2. 解放军第947医院骨科, 喀什 844200
2. Department of Orthopaedics, No. 947 Hospital of Chinese PLA, Kashi 844200, Xinjiang Uyghur Autonomous Region, China
胸腰椎骨质疏松性椎体压缩性骨折(OVCF)好发于中老年人,常引起严重的背部疼痛、胸腰椎后凸畸形,降低患者生活质量、增加死亡风险。传统的非手术治疗主要是长期卧床、佩戴支具及使用抗骨质疏松药物。非手术治疗是临床治疗OVCF的常用方法,可有效缓解骨折引起的疼痛,但可导致骨折进一步加重,尤其对于老年患者,可能引发多种并发症,如肺炎、深静脉血栓、泌尿系统感染等,最终导致患者生活质量严重下降[1-2]。由于骨质疏松,开放性骨折复位内固定术并不适合[3]。近年来,随着微创技术的发展,经皮椎体成形术(PVP)成为治疗OVCF的常用术式,其具有创伤小、术后疼痛症状改善明显、患者恢复快等优势,但也存在骨水泥渗漏、神经损伤、血管栓塞、再骨折等并发症[4]。目前,临床上对于PVP术中骨水泥的具体使用量尚存争议,本研究在PVP术中分别采用小剂量(≥2.5 mL且 < 4.0 mL)和大剂量(≥4.0 mL且 < 6.0 mL)骨水泥治疗老年单椎体OVCF,以探讨骨水泥最佳注入量,为临床治疗OVCF提供参考。
1 资料与方法 1.1 一般资料病例纳入标准:①年龄 > 60岁,经骨密度检查证实为骨质疏松症;②经影像学检查证实为单椎体OVCF;③骨折节段T11 ~ L2;④MRI检查证实背痛与骨折关系密切;⑤随访时间 > 1年。排除标准:①合并脊柱恶性肿瘤、结核等病变;②合并脏器衰竭,全身评估不能耐受手术;③有脊髓或马尾神经损伤等表现;④存在骨代谢性疾病;⑤严重的退行性脊柱畸形。根据以上标准,共纳入2017年7月—2018年7月在海军军医大学附属长征医院接受PVP治疗的老年胸腰椎单椎体OVCF患者122例,其中51例患者术中注入小剂量骨水泥(小剂量组,≥2.5 mL且 < 4.0 mL),71例患者术中注入大剂量骨水泥(大剂量组,≥4.0 mL且 < 6.0 mL)。2组患者术前一般资料差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 2组患者一般资料 Tab. 1 General data of 2 groups |
患者取俯卧位,常规碘伏消毒后采用双侧入路,在C形臂X线机透视下确定骨折椎体椎弓根,采用1%利多卡因进行局部麻醉,透视下确定穿刺针位于伤椎椎弓根内,穿刺至椎体前1/3,在C形臂X线机透视下将针尖调整后,向损伤的椎体内注入拉丝期的骨水泥。待骨水泥凝固后拔出穿刺针。术后24 h患者可佩戴支具下床活动。
1.3 观察指标记录2组患者手术前后疼痛视觉模拟量表(VAS)评分[5]、椎体前缘高度,根据患者术后影像学资料判断骨水泥渗漏情况。
1.4 统计学处理采用SPSS 25.0软件对数据进行统计学分析,计量资料以x±s表示,组间比较采用独立样本t检验,同组手术前后比较采用配对t检验;计数资料比较采用χ2检验;以P < 0.05为差异有统计学意义。
2 结果2组患者术后1个月、1年VAS评分均较术前明显改善,差异有统计学意义(P < 0.05,表 2),术后各时间点组间比较差异无统计学意义(P > 0.05)。2组患者术后1年伤椎前缘高度均较术前显著改善,且大剂量组改善程度优于小剂量组,差异均有统计学意义(P < 0.05,表 2)。
|
|
表 2 2组患者统计数据 Tab. 2 Statistical data of 2 groups |
大剂量组术中发生骨水泥渗漏10例(14.08%),其中椎间盘渗漏6例、静脉渗漏1例及椎旁渗漏3例;小剂量组术中发生骨水泥渗漏3例(5.88%),其中椎间盘渗漏2例、椎旁渗漏1例。2组骨水泥渗漏率差异无统计学意义(P > 0.05)。2组均未发生肺栓塞、神经损伤等严重并发症。典型病例影像学资料见图 1、2。
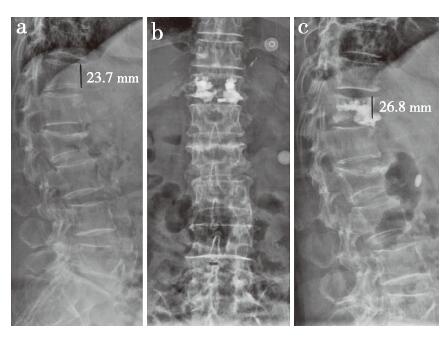
|
女,79岁,T12 OVCF a:术前椎体高度23.7 mm,L2为陈旧性骨折 b:骨水泥注入量4.5 mL,术后X线片示骨水泥椎间盘渗漏 c:术后1年椎体高度26.8 mm Female, 79 years old, T12 OVCF a:Preoperative height of injured vertebra is 23.7 mm, L2 old fracture b:Bone cement injection is 4.5 mL, and postoperative anteroposterior roentgenograph shows intervertebral disc leakage of bone cement c:Height of injured vertebra at postoperative 1 year is 26.8 mm 图 1 大剂量组典型病例影像学资料 Fig. 1 Imaging data of a typical case in high-dose group |
