胸腰椎骨折是临床常见的脊柱损伤,多由于高能量垂直暴力致使椎体发生爆裂性骨折,脊柱稳定性遭受破坏,需要外科干预[1]。临床上常采用后路椎弓根螺钉内固定术治疗胸腰椎爆裂性骨折,术后早期疗效确切,但骨折可造成不同程度的骨量丢失,易出现骨折不愈合、椎体高度丢失、进展性后凸畸形、顽固性腰背疼痛,甚至发生内固定断裂等严重后果[1-2]。近年来,随着脊柱外科技术和微创理念的日臻完善和发展,人们对胸腰椎骨折的认识逐步深入,Denis[3]提出了三柱理论,并发展出脊柱载荷评分(LSS)系统、胸腰椎损伤分类与严重程度评分(TLICS)、AO分型等多种临床评分和分型系统,这对胸腰椎骨折的临床诊治提供了有意义的指导[4-6]。然而,胸腰椎爆裂性骨折的手术治疗在手术适应证、手术方式及手术入路的选择等方面仍存在诸多争议[7]。本研究回顾性分析了126例胸腰椎爆裂性骨折患者临床资料,比较改良Wiltse入路经伤椎椎弓根植骨内固定术与常规后路内固定术治疗的效果,探讨改良Wiltse入路经伤椎椎弓根植骨内固定术治疗胸腰椎爆裂性骨折的临床价值。
1 资料与方法 1.1 临床资料回顾性分析2015年1月—2018年12月收治的126例胸腰椎爆裂性骨折患者的临床资料,其中64例采用改良Wiltse入路经伤椎椎弓根植骨内固定术治疗(观察组),62例采用常规后路内固定术治疗(对照组)。所有患者入院后均常规进行X线、CT三维重建及MRI检查。所有患者术前LSS评分[4]为5~6分,TLICS评分[5]为4~5分,美国脊髓损伤协会(ASIA)分级[8]均为E级。观察组患者64例,其中男45例、女19例,年龄19~63(38.7±11.6)岁,受伤至入院时间5~125(6.6±25.4)h;高处坠落伤31例,车祸伤15例,重物砸伤13例,其他外伤5例;受伤部位T11 6例,T12 18例,L1 24例,L2 9例,L3 3例,T11,12 1例,T12~L1 2例,L1,2 1例。对照组62例,其中男41例、女21例,年龄20~64(39.1±11.9)岁,受伤至入院时间6~127(6.8±25.2)h;高处坠落伤30例,车祸伤17例,重物砸伤12例,其他外伤3例;受伤部位T11 5例,T12 19例,L1 20例,L2 5例,L3 5例,T11,12 3例,T12~L1 4例,L1,2 1例。
1.2 手术方法患者采用气管插管全身麻醉,取俯卧位,保持腹部悬空,术中采用C形臂X线机透视定位。观察组以伤椎棘突为中心做后正中纵行切口,切开皮肤及皮下组织,沿深筋膜表面向两侧锐性分离2.5~3.0 cm,纵行切开深筋膜,双侧钝性分离最长肌与多裂肌间隙,充分显露伤椎及相邻椎体椎弓根投影点,分别置入椎弓根螺钉,调整体位撑开复位骨折椎体后,使用自制的植骨器械经骨折椎体单侧或双侧椎弓根植入人工骨颗粒(4.8 mm×2.8 mm,5 mL;Wright公司,美国),单个椎体植入量通常为3~5 mL,安装连接棒、锁紧螺母。对照组取后正中切口,沿棘突、椎板两侧剥离显露椎弓根投影点,分别置入椎弓根螺钉,复位骨折椎体后安装连接棒、锁紧螺母。
1.3 评价方法患者常规行胸腰椎正侧位X线检查,门诊定期随访复查。记录2组手术时间、术中出血量并进行比较。统计2组术前、术后1个月及末次随访时椎体高度丢失率、脊柱矢状面Cobb角,以及疼痛视觉模拟量表(VAS)评分[9]、Oswestry功能障碍指数(ODI)[10],评价疗效及预后。伤椎高度丢失率(%)=[1-2×伤椎高度/(近端椎高度+远端椎高度)]×100%。测量方法见图 1[11]。
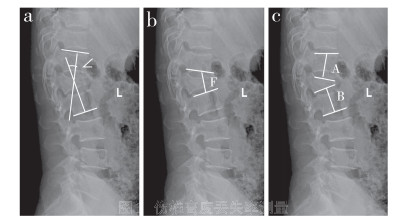
|
a:矢状位Cobb角(∠),近端椎上终板垂线与远端椎下终板垂线间的夹角 b:伤椎高度(F) c:近端椎高度(A)和远端椎高度(B),各椎高度均包括椎体高度和上下椎间盘高度 a: Sagittal Cobb's angle(∠), angle between vertical line of proximal superior vertebral endplate and distal inferior endplate b: Height of injured vertebra(F) c: Height of proximal vertebra(A) and distal vertebra(B). Height of each vertebra includes height of vertebral body and height of upper and lower intervertebral discs 图 1 伤椎高度丢失率测量 Fig. 1 Measurement of height loss rate of injured vertebral body |
