巨大型腰椎椎间盘突出症(LDH)是指突出椎间盘组织超过腰椎椎管矢状径50%,临床多见,部分病例起病较急,多伴有下肢神经症状,少数患者可伴有马尾神经损伤[1-3]。对于巨大型LDH,除少数非手术治疗的报道[4]外,多建议手术治疗[1-3, 5],对于合并马尾神经损伤者需尽早手术[1-3]。单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术疗效确切,近年来在临床上得到较多应用。该手术方式早期多采用正中切口,具有上手快、视野大、操作方便等优势,但存在明显的骶棘肌损伤,而肌间隙入路的引入为骶棘肌的保护提供了很好的方式[6-8]。虽然肌间隙入路内固定融合术获得了广泛应用,但是微创通道下肌间隙入路单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术治疗巨大型LDH是否可行,是否会增加并发症的发生,特别是神经损伤的风险,目前尚未见报道。本研究回顾性分析2012年6月—2017年12月采用正中切口和微创通道下肌间隙入路单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术治疗且获得1年或以上随访的47例巨大型LDH患者资料,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①单节段巨大型LDH(突出椎间盘组织超过腰椎椎管矢状径50%);②合并马尾神经损伤或神经根损伤进行性加重需及时手术治疗,或经严格非手术治疗3~6个月效果不佳;③资料完整且获得1年或以上随访。排除标准:①病变节段椎弓根或椎板发育不良;②病变节段椎弓根峡部断裂;③合并骨质疏松;④体质量指数(BMI) > 25 kg/m2;⑤腰椎存在严重的三维畸形;⑥既往有腰椎后路手术史。根据上述标准,共纳入47例患者,均采用单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术治疗,其中采用正中切口入路22例(正中切口组),采用微创通道下肌间隙入路25例(肌间隙组)。所有患者均有腰痛病史,伴一侧下肢放射痛4例、伴双下肢放射痛38例、伴马尾神经损伤5例。入院后常规行腰椎正侧位和过屈过伸位(伴马尾神经损伤者除外)X线、CT及MRI检查,测量拟固定节段椎板关节突钉道长度、椎板厚度、椎板外斜角、椎板下倾角等参数[9]作为手术中操作参考。2组患者术前一般资料差异均无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 2组患者术前一般资料 Tab. 1 General data of 2 groups before operation |
手术由同一组医师完成。均采用静脉复合麻醉,患者采用俯卧位,腹部悬空。
正中切口组:以病变节段为中心点,经棘突做腰部正中纵行切口,依次切开,剥离一侧(有神经症状侧或病变严重侧)骶棘肌,使用自行设计的组配型横突拉钩(专利号:ZL 2013 2 0442436.7)[10]牵开骶棘肌。使椎板间隙及关节突关节获得良好显露,C形臂X线机透视确定病变节段。于病变节段上、下椎体经椎弓根置入定位针,采用标准的经椎间孔腰椎椎间融合术(TLIF)进行椎管扩大减压、髓核摘除,进行椎间隙深部植骨和融合器置入。在自行设计瞄准器(专利号ZL 2009 2 0120264.5)[11]引导下置入对侧椎板关节突螺钉,具体操作方法见文献[12-13]。最后取出定位针,置入椎弓根螺钉并安装连接棒,椎间作适当压缩。
肌间隙组:于神经根症状侧或病变严重侧以病变节段为中心,棘突旁开2~3 cm做腰部纵行切口,依次切开至腰背筋膜,经多裂肌肌纤维间作钝性分离,达椎板和关节突表面,顺序插入扩张套管,逐级扩张,置入带光源通道(Mispine系统,威高,中国山东)并纵向撑开,使通道底部呈喇叭状张开,将通道保持外倾并头倾方向固定。进一步清除椎板、关节突表面残余软组织,充分显露椎板间隙及关节突关节。采用C形臂X线机透视确定病变节段,其余操作同正中切口组。
椎弓根和椎板关节突螺钉置入均在C形臂X线机透视下完成,手术完成后切口内彻底止血,用大量生理盐水冲洗后依次缝合切口,切口内放置负压引流管1根。
钛合金空心椎板关节突螺钉(浦卫,中国上海)47例;钛合金椎弓根螺钉(威高,中国山东)42例,钛合金椎弓根螺钉(宝楠,中国台湾)5例;解剖型PEEK融合器(富乐,中国北京)16例(5例患者自一侧置入2枚融合器),香焦型PEEK融合器(Sofamor Danek,美国)31例。融合器内植骨采用关节突切除和椎管减压所获自体骨,椎间隙深部植骨材料来自自体骨7例、自体骨联合异种异体骨(金世植骨灵,中津,中国天津)9例、自体骨联合同种异体骨(鑫康辰,中国北京)16例、自体骨联合人工骨(骨肽,瑞邦,中国上海)15例。
