胸腰椎骨折是骨科常见病、多发病,目前常见的治疗方法是后路开放椎弓根螺钉内固定术,但该术式术中需广泛切开组织,创伤大、出血量多,晚期残留腰背部僵硬、疼痛等并发症[1]。针对开放手术的弊端,本研究组自2014年1月开始采用改良金属网格定位器经皮微创椎弓根螺钉内固定术治疗单椎体无神经症状的胸腰椎骨折。本研究回顾性分析2014年1月—2017年12月收治的50例单椎体胸腰椎骨折患者临床资料,分别采用改良金属网格定位器经皮微创和传统后路开放椎弓根螺钉内固定术治疗并比较其疗效,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄20 ~ 60岁;②单椎体骨折;③椎管受累≤1/3,椎体前缘高度丢失≥1/3;④无脊髓或神经损伤。排除标准:①病理性骨折;②严重骨质疏松;③合并其他基础疾病或不能耐受手术。根据上述标准共纳入无神经症状的单椎体胸腰椎骨折患者50例,其中25例采用改良金属网格定位器经皮微创椎弓根螺钉内固定术治疗(微创组),25例采用传统后路开放椎弓根螺钉内固定术治疗(开放组)。2组患者术前一般资料差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 一般资料 Tab. 1 General data |
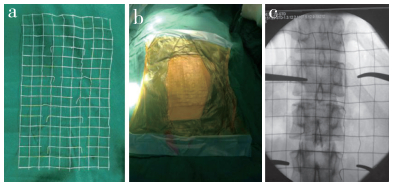
微创组患者气管插管全身麻醉后俯卧于双横软垫上,过伸体位复位椎体骨折。C形臂X线机透视定位伤椎,手术区域常规消毒铺巾,以伤椎为中心放置改良金属网格定位器(图 1),通过金属网格定位伤椎上下椎体的椎弓根影,C形臂X线机透视下将4根导针经伤椎上下邻近椎体椎弓根穿刺入椎体内。以导针为中心,做4个长约2 cm小切口,依次切开皮肤、皮下组织及腰背筋膜,沿导针用扩张器钝性分离肌纤维后置入工作套筒,沿导针攻丝后在伤椎上下邻近椎体拧入合适长度及直径的椎弓根螺钉;持棒器夹持合适长度的连接棒,通过上位螺钉处切口,将连接棒置入椎弓根螺钉U形槽中,先拧紧连接棒一端的尾帽,复位器撑开复位后再拧紧另一端尾帽。C形臂X线机透视证实骨折椎体复位满意,内固定在位,清点纱布、器械后缝合切口。
|
a:改良金属网格定位器网格大小约1 cm×1 cm,可局部剪断或弯折利于术中定位 b:术中将金属网格定位器用3M贴膜固定于皮肤,防止移位 c:术中1次透视即可定位伤椎椎弓根 a:Mesh size of modified metal grid locator is about 1 cm×1 cm, which can be cut or bent to facilitate intraoperative localization b:Metal grid locator is fixed on skin with 3M adhesive tape during operation to prevent displacement c:One fluoroscopy during operation can locate injured vertebral pedicle 图 1 改良金属网格定位器 Fig. 1 Modified metal grid locator |
开放组患者气管插管全身麻醉后俯卧于双横软垫上,过伸体位复位椎体骨折,C形臂X线机透视定位伤椎,手术区域常规消毒铺巾。以伤椎为中心做1个长约12 cm后正中切口,依次切开皮肤、皮下组织及腰背筋膜,分离椎旁肌在棘突上的附着处,剥离椎旁肌,直视下置入合适长度及直径的椎弓根螺钉,选取合适长度的连接棒,预弯后安装连接棒,撑开复位后拧紧尾帽,透视确定椎弓根螺钉位置及椎体复位满意后,伤口冲洗、彻底止血,留置负压引流管1根,缝合切口。
1.3 围手术期处理术前30 min预防性应用抗生素,术后24 h停用。微创组不放置引流管;开放组常规放置引流管,术后48 h内拔除。术后3 d指导患者床上轴线翻身,并进行肌肉主动舒缩训练及被动伸屈踝、膝、髋关节功能训练,术后3 d佩戴腰围下床活动。
1.4 观察指标记录2组切口总长度、手术时间、术中出血量、置钉准确率及并发症发生情况。术前、术后1周、末次随访时均行X线、CT检查,必要时行MRI检查,测量2组伤椎前缘高度及Cobb角。伤椎前缘相对高度(%)=(伤椎前缘高度×2)/(伤椎上位椎体前缘高度+伤椎下位椎体前缘高度)×100%;Cobb角为伤椎上位椎体上终板线垂线和伤椎下位椎体下终板线垂线间的夹角。末次随访时采用改良MacNab疗效评定标准[3]评价腰背部功能恢复情况。采用Mobbs-Raley简易分级标准[4]评价置钉准确率:0级,螺钉位于椎弓根皮质内;1级,螺钉突破椎弓根骨壁≤2 mm;2级,螺钉突破椎弓根骨壁 > 2 mm,但无神经根受压症状;3级,出现椎弓根骨折、突破椎体前壁压迫血管/神经、突破椎弓根内/外壁出现神经并发症;0级和1级为置钉准确螺钉。
1.5 统计学处理采用SPSS 19.0软件对数据进行统计学分析,计量资料以x±s表示,组间比较采用t检验,计数资料比较采用χ2检验;以P < 0.05为差异有统计学意义。
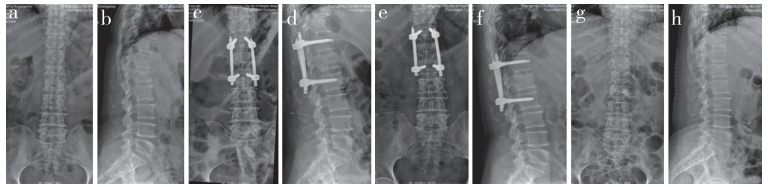
