骨质疏松性骨折严重危害社会公众健康,年龄超过50岁的人群30% ~ 50%为骨质疏松性骨折高危人群,其中,椎体骨折是最常见类型,年龄超过70岁的人群和绝经后妇女尤为多见[1]。有报道证实,经皮椎体后凸成形术(PKP)治疗骨质疏松性椎体压缩性骨折(OVCF)具有一定优势[2-4]。压力引导式经皮椎体后凸成形术(PG-PKP)由本研究组首次提出并应用于胸腰段OVCF患者,该术式操作原理是经双侧椎弓根入路穿刺定位,保证球囊扩张后双侧通道互通,在椎体压缩严重一侧注入骨水泥,另一侧作为低压区引导骨水泥的流向,进而减少骨水泥渗漏,临床疗效满意[5]。目前,有关中段胸椎OVCF的手术治疗研究颇少,尚无满意的手术方法[6-8]。本研究借鉴PG-PKP在胸腰段OVCF的成功应用,利用PG-PKP治疗中段胸椎OVCF,手术疗效满意,骨水泥渗漏率低,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄 > 60岁,骨密度T值< -2;②症状、体征与影像学检查结果相符;③无神经受压症状;④MRI示T5~8新鲜单椎体骨折;⑤影像学资料及功能评分数据完整。排除标准:①影像学检查提示椎管内压迫 > 30%;②合并血液系统疾病;③合并脊柱肿瘤、感染性疾病。根据上述标准,2017年1月—2019年8月纳入中段胸椎OVCF患者39例,其中男23例、女16例,年龄60 ~ 87(73.56±6.13)岁。根据手术方式分为PG-PKP组(A组,20例)和传统PKP组(B组,19例),2组患者年龄、性别、骨密度T值及骨折部位差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 2组患者一般资料 Tab. 1 General information of 2 groups |
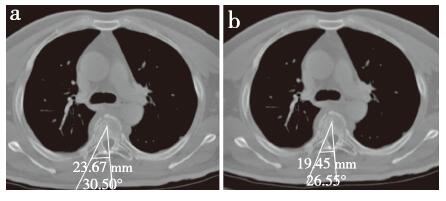
所有患者术前均行骨折部位X线、CT和MRI检查。在CT平扫椎弓根横径最大平面测量2种术式手术通道影像学参数。PG-PKP手术通道根据“一点一切线”原则,x点为椎体矢状位正中线前、中1/3交点,由经过x点与双侧椎弓根外侧壁切线为PG-PKP手术通道(图 1a);传统PKP手术通道根据“两点一线”原则,x点为椎体矢状位正中线前、中1/3交点,y点为椎弓根中点,x、y连线为传统PKP手术通道(图 1b)。

|
a:PG-PKP手术通道b:传统PKP手术通道 a:PG-PKP operation channel b:Traditional PKP operation channel 图 1 手术通道CT示意图 Fig. 1 CT schematic diagram of operation channel |
患者全身麻醉,俯卧于腰床上,胸骨中线下方向放置圆柱垫,避免骨性结构影响术中透视。根据术前CT定位的手术通道测量通道水平线夹角、骨性进针点与脊柱中线距离,测量方法见图 2。在C形臂X线机透视下定位并标记皮肤进针点,正位透视下穿刺针位于双侧椎弓根外上缘(左侧11点、右侧1点位置),侧位透视穿刺针位于椎弓根顶端,根据透视影像调整矢状面进针角度,在穿刺针位于双侧椎弓根内缘时,侧位透视穿刺针位于椎体后壁。A组依次利用骨导向器、椎体扩张球囊导管操作保证双侧通道能够相通,选择压缩严重一侧注入骨水泥,另一侧作为低压区引导骨水泥流向。B组直接注入骨水泥。2组患者手术操作均在C形臂X线机透视下进行,每注入0.2 mL骨水泥均透视观察填充情况,当骨水泥即将达到椎体后壁时立即停止注射。伤口无需缝合,敷料加压包扎。术后6 h可下床活动,鼓励患者早期进行功能锻炼。术后应用碳酸钙D3咀嚼片(1.25 g,每日2次)、鲑鱼降钙素鼻喷剂(50 U,每日2次)治疗骨质疏松。
|
a:PG-PKP手术通道水平线夹角为30.50°,骨性进针点与脊柱中线距离为23.67 mm b:传统PKP手术通道水平线夹角为26.55°,骨性进针点与脊柱中线距离为19.45 mm a:Angle between horizontal line of PG-PKP operation channel is 26.55°, and distance between bony puncture point and midline of spine is 23.67 mm b:Angle between horizontal line of traditional PKP operation channel is 30.50°, and distance between bony puncture point and midline of spine is 19.45 mm 图 2 手术通道影像学参数CT示意图 Fig. 2 CT schematic diagram of imaging parameters of operation channel |