1.3 术后处理术后常规预防性抗感染、胃黏膜保护、小剂量糖皮质激素等处理,并嘱患者卧床休息。麻醉苏醒后即嘱患者进行踝关节主动背伸运动,并进行双下肢直腿抬高的被动运动。切口引流管根据引流量(24 h引流量 < 50 mL)于术后48~72 h拔除。术后3~5 d佩戴腰围下床活动,术后6周进行腰背肌、腹肌功能锻炼。
1.4 观察和评价指标记录2组手术时间、术中出血量、术后引流量和切口长度。术后72 h采用视觉模拟量表(VAS)评分[14]评价腰部切口疼痛程度。采用日本骨科学会(JOA)评分(29分法)[15]评估术前和末次随访腰椎功能。观察术中及术后并发症发生情况:术中终板损伤、椎弓根骨折、硬膜损伤;术中和术后神经损伤。观察术后切口愈合情况,有无感染。
分别于术后3~5 d、3个月、6个月、12个月,随后每隔12个月行腰椎正侧位X线检查,于术后12个月行腰椎过屈过伸位X线检查;术后3~5 d行腰椎CT平扫,术后12个月行腰椎CT平扫并进行冠状面、矢状面重建;于术后12个月选取正中切口组17例、肌间隙组19例行腰椎MRI检查。记录并对比术前、术后12个月多裂肌面积与等级变化,术前、术后3~5 d和末次随访时病变节段椎间隙高度,术前和末次随访时腰椎冠状面和矢状面Cobb角;观察并评价螺钉位置、椎间融合情况。
多裂肌面积利用宁波明天医学影像系统不规则面积测量模块实时在线测量。多裂肌等级(MRI T2加权像上多裂肌脂肪组织沉积)采用Goutallier等[16]的标准:1级,正常肌肉;2级,脂肪组织散在分布于肌纤维间;3级,脂肪组织与肌肉组织所占比例大致相等;4级,脂肪组织占比超过肌肉组织。
按Xu等[17]提出的标准评价椎弓根螺钉位置:Ⅰ度,螺钉位于椎弓根内;Ⅱ度,穿出椎弓根部分螺钉直径 < 50%;Ⅲ度,穿出椎弓根部分螺钉直径≥50%。椎板关节突螺钉位置评价:Ⅰ型,螺钉位于椎板骨质内;Ⅱ型,螺钉部分穿透椎板;Ⅲ型,螺钉完全穿透椎板(螺钉位于椎板表面或完全进入椎管)。其中Ⅱ、Ⅲ度椎弓根螺钉和Ⅱ、Ⅲ型椎板关节突螺钉为位置不良螺钉。
椎间融合判断标准:①椎间融合器无移位,融合器内无透亮线;②椎间融合器前方有骨小梁通过;③融合器与椎体终板间无透亮线并有骨小梁通过;④过屈过伸位X线片示融合节段椎体无相对移位及终板角度变化 < 5°。符合①、②、④或者①、③、④项认为椎间融合良好。同时观察内固定有无松动、断裂,融合器有无位移。
1.5 统计学处理采用SPSS 20.0软件对数据进行统计学分析。计量资料以x±s表示,对术前、术后3~5 d和末次随访时的病变节段椎间隙高度变化进行方差分析,对术前和末次随访时腰椎冠状面和矢状面Cobb角、JOA评分,以及术前和术后12个月多裂肌面积比较采用配对t检验;计数资料以例数和百分数表示,并发症发生率比较采用χ2检验,术前和术后12个月多裂肌等级比较采用Wilcoxon符号秩检验;以P < 0.05为差异有统计学意义。
2 结果所有手术均顺利完成,均无切口感染,2组患者手术时间差异无统计学意义(P > 0.05,表 2)。所有患者随访12~48(26.50±7.45)个月。与正中切口组相比,肌间隙组切口较短、术中出血量较少、术后切口引流量较少、术后72 h腰部切口疼痛VAS评分较低,差异均有统计学意义(P < 0.05,表 2)。末次随访时2组JOA评分均较术前明显改善,差异均有统计学意义(P < 0.05,表 2);组间比较差异无统计学意义(P > 0.05,表 2)。
|
|
表 2 2组患者统计数据 Tab. 2 Statistical data of 2 groups |
椎弓根螺钉位置:正中切口组Ⅰ度41枚、Ⅱ度3枚,螺钉位置不良率为6.8%;肌间隙组Ⅰ度45枚、Ⅱ度5枚,螺钉位置不良率为10.0%;组间比较差异无统计学意义(P > 0.05)。椎板关节突螺钉位置:正中切口组Ⅰ型19枚、Ⅱ型3枚,螺钉位置不良率为13.6%;肌间隙组Ⅰ型20枚、Ⅱ型4枚、Ⅲ型1枚,螺钉位置不良率为20.0%;肌间隙组椎板关节突螺钉位置不良率高于正中切口组,差异有统计学意义(P < 0.05)。
2组患者术后椎间隙高度较术前明显恢复,但末次随访时较术后3~5 d出现丢失,差异均有统计学意义(P < 0.05,表 2);2组间各时间点比较差异均无统计学意义(P > 0.05,表 2)。末次随访时2组患者腰椎冠状面和矢状面平衡获得改善,与术前比较差异均有统计学意义(P < 0.05,表 2);2组间比较差异均无统计学意义(P > 0.05,表 2)。2组术前多裂肌面积和等级差异无统计学意义(P > 0.05,表 3);肌间隙组术后12个月多裂肌面积和等级与术前比较,差异均无统计学意义(P > 0.05,表 3),而正中切口组术后12个月多裂肌面积和等级与术前比较,差异均有统计学意义(P < 0.05,表 3);肌间隙组术后12个月多裂肌面积和等级均优于正中切口组,差异有统计学意义(P < 0.05,表 3)。
|
|
表 3 2组行MRI检查患者多裂肌面积及等级 Tab. 3 Multifidus area and grade of patients underwent MRI in 2 groups |
