2. 海军军医大学附属长海医院骨科, 上海 200433;
3. 海军军医大学附属长征医院骨科, 上海 200003
2. Department of Orthopaedics, Changhai Hospital, Navy Medical University, Shanghai 200433, China;
3. Department of Orthopaedics, Changzheng Hospital, Navy Medical University, Shanghai 200003, China
腰椎椎间盘突出症(LDH)是临床上引起腰痛的常见原因,常伴随单/双侧下肢放射痛和/或麻木,是中老年人群的常见病、多发病。Wahren等[1]于1945年首次报道了青少年LDH,通常青少年的椎间盘处于生长发育阶段,不易发生LDH,该文献报道青少年LDH占全部LDH的0.4% ~ 6.0%。Zitting等[2]分析了12 058例0 ~ 28岁的样本人群,在0 ~ 15岁人群中未发现LDH患者;在 > 15且≤ 20岁人群中,LDH发生率为0.1% ~ 0.2%;在 > 20且≤ 28岁人群中,LDH发生率显著升高(男性9.5%,女性4.2%)。Wang等[3]提出LDH发生率逐年上升,且趋于年轻化,< 21岁人群LDH发生率呈增高趋势。大部分青少年LDH患者经规范的非手术治疗后症状会逐渐缓解直至消失,但仍有部分患者需手术治疗。经皮内窥镜下腰椎椎间盘切除术(PELD)和椎板开窗椎间盘切除术是治疗青少年LDH的常见术式,本研究对2012年1月—2016年12月海军军医大学附属长征医院收治的采用2种术式治疗的青少年LDH患者临床资料进行回顾性分析,探讨PELD在治疗青少年LDH中的应用价值,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄13 ~ 21岁;②CT、MRI检查明确诊断为单节段LDH,突出位置、程度和患者临床症状、体征相符;③持续或反复腰痛,采用规范非手术治疗 > 3个月症状不能缓解或进行性加重,需进行手术治疗;④患者对研究知情,愿意配合并签署知情同意书。排除标准:①合并严重肝肾功能不全等内科疾病;②凝血功能障碍;③病变部位有既往手术史;④合并严重腰椎椎管狭窄或腰椎滑脱;⑤患有精神疾病。术前详细告知患者及家属2种手术方案的优缺点、风险及术后并发症,患者及家属自主选择手术方案。根据以上标准,共纳入青少年LDH患者82例,其中40例(A组)采用PELD治疗,42例(B组)采用椎板开窗椎间盘切除术治疗。2组患者术前均常规进行腰椎正侧位X线、CT三维重建、MRI平扫等检查确定LDH类型和程度,根据影像学检查结果制定合理的治疗方案,所有手术均由同一手术组完成。2组患者术前一般资料差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 一般资料 Tab. 1 General data |
对于L4/L5节段突出和低髂棘的L5/S1节段突出患者,选用经椎间孔入路经皮内窥镜下椎间盘切除术(PETD)。患者俯卧于Jackson透视床上,C形臂X线机透视定位,根据正侧位透视的椎间隙水平的交点确定进针点,由于患者体型不同,一般取棘突正中线旁开8 ~ 14 cm,术前根据患者横断面CT资料计算穿刺针长度。采用2%利多卡因行局部浸润麻醉,C形臂X线机透视下穿刺,采用1:3的美蓝与泛影葡胺混合液进行椎间盘造影,穿刺针最终进针位置:正位X线片上位于椎弓根内侧线,侧位X线片上位于椎体后缘,此部位与安全三角相对应。以导针为中心扩张工作通路,直径约8 mm,经工作通道置入手术操作系统,以髓核钳取出蓝染的椎间盘病变组织,减压神经根并行纤维环成形。术毕探查神经根松解程度,缝合皮肤,无菌敷料包扎。
PETD处理范围有限,特别是对于髂嵴较高的L5/S1节段突出患者,由于高髂嵴的遮挡,穿刺针及内窥镜无法顺利到达椎间盘突出的部位,增加了手术难度。此类患者可选择经椎板间入路经皮内窥镜下椎间盘切除术(PEID)[4]。PEID可充分暴露病灶,术野清晰;探查范围广泛,可充分切除病灶、分离神经根,进行减压。
A组40例患者中23例采用PETD治疗,17例采用PEID治疗。
1.2.2 椎板开窗椎间盘切除术患者取俯卧位,全身麻醉,定位病变节段,沿后正中线做3 ~ 5 cm切口,逐层暴露至椎间盘突出侧关节突关节,神经拉钩保护硬膜和神经根,清除髓核和纤维环,彻底清理椎间隙、松解神经根,生理盐水冲洗术区,彻底止血后放置引流管,常规缝合切口,无菌敷料包扎。
1.3 术后处理2组患者术后常规使用二代头孢48 ~ 72 h预防感染,A组患者术后72 h佩戴腰围下床活动,1个月内以卧床休息为主,3个月内避免剧烈运动、弯腰等活动。B组术后72 h佩戴腰围下床活动,腰围佩戴时间均 > 2个月。
患者在术后3、6和12个月进行随访。之后2年内每6个月随访1次,或患者感到不适时进行随访。随访时行X线和/或MRI检查。
1.4 观察指标记录2组患者手术时间、术中出血量、术后卧床时间、咬骨体积,以及术前、术后1个月和末次随访时疼痛视觉模拟量表(VAS)评分[5]、Oswestry功能障碍指数(ODI)[6]。末次随访时采用改良MacNab疗效评定标准[7]对2组患者的临床疗效进行评估。
1.5 统计学处理采用SPSS 19.0软件对数据进行统计学分析,计量资料以x±s表示,组间一般资料及围手术期指标采用完全随机t检验;术前、术后1个月、末次随访时VAS评分、ODI比较采用单因素方差分析;计数资料采用χ2检验;以P < 0.05为差异有统计学意义。
2 结果所有手术顺利完成。所有患者随访 > 12个月,平均28个月。A组的手术时间、术中出血量、术后卧床时间及咬骨体积均低于B组,差异有统计学意义(P < 0.05,表 2)。2组患者术后VAS评分和ODI均较术前明显改善,差异有统计学意义(P < 0.05,表 2);组间比较术后VAS评分和ODI,差异均无统计学意义(P > 0.05,表 2)。
