2. 梅奥医学中心骨科, 罗彻斯特 55901
2. Department of Orthopaedics, Mayo Medical Center, Rochester 55901, Minnesota, USA
青少年特发性脊柱侧凸(AIS)是最常见的脊柱畸形,是一种严重的脊柱三维空间畸形[1-2]。脊柱融合矫正手术是治疗脊柱侧凸的重要手段,其中后路手术应用最为广泛[3-5]。胸椎前方存在大量重要结构(如主动脉、食管等),因椎弓根置钉不佳造成的主动脉损伤虽不多见,但一旦发生后果严重,甚至危及患者生命[6]。相关研究发现,脊柱侧凸手术中胸椎螺钉位置不佳的概率为10% ~ 15%[7-8],置钉穿孔率为1.2% ~ 65.0%[9],其中螺钉误置导致主动脉损伤的发生率为0.29% ~ 1.50%[10-11],主动脉损伤导致的相关死亡率为15% ~ 65%[12],因而了解椎体与主动脉的毗邻关系非常重要。通过术前MRI或CT平扫,可以获得椎体横断面影像,进而了解椎体和主动脉的毗邻关系,但这种影像是在仰卧位获得的,而后路手术中体位却是俯卧位。因此,探究不同体位下椎体和主动脉的毗邻关系具有一定意义。O形臂X线机的应用可辅助术中椎弓根螺钉的安全置入[13],同时可获取术中俯卧位下椎体横断面影像,为研究2种体位下主动脉位置的变化提供依据。本研究通过术前仰卧位MRI和术中俯卧位O形臂X线影像研究2种体位下主胸弯顶椎和主动脉的毗邻关系。
1 资料与方法 1.1 一般资料纳入标准:①综合分析病史、物理检查结果、术前全脊柱正侧位X线和MRI资料,确诊为AIS;②均行单纯后路(标准俯卧位)切开三维矫形植骨融合内固定术;③术中使用O形臂X线机辅助手术,影像资料齐全;④术中O形臂X线机获得的椎体横断面影像资料中主动脉成像清晰;⑤主胸弯为右弯。排除标准:①先天性、神经源性、椎体结构极端异常、遗传性疾病、神经系统结构异常、内分泌系统异常或结缔组织病导致的脊柱侧凸;②年龄 > 18岁或 < 10岁;③无结构性胸弯的AIS(Lenke 5型);④主胸弯Cobb角≤40°或≥100°。根据以上标准,共纳入2013年4月—2018年7月美国梅奥医学中心收治的AIS患者18例,其中男3例、女15例,年龄10 ~ 18(13.50±2.12)岁;Lenke 1型7例,2型7例,3型2例,6型2例;主胸弯顶椎位于T6 1例,T7 4例,T8 8例,T9 3例,T10 2例;主胸弯Cobb角为46.5° ~ 80.7°(60.09°±11.62°);T5~12后凸角为7.3° ~ 52.1°(21.68°±11.36°)。
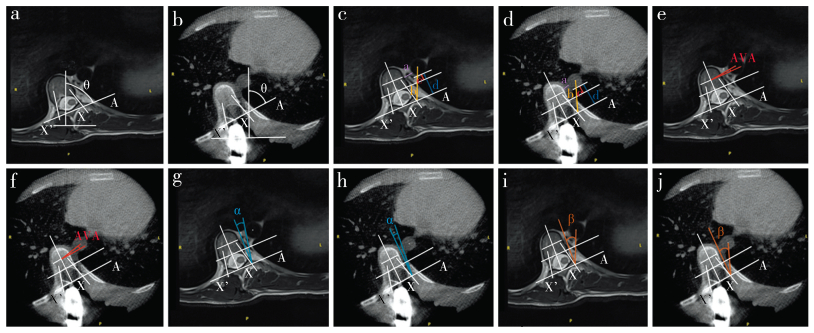
1.2 测量方法及指标将患者术前全脊柱仰卧位MRI和术中俯卧位O形臂X线机(美敦力,美国)采集的影像资料处理后上传至临床图像显示系统(Qreads 5.10),测量以下指标。选择MRI和O形臂X线机平扫中主胸弯顶椎椎弓根最粗的平面,改良Göçen等[14]的方法测量顶椎椎体旋转角(AVR),原方法通过标记椎体横断面两侧椎弓根最后点(X、X’),本研究将其方法进一步改进,X、X’点为通过椎弓根中心的椎弓根轴线与后方骨性结构的交点(可看作椎弓根螺钉左右置钉点),过X、X’点做一条直线(A线),此线与矢状面的夹角为∠θ,AVR为90°-∠θ,椎体向右旋转AVR记为负值,向左旋转记为正值(图 1a,b);主动脉到椎体距离,即主动脉外壁到椎体的最小距离(a线;图 1c,d);主动脉到左侧椎弓根置钉点距离,即左侧椎弓根置钉点X和主动脉中心点的连线与主动脉外壁相交,此交点与X的距离(b线;图 1c,d);主动脉到椎管垂直距离,即经过主动脉后壁和椎管前壁分别作A线的平行线,两线间的垂直距离(c线;图 1c,d);主动脉后壁到椎弓根置钉点连线(A线)的垂直距离(d线;图 1c,d);主动脉椎体角(AVA),即主动脉中心点和椎体中心点连线与A线平行线间的夹角,在测量时如主动脉中心点和椎体中心点连线在A线平行线前方时为正值,反之为负值(图 1e,f);左侧椎弓根置钉点和主动脉内侧切线与椎体中轴线平行线间的夹角(∠α;图 1g,h);左侧椎弓根置钉点和主动脉中心点连线与椎体中轴线平行线间的夹角(∠β;图 1i,j)。
|
男,17岁,Lenke 1 AIS,主胸弯顶椎为T9,术前仰卧位MRI和术中俯卧位X线片测量平面均为T9 a:仰卧位测量AVR b:俯卧位测量AVR c:仰卧位测量a,b,c,d线 d:俯卧位测量a,b,c,d线 e:仰卧位测量AVA f:俯卧位测量AVA g:仰卧位测量∠α h:俯卧位测量∠α i:仰卧位测量∠β j:俯卧位测量∠β Male, 17 years old, Lenke 1 AIS, main thoracic curvature is T9, measurement planes of preoperative MRI in supine position and intraoperative roentgenograph in prone position are T9 a:Measurement of AVR in