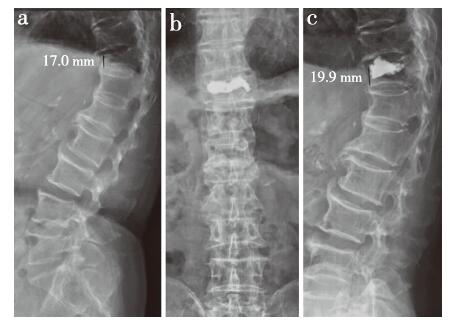
|
男,83岁,T11 OVCF a:术前椎体高度17.0 mm b:骨水泥注入量3.0 mL,术后X线片示骨水泥椎间盘渗漏 c:术后1年椎体高度19.9 mm Male, 83 years old, T11 OVCF a:Preoperative height of injured vertebra is 17.0 mm b:Bone cement injection is 3.0 mL, and postoperative anteroposterior roentgenograph shows intervertebral disc leakage of bone cement c:Height of injured vertebra at postoperative 1 year is 19.9 mm 图 2 小剂量组典型病例影像学资料 Fig. 2 Imaging data of a typical case in low-dose group |
骨质疏松症是临床较为常见的老年性疾病,不仅引起临床症状,还伴随严重的并发症。胸腰椎压缩性骨折是骨质疏松症较为常见的并发症,具有较高的致残率和死亡率[6]。PVP是一种安全、有效的治疗胸腰椎OVCF的微创手术方式,患者术后疼痛缓解明显,短期内可下床活动,治疗效果满意[7]。PVP可重建脊柱稳定性、纠正畸形、促进骨折早期愈合[8]。Lou等[9]对PVP与非手术治疗OVCF的效果进行荟萃分析,发现PVP仅对治疗新鲜OVCF有明确的效果,并可明显缓解疼痛症状,对陈旧性OVCF或临床症状较轻患者效果较差。而Graziotti等[10]的临床随机对照研究表明,与假手术组相比,PVP在缓解疼痛和改善功能方面均无优势。Ebeling等[11]也认为,对于急性疼痛性椎体骨折,目前的证据尚不足以支持继续使用椎体成形术治疗。然而,本研究结果表明,不同剂量的骨水泥均可以达到缓解临床症状的目的,提高患者的生活质量。Van Meirhaeghe等[12]的研究也表明,骨水泥注入后可明显缓解疼痛,且疼痛缓解程度与骨水泥注入量无明显相关性。
PVP可通过注入骨水泥恢复患椎高度,提高脊柱稳定性[13]。骨水泥注入剂量是影响PVP手术疗效的重要因素,小剂量骨水泥难以固定连接断裂的骨小梁,不能恢复椎体的机械性能;而大剂量骨水泥则有发生骨水泥渗漏的风险,导致神经受损、肺栓塞等,危及生命[14]。Gaughen等[15]的研究发现,注入足够量的骨水泥是预防椎体再次压缩的关键因素。Guarnieri等[16]也发现,大剂量骨水泥有利于恢复椎体前缘高度,进而促进脊柱力线恢复。也有研究表明,同大剂量骨水泥相比,小剂量骨水泥可以降低PVP术中发生并发症的风险,且同样具有维持椎体稳定性的作用[17]。本研究结果提示,大量骨水泥更有利于伤椎前缘高度的恢复,重塑脊柱正常力线,恢复脊柱正常的生理功能。
骨水泥渗漏是PVP的严重并发症,有研究发现,椎体压缩程度高和骨折节段数多是骨水泥椎间盘渗漏的危险因素;骨水泥注射量大和椎体压缩程度高是骨水泥软组织渗漏的危险因素;女性和低龄是骨水泥血管内渗漏的危险因素;骨水泥注射量大和椎体终板/后壁破裂是骨水泥椎管内渗漏的危险因素[18]。Chen等[19]的研究发现,骨水泥渗入椎间隙虽然不影响最终临床疗效,但可能增加邻近节段再骨折的风险。陈家麟等[20]的研究也发现,骨水泥渗漏及邻近椎体骨折与骨水泥注射量密切相关。Sun等[21]的研究发现,增加骨水泥注射量并不会增加骨水泥渗漏的风险,骨水泥渗漏可能与骨水泥本身特性有关。以往为了有效预防骨水泥渗漏引起的各种并发症,如神经损伤、肺栓塞等,术中通常采用小剂量骨水泥。本研究结果显示,不同剂量骨水泥渗漏率差异无统计学意义,为了减少骨水泥的渗漏,本研究术中采取套筒内置入适量明胶海绵,待骨水泥进入拉丝期再进行注入。
综上,PVP术中注入不同剂量骨水泥治疗老年单椎体OVCF均可获得良好的临床效果,改善患者临床症状,恢复脊柱功能,且注入大剂量骨水泥可更有效地恢复椎体高度。但本研究样本量小,且为回顾性研究,结论仍有待更大样本量的前瞻性随机对照研究进一步验证。