|
|
表 2 统计数据 Tab. 2 Statistical data |
末次随访时MacNab疗效评定,A组优28例、良9例、可3例,优良率为92.50%(37/40);B组优28例、良10例、可4例,优良率为90.48%(38/42);组间比较差异无统计学意义(P > 0.05)。
A组术后出现手术侧肢体一过性浅感觉减退2例,并发症发生率为5.0%(2/40);B组术后发生脑脊液漏1例,手术侧肢体一过性浅感觉减退1例,腰痛复发1例,并发症发生率为7.1%(3/42);组间比较差异无统计学意义(P > 0.05);末次随访时上述症状均已消失。
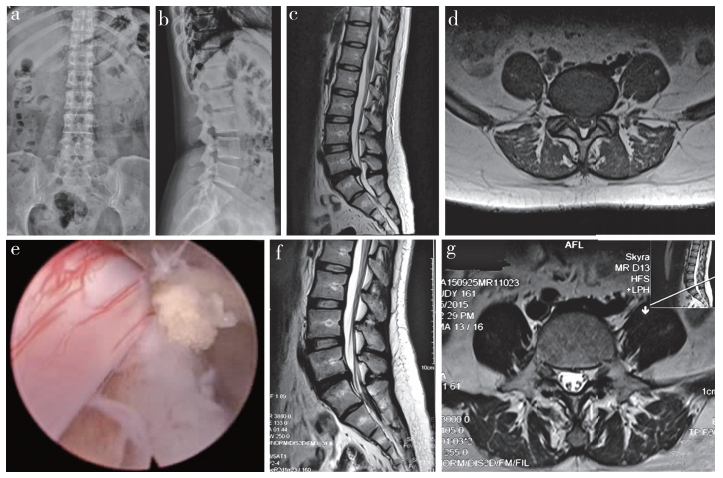
末次随访时,A组有2例复发,复发率为5.00%;B组有1例复发,复发率为2.38%;组间比较差异无统计学意义(P > 0.05)。A组1例复发病例为男性,体质量指数(BMI)为30.2,术后45个月打篮球后腰部疼痛不适伴左下肢放射痛,经非手术治疗后疼痛明显缓解,未再次行手术治疗。其余2例复发患者非手术治疗无效后行腰椎减压植骨融合内固定术,术后恢复尚可。典型病例影像学资料见图 1。
|
男,19岁,体质量89 kg,腰痛伴右下肢放射痛、麻木3个月,加重1周,采用PEID治疗 a:术前正位X线片示骨质结构完整,未骨折 b:术前侧位X线片示腰椎生理曲度变直,L5/S1椎间隙稍变窄 c:术前矢状面MRI示L5/S1椎间盘突出明显,硬膜囊受压严重 d:术前横断面MRI示椎间盘中央型突出,硬膜囊受压明显 e:术中取出突出髓核组织,彻底减压 f:术后28个月矢状面MRI示硬膜囊无受压 g:术后28个月横断面MRI示硬膜囊恢复,脑脊液分布均匀 Male, 19 years old, weighing 89 kg, with low back pain, right lower extremity radiation pain and numbness for 3 months and aggravated 1 week, treated with PEID a:Preoperative anteroposterior roentgenograph shows complete bone structure without fracture b:Preoperative lateral roentgenograph shows that lumbar physiological curvature become straight and L5/S1 intervertebral space slightly narrowed c:Preoperative sagittal MRI shows that L5/S1 intervertebral disc herniation is obvious, and dural sac is seriously compressed d:Preoperative transverse MRI shows central disc herniation and compression of dural sac e:Herniated nucleus pulposus tissue has been removed during operation and complete decompression f:Sagittal MRI at postoperative 28 months shows no compression of dural sac g:Transverse MRI at postoperative 28 months shows dural sac has been restored, and cerebrospinal fluid is evenly distributed 图 1 典型病例影像学资料 Fig. 1 Imaging data of a typical case |
20岁之后人体的椎间盘开始发生退行性变,30岁以后即有明显的退行性变表现,加之生活方式和工作方式的改变,久坐、肥胖、不良姿势等因素导致青少年LDH的发生率逐年增高[8-9]。区别于中老年LDH,青少年LDH有以下特点。①症状轻,体征重,患者腰痛及坐骨神经痛等主观感受轻,下肢感觉、运动和病理反射改变较为常见;②脊柱通常伴有先天畸形,如骶椎腰化、腰椎骶化等;③常有外伤史;④男性发生率高于女性[9-11]。
青少年LDH的危险因素主要有腰部外伤史、结构畸形、遗传因素、职业因素及心理因素等[12]。Lee等[9]认为外伤是青少年LDH的主要原因,本研究纳入的82例患者中有21例存在腰部外伤史。青少年的椎间盘结构存在一定缺陷,有研究发现青少年LDH患者的椎间盘纤维环相对薄弱,在外伤等因素作用下可出现纤维环破裂,进而导致LDH的发生;椎间盘纤维环血供缺乏、营养不足,外伤等外力作用造成纤维环破坏后无法及时修复,导致LDH的发生与进展[12-13]。
青少年LDH的治疗原则为首先非手术治疗,若无效再行手术治疗。传统椎板开窗椎间盘切除术可通过切除部分椎板、摘除突出的髓核组织达到减压目的,但其存在椎板及椎旁肌肉组织损伤大、影响椎体稳定性、增加术后组织粘连、术后患者恢复慢等缺点,对青少年术后生活质量产生较大影响;相比较而言,显微内窥镜下椎间盘切除术(MED)及PELD等微创术式具有创伤小、恢复快、对脊柱稳定性影响小等诸多优势,是治疗青少年LDH的首选[14]。PELD无需切除椎板,不破坏椎旁肌肉和韧带,保留脊柱完整性,避免神经根粘连;手术在局部麻醉下进行,通过术者与患者的术中沟通可预防神经根损伤,内窥镜下可清晰探查、准确摘除髓核,有效减压[15-17]。PETD及PEID为PELD的2种主要术式。对于L4/L5节段的病变推荐采用PETD治疗;对于L5/S1节段的病变PEID疗效更佳[4, 8, 18-20],如髂嵴明显高于L5/S1椎间隙,PEID可避免髂嵴阻挡,穿刺相对简单,术中透视时间短,减少射线暴露。
