2 统计数据 Tab. 2 Statistical data |
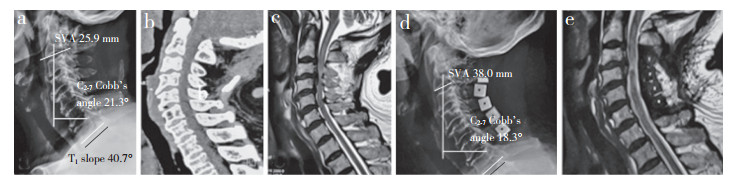
试验组术后1例因切口愈合不良行清创术,术后伤口愈合良好。对照组2例发生C5神经根麻痹,给予营养神经药物治疗后1个月好转;发生脑脊液漏1例,伤口感染2例,均经换药、清创等治疗后痊愈。末次随访时,试验组7例(7/67,10.4%)发生轴性症状,对照组20例(20/63,31.7%)发生轴性症状,试验组轴性症状发生率显著低于对照组,差异有统计学意义(P < 0.05)。2组典型病例影像学资料见图 2,3。
|
女,71岁,四肢麻木 > 4个月,行C3~6椎板成形术 a ~ c:术前影像学资料 d,e:术后2年影像学资料示减压充分,颈椎矢状位序列良好 Female, 71 years old, limbs numb for > 4 months, treated with C3-6 laminoplasty a-c:Preoperative imaging data d, e:Imaging data at postoperative 2 years show that decompression is sufficient and sagittal sequence of cervical spine is good 图 2 对照组典型病例影像学资料 Fig. 2 Imaging data of a typical case in control group |

|
男,47岁,右上肢无力 > 2年,加重0.5年,行C3~5椎板成形术,C2,6椎板潜行减压 a ~ c:术前影像学资料 d,e:术后3年影像学资料示减压充分,颈椎矢状位序列良好 Male, 47 years old, right upper limb weakness for > 2 years, aggravated by 0.5 years, treated with C3-5 laminoplasty and C2, 6 lamina decompression a-c:Preoperative imaging data d, e:Imaging data at postoperative 3 years show that decompression is sufficient and sagittal sequence of cervical spine is good 图 3 试验组典型病例影像学资料 Fig. 3 Imaging data of a typical case in experiment group |
颈椎生理曲度丢失或后凸畸形是椎板成形术后的主要并发症,颈椎生理曲度丢失使脊髓向后方漂移受限,间接导致减压效果下降,脊髓还会重新遭受前方致压物压迫,使已恢复的神经功能重新恶化[11]。Maeda等[12]认为术后颈椎曲度的维持不是通过椎间软组织挛缩或骨性融合来实现的,而是通过动力性因素(如肌肉和韧带的功能)来实现的。Sakaura等[13]在椎板成形术中保留C6,7项韧带,术后发生后凸畸形的患者明显减少,说明保留C6,7项韧带对整个颈椎序列的维持至关重要。本研究中对照组术后C2~5 Cobb角、C5~7 Cobb角与术前相比差异无统计学意义,但术后下颈椎曲度C2~7 Cobb角较术前减小,差异有统计学意义,说明椎板成形术后颈椎曲度的丢失是整个下颈椎曲度的丢失;试验组对颈椎后部整体肌肉、韧带的剥离少、破坏小,很好地维持了颈椎序列的生理曲度。本研究还发现对照组术后C2~7 SVA较术前增加,而试验组无明显改变,分析其原因可能为传统椎板成形术对颈椎后部肌肉韧带等组织破坏相对较重,导致颈椎后部伸肌力量减弱,头部中心前移,SVA增加。
Fujiyoshi等[14]认为对于前方致压物超过K线的患者,后路减压后脊髓不能获得足够的漂移程度,不能获得足够的神经功能恢复。因此,术前制订手术计划时要综合测量考虑各矢状位参数,进行合理全面的影像学评估。本研究中3例患者(试验组1例、对照组2例)术前骨化的后纵韧带均超过K线,术后神经功能均恢复良好。Kim等[15]研究发现K线角与C2~7 SVA强烈相关,是颈椎重要的矢状位参数,可为制订手术计划及术后评价临床疗效提供依据。本研究中2组患者术后K线角有增大趋势,但差异无统计学意义,将来仍需积累大样本数据,对K线角术后变化及其对临床疗效的影响作进一步研究。
3.1.2 轴性症状轴性症状是颈椎后路椎板成形术后最常见的并发症[16],严重影响患者生活质量。其发生的具体机制仍不清楚,有研究表明其与颈椎后部肌肉韧带的破坏,特别是C2与C7棘突肌肉止点、韧带的剥离有关[4, 8, 17]。颈半棘肌作为颈部动力稳定系统[18-19],大部分止于C2棘突,在颈部伸展中起重要作用。传统椎板成形术通常切开、分离颈半棘肌在C2棘突上的附着,即使在关闭切口时进行缝合重建,仍有患者术后颈半棘肌重建不良,导致颈半棘肌及颈背部肌肉萎缩及功能不全,引起轴性症状[8]。Fielding等[17]的研究表明,项韧带与C7棘突剥离可能会影响背部肌肉的收缩。颈部项韧带正常状态下一直保持紧张状态,支持背部肌肉系统,协助保持头部向前注视位置,且项韧带本身存在本体感受器,能够控制头部位置;因此,减少对项韧带的剥离,保持项韧带的紧张状态及C7棘突的完整性可减少轴性症状的发生。Takeuchi等[4]也证实,保留C7棘突及项韧带可以降低椎板成形术后轴性症状发生率。本研究中试验组不剥离颈半棘肌在C2棘突上的附着及在C7棘突上的止点,不剥离止于C7棘突上的肌肉和项韧带,C7棘突完整保留,颈部轴性症状发生率低于对照组。
3.1.3 C5神经根麻痹研究报道,椎板成形术后C5神经根麻痹发生率为5% ~ 8%[20],其具体发生机制尚未明确,普遍认为与脊髓过度后移导致的神经根牵拉作用有关。本研究中对照组2例发生C5神经根麻痹,试验组减少开门节段,在保证减压效果的前提下一定程度上减少了脊髓的后移,未发生C5神经根麻痹。