所有患者术前均完善骨密度T值、X线、CT及MRI检查,并于术后1 d、3个月复查X线片,术后1 d复查CT。在侧位X线片上测量骨折椎体后凸Cobb角(骨折椎体上终板水平线垂线与下终板水平线垂线间的夹角)。在术前CT上测量手术通道水平线夹角、骨性进针点与脊柱中线距离,在术后CT上观察骨水泥渗漏情况。采用疼痛视觉模拟量表(VAS)评分[9]和Oswestry功能障碍指数(ODI)[10]评估临床疗效。记录并发症发生情况。
1.5 统计学处理利用SPSS 19.0软件对数据进行统计学分析,数据以x±s表示,2组患者年龄、骨密度T值、手术前后影像学参数、VAS评分及ODI比较采用独立样本t检验,2组骨水泥渗漏率比较采用非参数方法Kruskal-Wallis检验;以P < 0.05为差异有统计学意义。
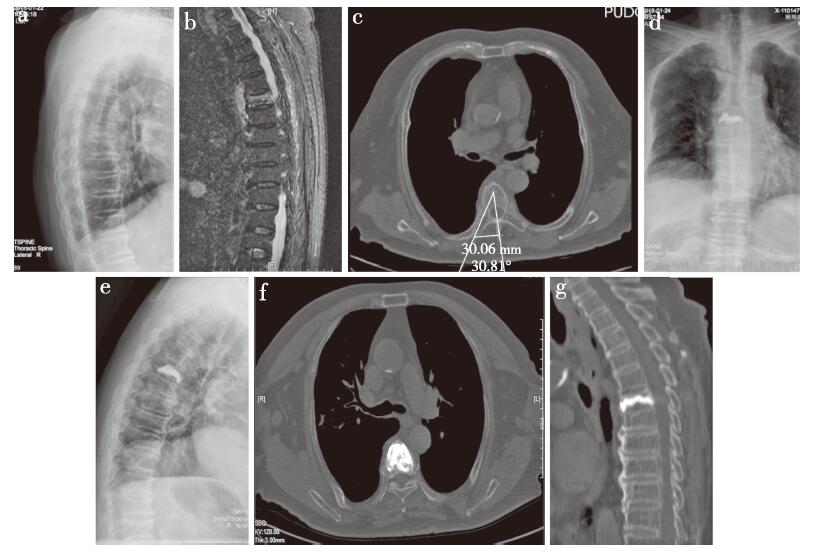
2 结果所有手术顺利完成,术后随访3 ~ 12(8.64±2.84)个月。手术时间40 ~ 90(63.33±13.59)min,住院时间4 ~ 8(6.15±1.16)d。A组手术通道水平线夹角、骨性进针点与脊柱中线距离大于B组,差异均有统计学意义(P < 0.05,表 2)。2组患者术后1 d、术后3个月的椎体前缘高度、伤椎后凸Cobb角、VAS评分、ODI均较术前明显改善,差异均有统计学意义(P < 0.05,表 2)。A组椎体前缘高度、伤椎后凸Cobb角术后改善优于B组,骨水泥注入量多于B组,骨水泥渗漏率低于B组,差异均有统计学意义(P < 0.05,表 2)。骨水泥渗漏情况:A组1例沿椎前渗漏,1例沿椎体侧方渗漏;B组3例沿椎前渗漏,1例沿椎体侧方渗漏,1例沿椎间隙渗漏。术后切口均一期愈合,无骨水泥渗漏致脏器栓塞及脊髓、神经根受压等并发症发生。A组典型病例影像学资料见图 3。
|
|
表 2 2组影像学参数及临床疗效 Tab. 2 Imaging parameters and clinical efficacy in 2 groups |
|
男,84岁,T7 OVCF a、b:术前X线片和MRI示T7压缩性骨折c:术前CT上测量PG-PKP手术通道水平面夹角为30.81°,骨性进针点距离脊柱后正中线30.06 mm d、e:术后3个月胸椎正侧位X线片示骨折椎体前缘高度、后凸Cobb角恢复满意f、g:术后1 d CT示骨水泥椎体内弥散分布满意,无椎旁渗漏 Male, 84 years old, T7 OVCF a, b:Preoperative roentgenograph and MRI show T7 compression fracture c:Preoperative CT measurement of angle between horizontal line and operation channel is 30.81°, and distance between bony puncture point and midline is 30.06 mm d, e:Anteroposterior and lateral roentgenographs at postoperative 3 months show that height of anterior vertebral and Cobb's angle recover satisfactorily f, g:CTs at postoperative 1 d show distribution of cement in vertebral body is satisfactory without paravertebral leakage 图 3 A组典型病例影像学资料 Fig. 3 Imaging data of a typical case in group A |