本研究结果显示,2组术后VAS评分和ODI均较术前明显下降,组间差异无统计学意义,说明2种术式均能有效缓解疼痛,改善功能,疗效相当,与既往报道结果一致[21]。A组手术时间、术中出血量、术后卧床时间均优于B组,说明PELD可减少手术创伤,有利于患者早期康复。A组咬骨体积明显小于B组,说明PELD对患者脊柱骨性结构的破坏更小,有利于维持脊柱稳定性。有研究证实PELD与其他手术方式相比,骨性结构损伤少,脊柱稳定性更高[22-23]。
综上所述,PELD可取得与传统椎板开窗椎间盘切除术相近的临床疗效,且可降低出血量,减少骨性结构破坏,缩短患者术后卧床及康复时间,是较为理想的治疗青少年LDH的微创方法。但本研究病例数较少,本研究结果还需大样本量的临床研究进一步证实。
| [1] |
Wahren H. Herniated nucleus pulposus in a child of twelve years[J]. Acta Orthop Scand, 1945, 16(1): 40-42. |
| [2] |
Zitting P, Rantakallio P, Vanharanta H. Cumulative incidence of lumbar disc diseases leading to hospitalization up to the age of 28 years[J]. Spine(Phila Pa 1976), 1998, 23(21): 2337-2343. DOI:10.1097/00007632-199811010-00017 |
| [3] |
Wang H, Cheng J, Xiao H, et al. Adolescent lumbar disc herniation:experience from a large minimally invasive treatment centre for lumbar degenerative disease in Chongqing, China[J]. Clin Neurol Neurosurg, 2013, 115(8): 1415-1419. DOI:10.1016/j.clineuro.2013.01.019 |
| [4] |
Papavero L, Kothe R. The translaminar approach for cranially extruded lumbar disc herniations[J]. Oper Orthop Traumatol, 2013, 25(1): 6-15. DOI:10.1007/s00064-012-0193-4 |
| [5] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [6] |
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271-273. |
| [7] |
MacNab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients[J]. J Bone Joint Surg Am, 1971, 53(5): 891-903. DOI:10.2106/00004623-197153050-00004 |
| [8] |
Ahn Y, Oh HK, Kim H, et al. Percutaneous endoscopic lumbar foraminotomy:an advanced surgical technique and clinical outcomes[J]. Neurosurgery, 2014, 75(2): 124-133. DOI:10.1227/NEU.0000000000000361 |
| [9] |
Lee DY, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation:surgical outcomes in 46 consecutive patients[J]. Mt Sinai J Med, 2006, 73(6): 864-870. |
| [10] |
Linkoaho O, Kivisaari R, Ahonen M. Spinal canal dimensions affect outcome of adolescent disc herniation[J]. J Child Orthop, 2017, 11(5): 380-386. DOI:10.1302/1863-2548.11.170055 |
| [11] |
Kadam G, Narsinghpura K, Deshmukh S, et al. Traumatic lumbar vertebral ring apophysis fracture with disk herniation in an adolescent[J]. Radiol Case Rep, 2017, 12(2): 427-430. DOI:10.1016/j.radcr.2016.11.026 |
| [12] |
Zhou Q, Teng D, Zhang T, et al. Association of facet tropism and orientation with lumbar disc herniation in young patients[J]. Neurol Sci, 2018, 39(5): 841-846. DOI:10.1007/s10072-018-3270-0 |