术中肌间隙组发生硬膜损伤并脑脊液漏1例、椎弓根骨折1例、终板损伤1例;正中切口组发生椎弓根骨折1例、终板损伤2例。术后肌间隙组发生切口皮肤局部坏死1例、马尾神经损伤1例,马尾神经损伤原因考虑为椎板关节突螺钉进入椎管所致,经行椎板关节突螺钉取出术。肌间隙组并发症发生率(20.0%,5/25)高于正中切口组(13.6%,3/22),差异有统计学意义(P < 0.05)。
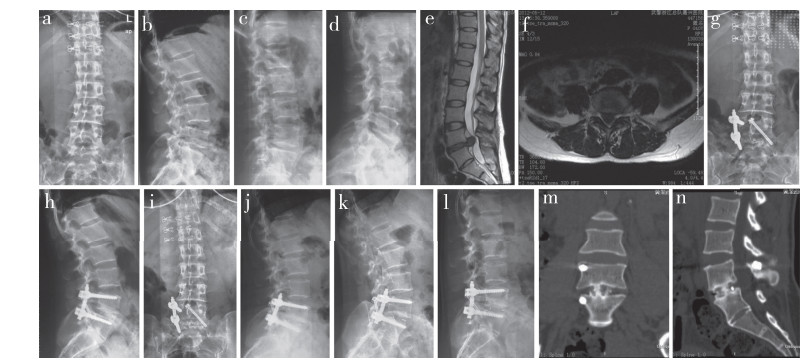
随访中观察到6例(正中切口组3例,肌间隙组3例)融合器切割终板部分陷入椎体内,未影响植骨融合。随访中未发现椎弓根螺钉与椎板关节突螺钉松动、移位、断裂或融合器前后移位等现象。除3例(正中切口组1例,肌间隙组2例)不能明确(椎间融合器内骨质稀疏,同时可见透亮线),其余患者均获得椎间融合,其中正中切口组融合率95.5%(21/22),肌间隙组融合率为92.0%(23/25),差异无统计学意义(P > 0.05)。2组均未观察到固定部位邻近节段发生明显退行性变(如椎间盘突出、椎间隙高度下降、骨质增生或局部畸形),而在椎板关节突螺钉固定侧的关节突出现程度不等的骨融合现象。2组典型病例影像学资料见图 1、2。
|
女,40岁,L4/L5巨大型LDH a、b:术前正侧位X线片示L4/L5椎间隙高度下降 c、d:术前过屈过伸位X线片示L4/L5终板角度无明显变化,椎体无相对位移 e、f:术前MRI示L4/L5椎间盘巨大突出,硬膜明显受压 g、h:术后3 d正侧位X线片示L4/L5椎间隙高度恢复,内固定位置良好 i、j:术后12个月正侧位X线片示L4/L5椎间隙高度有部分丢失,内固定位置良好 k、l:术后12个月过屈过伸位X线片示L4/L5终板角度无明显变化,椎体无相对位移 m、n:术后12个月CT示L4/L5椎间融合良好 Female, 40 years old, L4/L5 giant LDH a, b: Preoperative anteroposterior and lateral roentgenographs show L4/L5 intervertebral height decreases c, d: Preoperative hyperextension and hyperflexion roentgenographs show no significant change in L4/L5 endplate angle, and no relative displacement of L4 and L5 vertebral body e, f: Preoperative MRIs show L4/L5 giant lumbar disc herniation with significant dural compression g, h: Anteroposterior and lateral roentgenographs at postoperative 3 d show L4/L5 intervertebral height partly recovers and internal fixators are in good position i, j: Anteroposterior and lateral roentgenographs at postoperative 12 months show L4/L5 intervertebral height is partly lost, and internal fixators are in good position k, l: Hyperextension and hyperflexion roentgenographs at postoperative 12 months show no significant change in L4/L5 endplate angle and no relative displacement of L4 and L5 vertebral body m, n: CTs at postoperative 12 months show good interbody fusion of L4/L5 图 1 正中切口组典型病例影像学资料 Fig. 1 Imaging data of a typical case in median incision group |

|