supine position b:Measurement of AVR in prone position c:Measurement of line a, b, c and d in supine position d:Measurement of line a, b, c and d in prone position e:Measurement of AVA in supine position f:Measurement of AVA in prone position g:Measurement of ∠α in supine position h:Measurement of ∠α in prone position i:Measurement of ∠β in supine position j:Measurement of ∠β in prone position 图 1 2种体位下测量脊柱侧凸病例主胸弯顶椎与主动脉毗邻关系的影像学资料 Fig. 1 Imaging data of adjacent relationship of apical vertebra of main thoracic curvature with aorta in 2 positions of scoliosis patients |
采用SPSS 25.0软件对数据进行统计学分析,计量资料采用x±s表示,2种体位数据差异比较采用配对样本t检验,采用Pearson相关分析对数据进行相关性检验;以P < 0.05为差异有统计学意义。
2 结果患者术前仰卧位MRI和术中俯卧位O形臂X线机测量主胸弯顶椎主动脉与椎体毗邻关系见表 1。俯卧位AVR大于仰卧位,平均差值为2.71°,差异有统计学意义(P < 0.05);俯卧位c线大于仰卧位,平均差值为2.24 mm,差异有统计学意义(P < 0.05);俯卧位AVA与仰卧位平均差值为4.45°,差异有统计学意义(P < 0.05),数值由负转正,说明主动脉向椎体右前方移动;俯卧位和仰卧位a线、b线、d线、∠α、∠β差异无统计学意义(P > 0.05)。
|
|
表 1 两种体位下测量主胸弯顶椎与主动脉毗邻关系 Tab. 1 Measurement of adjacent relationship of apical vertebra of main thoracic curvature with aorta in 2 positions |
俯卧位AVR、a线、b线、c线、d线、AVA、∠α、∠β与仰卧位相应指标均呈正相关(r=0.531、0.624、0.761、0.742、0.700、0.675、0.609、0.699)。俯卧位∠β与主胸弯Cobb角呈正相关(r=0.682),与俯卧位及仰卧位AVR均呈负相关(r=-0.526、-0.575);俯卧位d线与主胸弯Cobb角呈负相关(r=-0.583),与俯卧位及仰卧位AVR呈正相关(r=0.624、0.480)。
3 讨论AIS手术矫正治疗中使用椎弓根螺钉,由于胸椎和胸主动脉的位置比较接近,螺钉位置不佳会发生胸主动脉损伤,后果严重[9, 15-16]。正常脊柱主动脉在T4水平向下形成降主动脉,位于椎体左前方,大约在T12水平穿过膈肌进入腹腔。脊柱侧凸导致的椎体变形、旋转、移位都伴随着主动脉位置变化。Sucato等[17]的研究发现,脊柱侧凸患者主动脉的位置较正常人更偏向外侧和后方,提示脊柱侧凸患者后路手术置钉时,较无脊柱侧凸患者发生主动脉损伤的可能性增加。此外,各患者畸形情况不同,侧凸或后凸角度不同,主动脉的位置变化也不一致[18]。MRI和CT检查时患者处于仰卧位,而患者手术时多为俯卧位,体位变化时椎体的畸形会发生部分变化,主动脉相对于椎体的毗邻关系也将发生变化,因此,用术前仰卧位的影像指导俯卧位手术可能存在一定偏差。获知术中实际体位下椎体畸形情况和主动脉位置信息,可为术中安全置钉提供保障。
O形臂X线机的应用不仅提供了术中安全置钉的3D影像辅助,同时也提供了患者俯卧位状态下胸椎和胸主动脉的位置毗邻关系。本研究发现,俯卧位AVR较仰卧位大,平均增加2.71°,提示术中置钉时的外展角度亦适度增大,考虑出现这种现象的原因是仰卧位时“剃刀背”区的肋骨直接受到仪器检查台的力量,传导至椎体时产生向左旋转的力量,导致AVR在仰卧位时比俯卧位时小;俯卧位主动脉到椎管垂直距离(c线)大于仰卧位,平均差值为2.24 mm,说明主动脉在顶椎水平向前方远离椎管区;俯卧位AVA时仰卧位的平均差值为4.45°,数值由负转正,进一步说明主动脉向椎体右前方移动。
本研究相关性分析结果显示,2种体位下AVR、a线、b线、c线、d线、AVA、∠α、∠β均呈正相关。俯卧位∠β与主胸弯Cobb角呈正相关,俯卧位d线与主胸弯Cobb角呈负相关,说明冠状面畸形越大,顶椎左侧椎弓根进针点在椎体横断面上与主动脉的成角越大,左侧椎弓根进针点到主动脉外壁的垂直距离越小。俯卧位∠β与AVR呈负相关,俯卧位d线与AVR呈正相关(测量时规定椎体向右旋转数值为负值),说明顶椎旋转越明显,顶椎左侧椎弓根进针点在椎体横断面上与主动脉的成角越大,左侧椎弓根进针点到主动脉外壁的垂直距离越小。