| [1] |
Burger H, Van Daele PL, Grashuis K, et al. Vertebral deformities and functional impairment in men and women[J]. J Bone Miner Res, 1997, 12(1): 152-157. DOI:10.1359/jbmr.1997.12.1.152 |
| [2] |
Yang EZ, Xu JG, Huang GZ, et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures[J]. Spine(Phila Pa 1976), 2016, 41(8): 653-660. DOI:10.1097/BRS.0000000000001298 |
| [3] |
Lange A, Kasperk C, Alvares L, et al. Survival and cost comparison of kyphoplasty and percutaneous vertebroplasty using German claims data[J]. Spine (Phila Pa 1976), 2014, 39(4): 318-326. DOI:10.1097/BRS.0000000000000135 |
| [4] |
Chen X, Ren J, Zhang J, et al. Impact of cement placement and leakage in osteoporotic vertebral compression fractures followed by percutaneous vertebroplasty[J]. Clin Spine Surg, 2016, 29(7): E365-E370. DOI:10.1097/BSD.0b013e3182aa28d6 |
| [5] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [6] |
Yimin Y, Zhiwei R, Wei M, et al. Current status of percutaneous vertebroplasty and percutaneous kyphoplasty—a review[J]. Med Sci Monit, 2013, 19: 826-836. DOI:10.12659/MSM.889479 |
| [7] |
蔡斌, 王文军, 宋西正, 等. 遥控骨水泥自动推进器辅助下经皮椎体成形术治疗骨质疏松性胸腰椎压缩性骨折[J]. 中国矫形外科杂志, 2016, 24(10): 865-869. |
| [8] |
王庚启, 谢林, 洪友松, 等. 经皮椎体成形术治疗骨质疏松性胸腰椎椎体压缩性骨折[J]. 脊柱外科杂志, 2009, 7(4): 245-247. |
| [9] |
Lou S, Shi X, Zhang X, et al. Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures:a meta-analysis of randomized controlled trials[J]. Osteoporos Int, 2019, 30(12): 2369-2380. DOI:10.1007/s00198-019-05101-8 |
| [10] |
Graziotti PJ. Vertebroplasty appears no better than placebo for painful osteoporotic spinal fractures, and has potential to cause harm[J]. Med J Aust, 2010, 192(3): 174. DOI:10.5694/j.1326-5377.2010.tb03467.x |
| [11] |
Ebeling PR, Akesson K, Bauer DC, et al. The efficacy and safety of vertebral augmentation:a second ASBMR task force report[J]. J Bone Miner Res, 2019, 34(1): 3-21. DOI:10.1002/jbmr.3653 |
| [12] |