男,42岁,L3/L4巨大型LDH a、b:术前正侧位X线片示L3/L4椎间隙高度下降 c、d:术前过屈过伸位X线片示L3/L4终板角度轻度变化,椎体无相对位移 e、f:术前MRI示L3/L4椎间盘巨大突出,硬膜明显受压 g、h:术后4 d正侧位X线片示L3/L4椎间隙高度部分恢复,内固定位置良好 i、j:术后12个月正侧位X线片示L3/L4椎间隙高度部分丢失,内固定位置良好 k、l:术后12个月过屈过伸位X线片示L3/L4终板角度无变化,无相对位移 m、n:术后12个月CT示L3/L4椎间融合良好 Male, 42 years old, L3/L4 giant LDH a, b: Preoperative anteroposterior and lateral roentgenographs show L3/L4 intervertebral height decreases c, d: Preoperative hyperextension and hyperflexion roentgenographs show slight change in L3/L4 endplate angle, and no relative displacement of L3 and L4 vertebral body e, f: Preoperative MRIs show L3/L4 giant lumbar disc herniation with significant dural compression g, h: Anteroposterior and lateral roentgenographs at postoperative 4 d show L3/L4 intervertebral height partly recovers and internal fixators are in good position i, j: Anteroposterior and lateral roentgenographs at postoperative 12 months show L3/L4 intervertebral height is partly lost, and internal fixators are in good position k, l: Hyperextension and hyperflexion roentgenographs at postoperative 12 months show no significant change in L3/L4 endplate angle and no relative displacement of L3 and L4 vertebral body m, n: CTs at postoperative 12 months show good interbody fusion of L3/L4 图 2 肌间隙组典型病例影像学资料 Fig. 2 Imaging data of a typical case in intermuscular group |
巨大型LDH具有特殊的病理形态和病情:①大块髓核脱出,多合并终板软骨剥脱;②椎间隙高度明显下降;③硬膜和神经根严重受压,脱出髓核与硬膜或神经根之间可能存在粘连;④病情进展较快,大部分患者伴有下肢神经症状,少部分合并马尾神经损伤;⑤由于髓核突出或脱出严重,硬膜、马尾神经、神经根受压明显,椎管内操作空间减少,神经退让余地少,手术治疗存在加重神经损伤的风险[18]。由于巨大型LDH具有上述病理改变和病情特点,手术治疗方式存在争议[1-3, 5, 19],但更多的文献建议行内固定融合术[1-3, 5]。单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术已广泛应用于治疗腰椎病变,但巨大型LDH能否采用微创通道下肌间隙入路尚不明确。
本研究中2组患者采用的内固定、减压、融合方式完全一致,术后椎间隙高度较术前均获得明显恢复,但在随访中均有不同程度丢失,末次随访时2组患者腰椎冠状面和矢状面平衡获得较好恢复,椎间融合良好,JOA评分改善明显,腰椎功能恢复良好,随访过程中均未出现内固定松动或断裂、融合器移位等现象。上述指标组间差异均无统计学意义,说明微创通道下肌间隙入路操作具有可行性,与正中切口入路相比,具有切口小、创伤小、出血量少、恢复快等优势。分析其原因:①通过多裂肌肌纤维间进入,肌肉剥离少;②通道顺肌纤维方向撑开,呈喇叭样张口,口小底大,可以实现较小切口内的最大化显露;③视野恒定,通道自带光源,照明良好;④手术区域正好位于视野内,操作方便。2组的手术时间基本一致,说明肌间隙入路并未增加手术时间,且术后72 h腰部切口疼痛明显轻于正中切口组,术后12个月多裂肌面积及等级均优于正中切口组,证明通道下肌间隙入路操作对多裂肌的损伤较轻。