3.1.4 发生“再关门”单开门椎板成形术后易出现“再关门”现象,有研究表明其发生率为10%[21],可造成已扩大椎管的再狭窄,产生粘连及脊髓压迫。锚钉及微型钛板等内固定技术的应用,大大降低了“再关门”的发生率,但一定程度上加重了患者的经济负担[22]。本研究2组患者术中均采用羟基磷灰石人工骨,其为多孔海绵状结构,有利于骨长入,生物相容性好,强度大,无机体免疫排斥反应,其弧形结构适配脊髓圆柱状结构,极大减少了粘连及内置物引起的压迫;与自体髂骨相比,羟基磷灰石人工骨形态规则,不会引起供骨区疼痛及相关并发症,减少手术时间及出血量。本研究2组患者随访中均未出现“再关门”现象或人工骨移位、脱落。
3.2 选择性椎板成形术的优势本研究结果显示,2组在JOA评分改善率、双手握力、10 s握拳次数试验等神经功能评价上没有差异,选择性椎板成形术后复查CT或MRI显示减压充分。选择性椎板成形术的优势:①在保证减压效果(减压≥3个节段)的前提下,减少开门节段,减少对肌肉、韧带的剥离,保留C2和C7棘突及其附着的肌肉、韧带组织,减少创伤,缩短手术时间,减少出血量。②有利于维持颈椎生理曲度和C2~7 SVA,防止后凸畸形。③降低轴性症状发生率。
综上所述,2种术式治疗CSM中期临床疗效满意。选择性椎板成形术在保证减压效果的前提下,减少开门节段,减少对颈椎后部肌肉韧带的破坏,保护C2和C7棘突及其附着的肌肉、韧带,术后神经功能恢复满意,颈椎矢状位序列维持良好,手术时间短、出血量少,显著降低术后轴性症状的发生率,疗效满意,但仍需进行远期随访。
| [1] |
Seichi A, Takeshita K, Ohishi I, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy[J]. Spine (Phila Pa 1976), 2001, 26(5): 479-487. DOI:10.1097/00007632-200103010-00010 |
| [2] |
Aita I, Hayashi K, Wadano Y, et al. Posterior movement and enlargement of the spinal cord after cervical laminoplasty[J]. J Bone Joint Surg Br, 1998, 80(1): 33-37. |
| [3] |
Sodeyama T, Goto S, Mochizuki M, et al. Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord[J]. Spine(Phila Pa 1976), 1999, 24(15): 1527-1531. DOI:10.1097/00007632-199908010-00005 |
| [4] |
Takeuchi T, Shono Y. Importance of preserving the C7 spinous process and attached nuchal ligament in Frenchdoor laminoplasty to reduce postoperative axial symptoms[J]. Eur Spine J, 2007, 16(9): 1417-1422. DOI:10.1007/s00586-007-0352-8 |
| [5] |
Kato M, Nakamura H, Konishi S, et al. Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty[J]. Spine(Phila Pa 1976), 2008, 33(14): E455-E459. DOI:10.1097/BRS.0b013e318178e607 |
| [6] |
Yoon S, Kim KH, Park JY, et al. Risk factors for cervical sagittal malalignment after cervical laminoplasty[J]. Nerve, 2017, 3(2): 38-43. DOI:10.21129/nerve.2017.3.2.38 |
| [7] |
Suk KS, Kim KT, Lee JH, et al. Sagittal alignment of the cervical spine after the laminoplasty[J]. Spine (Phila Pa 1976), 2007, 32(23): E656-E660. DOI:10.1097/BRS.0b013e318158c573 |
| [8] |
Iizuka H, Shimizu T, Tateno K, et al. Extensor musculature of the cervical spine after laminoplasty:morphologic evaluation by coronal view of the magnetic resonance image[J]. Spine (Phila Pa 1976), 2001, 26(20): 2220-2226. DOI:10.1097/00007632-200110150-00013 |
| [9] |
Tsuji T, Asazuma T, Masuoka K, et al. Retrospective cohort study between selective and standard C3-7 laminoplasty. Minimum 2-year follow-up study[J]. Eur Spine J, 2007, 16(12): 2072-2077. DOI:10.1007/s00586-007-0428-5 |