2 结果所有手术顺利完成,随访12 ~ 21(16.1±2.4)个月。微创组切口总长度、手术时间、术中出血量明显优于开放组,差异均有统计学意义(P < 0.05,表 2)。微创组置钉准确率为95%(95/100);开放组置钉准确率为94%(94/100);组间差异无统计学意义(P > 0.05,表 2)。2组患者术后1周、末次随访时伤椎前缘相对高度及Cobb角均较术前明显改善,差异有统计学意义(P < 0.05,表 2);组间比较差异无统计学意义(P > 0.05,表 2)。末次随访时改良MacNab疗效评定:微创组优15例,良8例,可2例,优良率为92%;开放组优13例,良9例,可3例,优良率为88%;组间差异无统计学意义(P > 0.05)。微创组患者均未放置引流管,开放组术后常规放置引流管,术后引流量(246.8±141.5)mL。微创组1例麻醉苏醒后侧卧位1 h后腰背部出现1个4 cm×5 cm×5 cm大小的皮下血肿,嘱患者仰卧位后皮下血肿未进一步增大,对症治疗后血肿自行吸收;其余患者术后采取仰卧位6 h后再翻身,未发生类似并发症。2组患者无其他相关并发症发生。2组典型病例影像学资料见图 2,3。
|
|
表 2 统计数据 Tab. 2 Statistical data |

|
男,38岁,T12压缩性骨折 a,b:术前正侧位X线片示T12压缩性骨折,椎体前缘压缩30% c,d:术后1周正侧位X线片示T12前缘高度恢复满意 e,f:术后1年正侧位X线片示骨折愈合,内固定在位 g,h:内固定取出后1周正侧位X线片示椎体前缘高度未见丢失 Male, 38 years old, T12 compression fracture a, b:Preoperative anteroposterior and lateral roentgenographs show T12 compression fractures, anterior vertebral height of injured vertebra is compressed by 30% c, d:Anteroposterior and lateral roentgenographs at postoperative 1 week show satisfactory recovery of T12 anterior vertebral height e, f:Anteroposterior and lateral roentgenographs at postoperative 1 year show fracture healing and good position of internal fixation g, h:Anteroposterior and lateral roentgenographs at 1 week after removal of internal fixation show no loss of anterior vertebral height 图 2 微创组典型病例影像学资料 Fig. 2 Imaging data of a typical case in minimally invasive group |
|
女,60岁,L1压缩性骨折 a,b:术前正侧位X线片示L1压缩性骨折,椎体前缘压缩30% c,d:术后1周正侧位X线片示L1前缘高度恢复满意 e,f:术后1年正侧位X线片示骨折愈合,内固定在位 g,h:内固定取出后1周正侧位X线片示椎体前缘高度未见丢失 Female, 60 years old, L1 compression fracture a, b:Preoperative anteroposterior and lateral roentgenographs show L1 compression fractures, anterior vertebral height of injured vertebra is compressed by 30% c, d:Anteroposterior and lateral roentgenographs at postoperative 1 week show satisfactory recovery of L1 anterior vertebral height e, f:Anteroposterior and lateral roentgenographs at postoperative 1 year show fracture healing and good position of internal fixation g, h:Anteroposterior and lateral roentgenographs at 1 week after removal of internal fixation show no loss of anterior vertebral height 图 3 开放组典型病例影像学资料 Fig. 3 Imaging data of a typical case in open group |