通过本研究的数据分析,同一患者俯卧位对比仰卧位,主动脉会远离顶椎区。不同患者主胸弯Cobb角越大,主动脉离左侧椎弓根进针点垂直距离越小;顶椎椎体旋转越大,顶椎左侧椎弓根进针点在横断面上与主动脉成角越大,说明患者顶椎旋转越大,置钉时只要掌握好置钉外展角度,风险反而降低,损伤主动脉的可能性随之降低。
综上所述,相较于仰卧位MRI数据,AIS患者俯卧位时顶椎旋转度增大,主动脉到椎管垂直距离增大,主动脉向椎体右前方移动。本研究样本量偏小,因为术中使用O形臂X线机获得椎体横断面影像资料时采用了骨算法进行数据重建,以便为置钉提供骨性结构图像,导致软组织分辨率明显下降,无法区分主动脉和周围软组织影,顶椎区主动脉显影清晰病例资料明显减少。下一步的研究可针对单一Lenke亚型患者进行分析。
| [1] |
Tambe AD, Panikkar SJ, Millner PA, et al. Current concepts in the surgical management of adolescent idiopathic scoliosis[J]. Bone Joint J, 2018, 100-B(4): 415-424. DOI:10.1302/0301-620X.100B4.BJJ-2017-0846.R2 |
| [2] |
Romano M, Minozzi S, Zaina F, et al. Exercises for adolescent idiopathic scoliosis:a Cochrane systematic review[J]. Spine(Phila Pa 1976), 2013, 38(14): E883-E893. DOI:10.1097/BRS.0b013e31829459f8 |
| [3] |
Jada A, Mackel CE, Hwang SW, et al. Evaluation and management of adolescent idiopathic scoliosis:a review[J]. Neurosurg Focus, 2017, 43(4): E2. DOI:10.3171/2017.7.FOCUS17297 |
| [4] |
El-Hawary R, Chukwunyerenwa C. Update on evaluation and treatment of scoliosis[J]. Pediatr Clin North Am, 2014, 61(6): 1223-1241. DOI:10.1016/j.pcl.2014.08.007 |
| [5] |
Kim HJ, Blanco JS, Widmann RF. Update on the management of idiopathic scoliosis[J]. Curr Opin Pediatr, 2009, 21(1): 55-64. DOI:10.1097/MOP.0b013e328320a929 |
| [6] |
Pesenti S, Bartoli MA, Blondel B, et al. Endovascular aortic injury repair after thoracic pedicle screw placement[J]. Orthop Traumatol Surg Res, 2014, 100(5): 569-573. DOI:10.1016/j.otsr.2014.03.020 |
| [7] |
Ughwanogho E, Patel NM, Baldwin KD, et al. Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal[J]. Spine(Phila Pa 1976), 2012, 37(8): E473-E478. DOI:10.1097/BRS.0b013e318238bbd9 |
| [8] |
Baghdadi YM, Larson AN, McIntosh AL, et al. Complications of pedicle screws in children 10 years or younger:a case control study[J]. Spine(Phila Pa 1976), 2013, 38(7): E386-E393. DOI:10.1097/BRS.0b013e318286be5d |
| [9] |
Kwan MK, Chiu CK, Gani SM, et al. Accuracy and safety of pedicle screw placement in adolescent idiopathic scoliosis patients:a review of 2020 screws using computed tomography assessment[J]. Spine(Phila Pa 1976), 2017, 42(5): 326-335. DOI:10.1097/BRS.0000000000001738 |