Van Meirhaeghe J, Bastian L, Boonen S, et al. A randomized trial of balloon kyphoplasty and nonsurgical management for treating acute vertebral compression fractures:vertebral body kyphosis correction and surgical parameters[J]. Spine(Phila Pa 1976), 2013, 38(12): 971-983. DOI:10.1097/BRS.0b013e31828e8e22 |
| [13] |
Baerlocher MO, Saad WE, Dariushnia S, et al. Quality improvement guidelines for percutaneous vertebroplasty[J]. J Vasc Interv Radiol, 2014, 25(2): 165-170. DOI:10.1016/j.jvir.2013.09.004 |
| [14] |
Jin YJ, Yoon SH, Park KW, et al. The volumetric analysis of cement in vertebroplasty:relationship with clinical outcome and complications[J]. Spine(Phila Pa 1976), 2011, 36(12): E761-E772. DOI:10.1097/BRS.0b013e3181fc914e |
| [15] |
Gaughen JR Jr, Jensen ME, Schweickert PA, et al. The therapeutic benefit of repeat percutaneous vertebroplasty at previously treated vertebral levels[J]. AJNR Am J Neuroradiol, 2002, 23(10): 1657-1661. |
| [16] |
Guarnieri G, Tecame M, Izzo R, et al. Vertebroplasty using calcium triglyceride bone cement(Kryptonite?)for vertebral compression fractures. A single-centre preliminary study of outcomes at one-year follow-up[J]. Interv Neuroradiol, 2014, 20(5): 576-582. DOI:10.15274/INR-2014-10060 |
| [17] |
Takahara K, Kamimura M, Moriya H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women[J]. BMC Musculoskeletal Disorders, 2016, 17: 12. DOI:10.1186/s12891-016-0887-0 |
| [18] |
王惠东, 姚方超, 傅智轶, 等. 大剂量骨水泥经皮椎体成形术治疗老年胸腰椎骨折的疗效及其影响因素[J]. 创伤外科杂志, 2019, 21(5): 340-345. |
| [19] |
Chen LH, Hsieh MK, Liao JC, et al. Repeated percutaneous vertebroplasty for refracture of cemented vertebrae[J]. Arch Orthop Trauma Surg, 2011, 131(7): 927-933. DOI:10.1007/s00402-010-1236-7 |
| [20] |
陈家麟, 陈晞, 杨军, 等. 椎体成形治疗中骨水泥渗漏的因素与临床分析[J]. 中国组织工程研究, 2017, 21(30): 4763-4768. |
| [21] |
Sun H, Li C. Comparison of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures:a systematic review and meta-analysis[J]. J Orthop Surg Res, 2016, 11(1): 156. |
 2020, Vol.18
2020, Vol.18  Issue(5): 289-292, 314
Issue(5): 289-292, 314