韩华等[11]报道了不同国家人群胸椎椎弓根的解剖特点,中国人群椎弓根高度从T1至T12逐渐增大,椎弓根宽度则是先减小后增大的变化趋势,最小值位于T4或T5水平,椎弓根水平面夹角从T1至T10呈逐渐减小趋势,T5至T8平均值分别为13.1°、11.2°、9.6°和8.7°。本研究结果显示,PG-PKP组和传统PKP组手术通道水平面夹角均明显大于上述数值,主要是由于韩华等[11]利用椎体前缘中点与椎弓根中点连线测量水平面夹角,而本研究组利用椎体矢状位正中线前、中1/3交点与椎弓根外侧壁切线或椎弓根中点连线测量水平面夹角。同时,本研究结果显示,PG-PKP组手术通道水平面夹角大于传统PKP组,可保证双侧穿刺通道球囊扩张后能够相通,一方面可有效地恢复骨折椎体高度,另一方面可降低骨水泥渗漏率。且中段胸椎由于周围肋骨、肩胛骨和肱骨遮挡,导致术中透视困难,本研究组采用Bayley等[12]报道的方法,将患者俯卧位置于腰床,双侧手臂保持内收并用胶带固定,将圆柱形支撑垫轴向放置在胸骨中线下,使肩胛骨、肱骨有效下垂避免遮挡术中侧位透视。
3.2 PKP治疗中段胸椎OVCF的骨水泥渗漏率传统PKP治疗中上胸椎OVCF报道较少,有关骨水泥渗漏数据亦不完善。Liu等[13]报道采用PKP和PVP治疗101例中段胸椎OVCF患者,共111个手术节段,2组骨水泥渗漏率分别为63.5%和48.6%,组间差异无统计学意义(P > 0.05),2组椎管内骨水泥渗漏率分别为5.4%和20.3%,组间差异有统计学意义(P < 0.05)。梁道臣等[14]报道45例CT引导下PKP治疗的T2~6 OVCF患者,总体骨水泥渗漏率为8.9%,其中2例骨水泥渗漏至椎管后壁,但未造成严重后果。赵兵德等[15]采用单侧经肋-椎弓根入路PKP治疗36例T4~8 OVCF患者,其中9例发生骨水泥渗漏,渗漏率为25%,其中1例出现椎管内渗漏,但未出现脊髓、神经根损伤症状,提示该手术入路存在损伤胸腔脏器的风险,且骨水泥渗漏率并不优于其他入路。本研究结果显示,PG-PKP组骨水泥渗漏率为10.00%,较传统PKP组26.32%的骨水泥渗漏率明显降低,且未见脊髓、神经根损伤等并发症发生,考虑原因可能是术中透视下一旦发现骨水泥即将到达椎体后壁时立即停止注射,等待骨水泥黏稠性增加、调整手术通道位置后再在连续透视下缓慢推注,避免了骨水泥经椎体后壁向椎管内渗漏。
3.3 PG-PKP特点及注意事项首先,须根据术前CT确定手术通道水平面夹角和骨性进针点;其次,术中根据术前影像学指标采用双侧经椎弓根外侧壁入路进行定位穿刺、椎体球囊扩张,球囊扩张后可保证双侧通道互通;最后,在椎体压缩严重侧注入骨水泥,另一侧作为低压区引导通道引流骨水泥,术中透视证实骨水泥充填满意后封堵引导侧通道,可有效减少骨水泥渗漏。
综上,与传统PKP相比,PG-PKP治疗中段胸椎OVCF也可取得满意疗效,且椎体高度、后凸Cobb角度恢复满意、骨水泥渗漏率低,值得临床推广。但本研究为回顾性分析,样本量较少、随访时间较短,未来可采用大样本前瞻性随机对照研究来评估PG-PKP治疗中段胸椎OVCF的手术疗效及中远期并发症。
| [1] |
Ballane G, Cauley JA, Luckey MM, et al. Worldwide prevalence and incidence of osteoporotic vertebral fractures[J]. Osteoporos Int, 2017, 28(5): 1531-1542. DOI:10.1007/s00198-017-3909-3 |
| [2] |
Zhao S, Xu CY, Zhu AR, et al. Comparison of the efficacy and safety of 3 treatments for patients with osteoporotic vertebral compression fractures:a network meta-analysis[J]. Medicine(Baltimore), 2017, 96(26): e7328. |
| [3] |
Wang F, Wang LF, Miao DC, et al. Which one is more effective for the treatment of very severe osteoporotic vertebral compression fractures:PVP or PKP?[J]. J Pain Res, 2018, 11: 2625-2631. DOI:10.2147/JPR.S179022 |