针对无神经症状的单椎体胸腰椎骨折,微创与开放手术临床疗效无明显差异[5-6],但微创手术具有组织损伤小、术中出血量少、术后恢复快等优点。微创手术成功的关键在于螺钉是否能准确经椎弓根到达椎体,而置钉成功与否取决于定位穿刺是否准确。张海平等[7]的研究表明,经皮微创内固定术治疗胸腰椎骨折最常见的并发症为螺钉位置不良,多与置钉路径欠佳有关。传统经皮微创椎弓根穿刺定位的方法包括髂嵴定位法、伤椎形态定位法、克氏针定位法、皮肤标记物定位法、穿刺针头定位法和金属网格定位法等,其定位准确率分别为52%、74%、83%、69%、82%和99%,金属网格定位法穿刺准确率最高[8]。但常规的金属网格为纵横交错的不锈钢丝组成的小方格,术中透视时需加用其他金属标志物,针对该弊端本研究组对其进行了改良,通过对局部金属丝剪断或折弯,极大提高了术中定位准确性和椎弓根穿刺的精确度。易国良等[8]的研究表明,常规网格在经皮微创椎弓根穿刺定位中平均定位时间为2 min,平均透视次数为2次,而本研究采用改良金属网格定位器定位伤椎椎弓根时均1次透视即穿刺成功,较常规金属网格具有优势。
3.2 微创和传统后路开放椎弓根螺钉内固定术治疗胸腰椎骨折的比较胸腰段骨折在临床上较为常见,经典的手术方法为后路椎弓根螺钉内固定术,被脊柱外科医师广泛接受,并取得了较好的治疗效果。但后路开放手术需对伤椎节段的椎旁肌及多裂肌广泛剥离,破坏脊柱稳定性,术后易出现腰痛、僵硬及功能受限等并发症。研究表明,患者术后出现腰痛、僵硬及功能受限可能与开放手术剥离至多裂肌止点,造成术后局部肌肉纤维瘢痕化、肌纤维水肿、功能下降及失神经支配有关,这些改变影响术后腰背部活动,从而造成患者术后慢性腰痛[9-11]。针对开放手术的缺陷,如何在保证临床疗效的同时,尽可能减少术后并发症、提高患者满意度是脊柱外科医师努力的方向。
目前临床上针对经皮微创和传统后路开放手术治疗单节段无神经症状胸腰椎骨折的研究较多,多数学者认为,经皮微创手术具有软组织损伤小、术中出血量少、术后疼痛评分低[12-15]、组织炎性反应小[16-17]等优点,且在影像学指标上与传统后路开放手术疗效相当[5-6]。但也有学者指出,微创手术后隐性出血量要高于开放手术,这点需引起临床医师的高度重视[18]。与开放手术相比,微创手术术中需反复透视,微创组术中透视时间比开放组长约13 min[12, 18]。本研究微创组采用自制的改良金属网格定位器,均1次透视即定位成功,且1次透视即可定位术中需要置钉的全部椎弓根,减少术中透视次数,缩短手术时间,降低医患辐射暴露。而且,改良金属网格定位器制作简单,经济投入小,值得临床推广应用。
3.3 注意事项及手术技巧改良金属网格定位器经皮微创椎弓根螺钉内固定术治疗无神经症状的胸腰椎骨折在临床应用时需注意以下方面。①患者入院后平卧位时在伤椎处垫软枕,手术室麻醉后采用腹部悬空俯卧体位复位伤椎,必要时可调节手术床使患者腰背部过伸,使伤椎前缘高度得到最大程度恢复。②通过体表标志大致定位伤椎后,在伤椎处放置改良金属网格定位器,并用3M贴膜固定于术区皮肤,金属网格可局部剪断或弯折,用血管钳夹辅助定位。在导针置入后取下改良金属网格定位器,否则会影响下一步经皮通道的建立及椎弓根螺钉置入。③术前影像学检查预先测量伤椎椎弓根确定螺钉直径及长度,利于术中快速选择合适直径及长度的椎弓根螺钉。④椎弓根螺钉置入后,体外的U形槽内预置金属连接棒,通过调整使同侧上下2个椎弓根螺钉U形槽方向一致,皮下置棒多可一次成功。上位椎弓根螺钉置棒后,可在下位椎弓根螺钉U形槽内垂直放置吸引器,通过按压持棒器观察吸引器是否有“跷跷板样”弹跳动作来确保连接棒位于下位椎弓根螺钉U形槽内。⑤固定连接棒时,先拧紧一端的椎弓根螺钉尾帽,通过体外撑开器再次撑开复位后再拧紧另一端的椎弓根螺钉尾帽,可确保伤椎前缘高度得到有效恢复。⑥严格把握微创手术的适应证与禁忌证。
综上所述,对于无神经症状的单椎体胸腰椎骨折,采用改良金属网格定位器经皮微创与传统后路开放椎弓根螺钉内固定术疗效相当,但微创手术具有创伤小、手术时间短、术后恢复快等优点,改良金属网格术中定位准确率高,值得临床推广应用。本研究的局限性:在手术方式选择上,2组均为跨伤椎固定,而未选择经伤椎固定;在透视次数及透视时间方面未与传统金属网格比较,需要在以后的研究中逐步完善。
| [1] |
王洪伟, 李长青, 周跃, 等. 附加伤椎固定的微创经皮椎弓根螺钉(Sextant)治疗胸腰椎骨折[J]. 中华创伤骨科杂志, 2010, 12(2): 18-22. |
| [2] |
Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive of classification of thoracic and lumbar injuries[J]. Eur Spine J, 1994, 3(4): 184-201. DOI:10.1007/BF02221591 |
| [3] |
MacNab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients[J]. J Bone Joint Surg Am, 1971, 53(5): 891-903. DOI:10.2106/00004623-197153050-00004 |