然而,本研究发现肌间隙入路操作并发症发生率较高,可能与肌间隙入路通道显露有关:①肌间隙入路通道采用全新的手术切口、入路、显露方式和操作空间,学习曲线陡峭[20-24],早期操作不熟练可能导致并发症发生率较高,主要为切口问题,如切口局部皮肤坏死、切口愈合不良等。另外,通道下操作可能增加硬膜或神经损伤[25-27]。②肌间隙入路显露棘突基底存在一定困难,因而影响椎板关节突螺钉进入点的准确判断,增加椎板关节突螺钉位置不良率。本研究中2组患者椎弓根螺钉位置不良率差异无统计学意义,而肌间隙组椎板关节突螺钉位置不良率高于正中切口组。椎板关节突穿刺或置钉不准,如进入椎管,可能损伤硬膜或马尾神经。③巨大型LDH病理形态和病情独特,而肌间隙入路是在一个新学习的、较小的空间内操作,增加了硬膜和神经损伤的风险。因而,除了椎弓根骨折和终板损伤,与正中切口组相比,肌间隙组还出现术中硬膜损伤并脑脊液漏1例、术后切口皮肤局部坏死1例、马尾神经损伤1例,均发生于该技术应用早期,提示通道下肌间隙入路操作学习曲线陡峭。
由于TLIF开放的骨性窗口不大,基于巨大型LDH特有的病理和病情,无论是采用正中切口入路还是微创通道下肌间隙入路,均应避免一进入椎管即行髓核摘除、取出,应先处理椎间隙,将椎间隙内髓核基本清除干净后再仔细分离突出于椎管的髓核,缓慢取出。如髓核较大,直接取出困难,则用神经剥离器将其推入空虚的椎间隙内再从侧方取出。为避免髓核残留,术中需仔细探查椎管,确保硬膜和神经根减压充分、松解彻底。对于微创通道下肌间隙入路,建议熟练掌握后再应用于巨大型LDH的手术治疗。另外,由于单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定的轴向载荷能力相对较弱,建议尽量使用面积较大的融合器,如香蕉型融合器或一侧置入2枚普通融合器,且型号方面宁大勿小,以增加接触面积和纤维环张力,提高椎间稳定性,促进骨性融合[28-31]。
综上所述,微创通道下肌间隙入路单侧椎弓根螺钉联合对侧椎板关节突螺钉内固定并椎间植骨融合术治疗巨大型LDH具有可行性,且临床效果良好,与正中切口入路相比具有切口小、创伤小、出血量少、恢复快等优势,但学习曲线陡峭,加之本病的特殊性,并发症发生率较高,早期应用要慎重,操作应特别小心。
| [1] |
Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation[J]. Spine(Phila Pa 1976), 2000, 25(3): 348-352. DOI:10.1097/00007632-200002010-00015 |
| [2] |
Barriga A, Villas C. Cauda equina syndrome due to giant disc herniation[J]. Rev Med Univ Navarra, 2002, 46(3): 33-35. |
| [3] |
Kapetanakis S, Chaniotakis C, Kazakos C, et al. Cauda equina syndrome due to lumbar disc herniation: a review of literature[J]. Folia Med(Plovdiv), 2017, 59(4): 377-386. |
| [4] |
Benson RT, Tavares SP, Robertson SC, et al. Conservatively treated massive prolapsed discs: a 7-year follow-up[J]. Ann R Coll Surg Engl, 2010, 92(2): 147-153. DOI:10.1308/003588410X12518836438840 |
| [5] |
Jhala A, Singh D, Mistry M. Minimally invasive transforaminal lumbar interbody fusion: results of 23 consecutive cases[J]. Indian J Orthop, 2014, 48(6): 562-567. DOI:10.4103/0019-5413.144217 |
| [6] |
Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion[J]. Spine(Phila Pa 1976), 2003, 28(15 Suppl): S26-S35. |
| [7] |
Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion(TLIF): technical feasibility and initial results[J]. J Spinal Disord Tech, 2005, 8 Suppl: S1-S6. |
| [8] |
Holly LT, Schwender JD, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications[J]. Neurosurg Focus, 2006, 20(3): E6. |
| [9] |