| [13] |
Choi SJ, Song JS, Kim C, et al. The use of magnetic resonance imaging to predict the clinical outcome of non-surgical treatment for lumbar intervertebral disc herniation[J]. Korean J Radiol, 2007, 8(2): 156-163. DOI:10.3348/kjr.2007.8.2.156 |
| [14] |
Pearson AM, Blood EA, Frymoyer JW, et al. SPORT lumbar intervertebral disk herniation and back pain:does treatment, location, or morphology matter?[J]. Spine(Phila Pa 1976), 2008, 33(4): 428-435. DOI:10.1097/BRS.0b013e31816469de |
| [15] |
Thomas JG, Hwang SW, Whitehead WE, et al. Minimally invasive lumbar microdiscectomy in pediatric patients:a series of 6 patients[J]. J Neurosurg Pediatr, 2011, 7(6): 616-619. DOI:10.3171/2011.3.PEDS10570 |
| [16] |
Cahill J, Frost G, Solanki GA. Paediatric lumbar disc herniation in the very young:a case-based update[J]. Childs Nerv Syst, 2011, 27(5): 687-691. DOI:10.1007/s00381-010-1369-6 |
| [17] |
Tu Z, Wang B, Li L, et al. Early Experience of full-endoscopic interlaminar discectomy for adolescent lumbar disc herniation with sciatic scoliosis[J]. Pain Physician, 2018, 21(1): E63-E70. |
| [18] |
Nellensteijn J, Ostelo R, Bartels R, et al. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations:a systematic review of the literature[J]. Eur Spine J, 2010, 19(2): 181-204. DOI:10.1007/s00586-009-1155-x |
| [19] |
Li H, Jiang C, Mu X, et al. Comparison of MED and PELD in the treatment of adolescent lumbar disc herniation:a 5-year retrospective follow-up[J]. World Neurosurg, 2018, 112: e255-e260. DOI:10.1016/j.wneu.2018.01.030 |
| [20] |
Gulati S, Madsbu MA, Solberg TK, et al. Lumbar microdiscectomy for sciatica in adolescents:a multicentre observational registry-based study[J]. Acta Neurochir(Wien), 2017, 159(3): 509-516. DOI:10.1007/s00701-017-3077-4 |
| [21] |
张红鹤, 赵柳絮, 邓丽, 等. 经皮椎间孔镜椎间盘切除术与椎板开窗髓核摘除术对脊柱运动单位影响的对比研究[J]. 脊柱外科杂志, 2015, 13(4): 223-227. |
| [22] |
Cahill KS, Dunn I, Gunnarsson T, et al. Lumbar microdiscectomy in pediatric patients:a large single-institution series[J]. J Neurosurg Spine, 2010, 12(2): 165-170. DOI:10.3171/2009.9.SPINE09756 |
| [23] |
Lagerbäck T, Elkan P, Möller H, et al. An observational study on the outcome after surgery for lumbar disc herniation in adolescents compared with adults based on the Swedish Spine Register[J]. Spine J, 2015, 15(6): 1241-1247. DOI:10.1016/j.spinee.2015.02.024 |
 2019, Vol.17
2019, Vol.17  Issue(6): 394-399
Issue(6): 394-399