| [4] |
Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine:accuracy and complication rates[J]. Spine(Phila Pa l976), 2012, 37(12): 1902-1100. |
| [5] |
Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures:systematic review and meta-analysis of comparative studies[J]. Clin Neurol Neurosurg, 2015, 135: 85-92. DOI:10.1016/j.clineuro.2015.05.016 |
| [6] |
张锦洪, 殷国勇, 曹晓建, 等. 开放手术与微创手术治疗胸腰椎骨折的疗效对比[J]. 脊柱外科杂志, 2015, 13(6): 364-368. |
| [7] |
张海平, 郝定均, 贺宝荣, 等. 经皮微创复位内固定术治疗胸腰椎骨折的并发症[J]. 脊柱外科杂志, 2018, 16(6): 344-348. |
| [8] |
易国良, 宋西正, 王文军, 等. 网格定位板在经皮椎弓根微创手术进钉点定位中的应用[J]. 中国组织工程研究, 2017, 21(15): 2366-2371. DOI:10.3969/j.issn.2095-4344.2017.15.013 |
| [9] |
Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture[J]. Asian Spine J, 2015, 9(1): 133-146. DOI:10.4184/asj.2015.9.1.133 |
| [10] |
Nakasuji M, Suh SH, Nomura M, et al. Hypotension from spinal anesthesia in patients aged greater than 80 years is due to a decrease in systemic vascular resistance[J]. J Clin Anesth, 2012, 24(3): 201-206. DOI:10.1016/j.jclinane.2011.07.014 |
| [11] |
Jindal N, Sankhala SS, Bachhal V. The role of fusion in the management of burst fractures of the thoracolumbar spine treated by short segment pedicle screw fixation:a prospective randomised trial[J]. J Bone Joint Surg Br, 2012, 94(8): 1101-1106. |
| [12] |
程彬, 史柏娜, 赵敏, 等. 自制引导通道经皮置入椎弓根螺钉与开放后路短节段内固定治疗胸腰椎骨折的疗效比较[J]. 临床骨科杂志, 2018, 21(3): 266-269. DOI:10.3969/j.issn.1008-0287.2018.03.004 |
| [13] |
史航, 朱裕成, 马军, 等. 两种不用术式治疗胸腰椎骨折的对比研究[J]. 实用骨科杂志, 2016, 22(9): 819-822. |
| [14] |
文天林, 孟浩, 王飞, 等. 经皮与开放椎弓根螺钉内固定术治疗无神经损伤胸腰椎骨折的疗效对比[J]. 中国脊柱脊髓杂志, 2016, 26(5): 401-407. DOI:10.3969/j.issn.1004-406X.2016.05.04 |
| [15] |
夏太宝, 赵广超, 薛双桃, 等. 经皮与Wiltse入路椎弓根螺钉治疗单节段胸腰椎骨折的疗效比较[J]. 临床骨科杂志, 2018, 21(4): 415-418. DOI:10.3969/j.issn.1008-0287.2018.04.011 |
| [16] |
邹澍, 吕仁发, 刘加钱, 等. 经皮与开放椎弓根钉内固定术后创伤反应相关血清指标的比较研究[J]. 创伤外科杂志, 2018, 20(3): 221-224. |
| [17] |
梁波. 微创经皮椎弓根钉内固定术治疗单纯性下胸椎及腰椎骨折的疗效分析[J]. 创伤外科杂志, 2018, 20(9): 696-700. DOI:10.3969/j.issn.1009-4237.2018.09.015 |
| [18] |
张永远, 王希骥, 赵勤鹏, 等. 经皮与开放椎弓根钉复位内固定治疗无神经损伤胸腰椎骨折的比较研究[J]. 中华创伤骨科杂志, 2018, 20(4): 296-302. DOI:10.3760/cma.j.issn.1671-7600.2018.04.005 |
 2019, Vol.17
2019, Vol.17  Issue(6): 388-393
Issue(6): 388-393