曾忠友, 江春宇, 宋永兴, 等. 下腰椎椎板、关节突的影像学测量与临床意义[J]. 中国临床解剖学杂志, 2009, 27(4): 420-422. |
| [10] |
曾忠友, 吴鹏, 宋国浩. 组配型横突拉钩的研制与临床应用[J]. 脊柱外科杂志, 2015, 13(1): 28-32. DOI:10.3969/j.issn.1672-2957.2015.01.007 |
| [11] |
曾忠友, 江春宇, 张建乔, 等. 腰椎椎板关节突螺钉瞄准器的研制[J]. 中国骨与关节损伤杂志, 2009, 24(8): 761-762. |
| [12] |
曾忠友, 严卫锋, 陈国军, 等. 单侧椎弓根螺钉联合对侧椎板关节突螺钉固定治疗下腰椎病变的临床观察[J]. 中华骨科杂志, 2011, 31(8): 834-839. DOI:10.3760/cma.j.issn.0253-2352.2011.08.003 |
| [13] |
Zeng ZY, Wu P, Yan WF, et al. Mixed fixation and interbody fusion for treatment single-segment lower lumbar vertebral disease: midterm follow-up results[J]. Orthop Surg, 2015, 7(4): 324-332. DOI:10.1111/os.12214 |
| [14] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [15] |
Fukui M, Chiba K, Kawakami M, et al. Japanese Orthopaedic Association back pain evaluation questionnaire. Part 2. Verification of its reliability: the subcommittee on low back pain and cervical myelopathy evaluation of the clinical outcome committee of the Japanese Orthopaedic Association[J]. J Orthop Sci, 2007, 12(6): 526-532. DOI:10.1007/s00776-007-1168-4 |
| [16] |
Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan[J]. Clin Orthop Relat Res, 1994(304): 78-83. |
| [17] |
Xu R, Ebraheim NA, Ou Y, et al. Anatomic considerations of pedicle screw placement in the thoracic spine. Roy-Camille technique versus open-lamina technique[J]. Spine(Phila Pa 1976), 1998, 23(9): 1065-1068. DOI:10.1097/00007632-199805010-00021 |
| [18] |
Henriques T, Olerud C, Petrén-Mallmin M, et al. Cauda equina syndrome as a postoperative complication in five patients operated for lumbar disc herniation[J]. Spine(Phila Pa 1976), 2001, 26(3): 293-297. DOI:10.1097/00007632-200102010-00015 |
| [19] |
Li X, Dou Q, Hu S, et al. Treatment of cauda equina syndrome caused by lumbar disc herniation with percutaneous endoscopic lumbar discectomy[J]. Acta Neurol Belg, 2016, 116(2): 185-190. DOI:10.1007/s13760-015-0530-0 |
| [20] |
Villavicencio AT, Burneikiene S, Roeca CM, et al. Minimally invasive versus open transforaminal lumbar interbody fusion[J]. Surg Neurol Int, 2010, 1: 12. DOI:10.4103/2152-7806.63905 |
| [21] |
Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases[J]. Spine(Phila Pa 1976), 2012, 37(18): 1548-1557. DOI:10.1097/BRS.0b013e318252d44b |
| [22] |
Silva PS, Pereira P, Monteiro P, et al. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion[J]. Neurosurg Focus, 2013, 35(2): E7. DOI:10.3171/2013.5.FOCUS13157 |
| [23] |
Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review[J]. Clin Orthop Relat Res, 2014, 472(6): 1711-1717. DOI:10.1007/s11999-014-3495-z |
| [24] |
Lee KH, Yeo W, Soeharno H, et al. Learning curve of a complex surgical technique: minimally invasive transforaminal lumbar interbody fusion(MIS TLIF)[J]. J Spinal Disord Tech, 2014, 27(7): E234-E240. DOI:10.1097/BSD.0000000000000089 |
| [25] |
曾忠友, 宋永兴, 吴鹏, 等. 通道下肌间隙入路椎间融合术治疗腰椎病变的近期疗效[J]. 中华骨科杂志, 2015, 35(12): 1191-1199. DOI:10.3760/cma.j.issn.0253-2352.2015.12.003 |
| [26] |
曾忠友, 宋永兴, 吴鹏, 等. 通道下联合固定并椎间融合术治疗腰椎病变的早期并发症[J]. 中国矫形外科杂志, 2016, 24(17): 1537-1544. |
| [27] |
曾忠友, 宋永兴, 严卫锋, 等. 通道下肌间隙入路腰椎固定融合术并发神经损伤的原因及预防[J]. 脊柱外科杂志, 2017, 15(4): 211-216. DOI:10.3969/j.issn.1672-2957.2017.04.004 |
| [28] |
Lee JH, Jeon DW, Lee SJ, et al. Fusion rates and subsidence of morselized local bone grafted in titanium cages in posterior lumbar interbody fusion using quantitative three-dimensional computed tomography scans[J]. Spine(Phila Pa 1976), 2010, 35(15): 1460-1465. DOI:10.1097/BRS.0b013e3181c4baf5 |
| [29] |
Lee JH, Lee JH, Park JW, et al. Fusion rates of a morselized local bone graft in polyetheretherketone cages in posterior lumbar interbody fusion by quantitative analysis using consecutive three-dimensional computed tomography scans[J]. Spine J, 2011, 11(7): 647-653. DOI:10.1016/j.spinee.2011.04.029 |
| [30] |
Tassemeier T, Haversath M, Jäger M. Transforaminal lumbar interbody fusion with expandable cages: radiological and clinical results of banana-shaped and straight implants[J]. J Craniovertebr Junction Spine, 2018, 9(3): 196-201. DOI:10.4103/jcvjs.JCVJS_56_18 |
| [31] |
王正安, 曾忠友, 张建乔, 等. 通道下联合固定并椎间不同融合器植骨治疗腰椎疾患的病例对照研究[J]. 中国骨伤, 2020, 33(4): 337-347. |
 2021, Vol.19
2021, Vol.19  Issue(1): 26-33
Issue(1): 26-33