| [4] |
Wang H, Zhang Z, Liu Y, et al. Percutaneous kyphoplasty for the treatment of very severe osteoporotic vertebral compression fractures with spinal canal compromise[J]. J Orthop Surg Res, 2018, 13(1): 13. DOI:10.1186/s13018-018-0719-z |
| [5] |
宋鑫, 胥成平, 任东林, 等. 压力引导PKP治疗骨质疏松性椎体压缩骨折的临床疗效[J]. 脊柱外科杂志, 2020, 18(2): 82-87. |
| [6] |
Kim HS, Kim SW, Ju CI. Balloon kyphoplasty through extrapedicular approach in the treatment of middle thoracic osteoporotic compression fracture:T5-T8 level[J]. J Korean Neurosurg Soc, 2007, 42(5): 363-366. DOI:10.3340/jkns.2007.42.5.363 |
| [7] |
姚珍松, 叶林强, 江晓兵, 等. PVP治疗中上段胸椎骨质疏松性重度椎体压缩骨折的临床效果[J]. 中国脊柱脊髓杂志, 2014, 24(2): 138-143. |
| [8] |
Seong JY, Kim JS, Jung B, et al. CT-guided percutaneous vertebroplasty in the treatment of an upper thoracic compression fracture[J]. Korean J Radiol, 2009, 10(2): 185-189. DOI:10.3348/kjr.2009.10.2.185 |
| [9] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [10] |
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271-273. |
| [11] |
韩华, 项燕, 韩佳栩, 等. 不同国家人群胸椎椎弓根解剖结构的对比研究[J]. 中国临床解剖学杂志, 2018, 36(3): 252-258. |
| [12] |
Bayley E, Clamp J, Boszczyk BM. Percutaneous approach to the upper thoracic spine:optimal patient positioning[J]. Eur Spine J, 2009, 18(12): 1986-1988. |
| [13] |
Liu J, Tang J, Zhang Y, et al. Percutaneous vertebral augmentation for osteoporotic vertebral compression fracture in the midthoracic vertebrae(T5-8):a retrospective study of 101 Patients with 111 fractured segments[J]. World Neurosurg, 2019, 122: e1381-e1387. DOI:10.1016/j.wneu.2018.11.062 |
| [14] |
梁道臣, 李青, 张爱明, 等. CT引导下经椎弓根椎体成形术治疗老年骨质疏松性上位胸椎椎体压缩性骨折[J]. 深圳中西医结合杂志, 2016, 26(14): 93-95. |
| [15] |
赵兵德, 赵帅, 张文彬, 等. 单侧经肋-椎弓根入路椎体成形术在中上胸椎压缩性骨折中的应用[J]. 中国临床研究, 2017, 30(6): 756-760. |
 2020, Vol.18
2020, Vol.18  Issue(5): 300-304
Issue(5): 300-304