| [10] |
Fukui M, Chiba K, Kawakami M, et al. Japanese Orthopaedic Association cervical myelopathy evaluation questionnaire(JOACMEQ):Part 2. Endorsement of the alternative item[J]. J Orthop Sci, 2007, 12(3): 241-248. DOI:10.1007/s00776-007-1119-0 |
| [11] |
Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery[J]. Neurosurgery, 2012, 71(3): 662-669. DOI:10.1227/NEU.0b013e31826100c9 |
| [12] |
Maeda T, Arizono T, Saito T, et al. Cervical alignment, range of motion, and instability after cervical laminoplasty[J]. Clin Orthop Relat Res, 2002(401): 132-138. |
| [13] |
Sakaura H, Hosono N, Mukai Y, et al. Preservation of the nuchal ligament plays an important role in preventing unfavorable radiologic changes after laminoplasty[J]. J Spinal Disord Tech, 2008, 21(5): 338-343. DOI:10.1097/BSD.0b013e3181453de4 |
| [14] |
Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament:the K-line[J]. Spine(Phila Pa 1976), 2008, 33(26): E990-E993. DOI:10.1097/BRS.0b013e318188b300 |
| [15] |
Kim HS, Kim TH, Park MS, et al. K-line tilt as a novel radiographic parameter in cervical sagittal alignment[J]. Eur Spine J, 2018, 27(8): 2023-2028. DOI:10.1007/s00586-018-5634-9 |
| [16] |
Moon MS. Neck and shoulder pain after laminoplasty[J]. Spine (Phila Pa 1976), 1997, 22(14): 1674-1676. DOI:10.1097/00007632-199707150-00030 |
| [17] |
Fielding JW, Burstein AH, Frankel VH. The nuchal ligament[J]. Spine (Phila Pa 1976), 1976, 1(1): 3-14. DOI:10.1097/00007632-197603000-00002 |
| [18] |
Nolan JP Jr, Sherk HH. Biomechanical evaluation of the extensor musculature of the cervical spine[J]. Spine (Phila Pa 1976), 1988, 13(1): 9-11. DOI:10.1097/00007632-198801000-00003 |
| [19] |
Sherk HH. Stability of the lower cervical spine[M]//Kehr P, Weidne A. Cervical Spine I. Vienna: Springer, 1987: 59-64.
|
| [20] |
Chiba K, Toyama Y, Matsumoto M, et al. Segmental motor paralysis after expansive open-door laminoplasty[J]. Spine (Phila Pa 1976), 2002, 27(19): 2108-2115. DOI:10.1097/00007632-200210010-00006 |
| [21] |
Wang HQ, Mak KC, Samartzis D, et al. "Spring-back" closure associated with open-door cervical laminoplasty[J]. Spine J, 2011, 11(9): 832-838. DOI:10.1016/j.spinee.2011.07.026 |
| [22] |
Freedman B, Heller J, Rhee J. Cervical laminoplasty myths and realities:a meta-analysis of outcomes and complications[J]. Spine J, 2009, 9(Suppl 1): 23. |
 2019, Vol.17
2019, Vol.17  Issue(5): 308-313
Issue(5): 308-313