| [10] |
Parker SL, Amin AG, Santiago-Dieppa D, et al. Incidence andclinical significance of vascular encroachment resulting fromfreehand placement of pedicle screws in the thoracic and lumbarspine:analysis of 6816 consecutive screws[J]. Spine(Phila Pa 1976), 2014, 39(8): 683-687. DOI:10.1097/BRS.0000000000000221 |
| [11] |
Sarwahi V, Suggs W, Wollowick AL, et al. Pedicle screws adjacentto the great vessels or viscera:a study of 2132 pedicle screws inpediatric spine deformity[J]. J Spinal Disord Tech, 2014, 27(2): 64-69. DOI:10.1097/BSD.0b013e31825bfecd |
| [12] |
Papadoulas S, Konstantinou D, Kourea HP, et al. Vascular injury complicating lumbar discsurgery. A systematic review[J]. Eur J Vasc Endovasc Surg, 2002, 24(3): 189-195. DOI:10.1053/ejvs.2002.1682 |
| [13] |
Zhang W, Takigawa T, Wu Y, et al. Accuracy of pedicle screw insertion in posterior scoliosis surgery:a comparison between intraoperative navigation and preoperative navigation techniques[J]. Eur Spine J, 2017, 26(6): 1756-1764. DOI:10.1007/s00586-016-4930-5 |
| [14] |
Göçen S1, Havitçioğlu H, Alici E. A new method to measure vertebral rotation from CT scans[J]. Eur Spine J, 1999, 8(4): 261-265. DOI:10.1007/s005860050170 |
| [15] |
Fouquet O, Loubière H, Talha A, et al. A pedicle screw in the descending thoracic aorta:a surgical approach[J]. Eur J Cardiothorac Surg, 2013, 44(2): 391-392. DOI:10.1093/ejcts/ezt151 |
| [16] |
Şarlak AY, Buluç L, Sarısoy HL, et al. Placement of pedicle screws in thoracic idiopathic scoliosis:a magnetic resonance imaging analysis of screw placement relative to structures at risk[J]. Eur Spine J, 2008, 17(5): 657-662. DOI:10.1007/s00586-008-0639-4 |
| [17] |
Sucato DJ, Duchene C. The position of the aorta relative to the spine:a comparison of patients with and without idiopathic scoliosis[J]. J Bone Joint Surg Am, 2003, 85-A(8): 1461-1469. |
| [18] |
Larson AN, Santos ER, Polly DW Jr, et al. Pediatric pedicle screw placement using intraoperative computed tomography and 3-dimensional image-guided navigation[J]. Spine(Phila Pa 1976), 2012, 37(3): E188-E194. DOI:10.1097/BRS.0b013e31822a2e0a |
 2019, Vol.17
2019, Vol.17  Issue(6): 404-408
Issue(6): 404-408