采用SPSS 20.0软件对数据进行统计学分析。计量资料以x±s表示,组间比较采用独立样本t检验;以P < 0.05为差异有统计学意义。
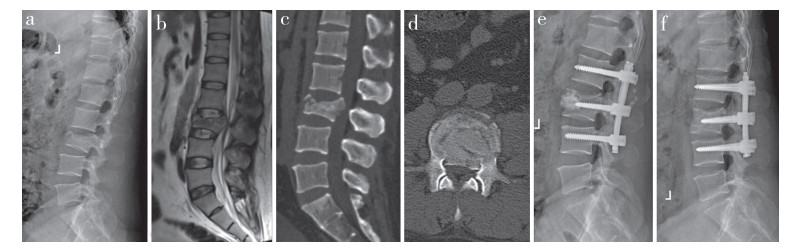
2 结果所有患者随访10~36(18.0±8.0)个月,手术时间、术后1个月椎体高度丢失率、术后1个月脊柱矢状面Cobb角组间比较差异均无统计学意义(P > 0.05,表 1);观察组术中出血量、术后1个月VAS评分均低于对照组,差异有统计学意义(P < 0.05,表 1)。末次随访时,观察组椎体高度丢失率、脊柱矢状面Cobb角、VAS评分和ODI均低于对照组,差异有统计学意义(P < 0.05,表 1)。典型病例影像学资料见图 2。
|
|
表 1 2组手术情况和术后疗效 Tab. 1 Operation situation and postoperative outcomes of 2 groups |
|
a:术前侧位X线片示L3骨折 b:术前矢状位MRI示椎管狭窄 c:术前矢状位CT示椎体爆裂性骨折 d:术前冠状位CT示骨块突入椎管 e:术后3 d侧位X线片示经椎弓根植骨、骨折复位 f:术后12个月侧位X线片示骨折愈合、椎体高度良好 a: Preoperative lateral roentgenograph shows L3 fracture b: Preoperative sagittal MRI shows spinal stenosis c: Preoperative sagittal CT shows burst fracture d: Preoperative coronal CT shows bone block protruding into vertebral canal e: Lateral roentgenograph at postoperative 3 d shows bone grafting through pedicle and fracture reduction f: Lateral roentgenograph at postoperative 12 months shows fracture healing and good vertebral height 图 2 观察组典型病例影像学资料 Fig. 2 Imaging data of a typical case in observation group |
胸腰椎爆裂性骨折往往由高处坠落伤、交通事故伤、重物砸伤等引起,多数症状严重,需要手术治疗[12]。传统的胸腰椎后路内固定术疗效确切,但手术需要剥离两侧椎旁肌,创伤较大,出血量较多,手术操作时间较长[13]。近年,随着脊柱外科微创理念及技术的发展,经皮置钉或通道置钉技术逐步应用于临床,但该类技术需要特殊设备辅助,操作过程中医患均要遭受一定剂量的辐射暴露,手术医师也需要经历一定的成长曲线,初期应用手术操作时间较长,对椎旁肌也会造成不同程度的损伤[14]。本研究观察组采用改良Wiltse入路经伤椎椎弓根植骨内固定术,其符合现代脊柱微创的理念,手术操作简单,能够避免传统后正中入路显露时对椎旁肌肉的剥离及失神经支配等问题,且出血量显著减少。而且,因手术从肌间隙进入,术后肌肉不易发生瘢痕化,最大限度地保留了椎旁软组织的功能,降低了术后腰背部疼痛的发生率[15]。
胸腰椎爆裂性骨折常规后路内固定术后常见的并发症为椎体高度丢失、内固定失效、假关节形成、继发性后凸畸形,最终产生严重胸背部疼痛,甚至出现脊髓神经损伤等严重后果[1-2]。引起上述并发症的主要原因可能是爆裂的椎体经椎弓根螺钉系统撑开后,椎体高度虽然获得恢复,但伤椎内松质骨因爆裂、塌陷而呈中空的“蛋壳样”结构,骨折椎体可发生延迟愈合或不愈合;如果患者年龄偏大、骨量减少或过早负重,则极易发生椎体高度丢失,甚至内固定失效,而导致严重后果。临床研究表明,经伤椎椎弓根向爆裂椎体的前中柱植骨可有效解决椎体中空现象,提供相对稳定的骨折椎体内部支撑,同时为骨折愈合提供良好的条件[16-17]。本研究观察组末次随访椎体高度丢失率、脊柱矢状面Cobb角、VAS评分及ODI均优于对照组,表明经伤椎椎弓根植骨能够为椎体提供有效的内部支撑,使骨折椎体获得长期稳定性,避免椎体高度丢失、继发性后凸及脊髓神经损伤等远期并发症的发生。
综上所述,改良Wiltse入路经伤椎椎弓根植骨内固定术治疗胸腰椎爆裂性骨折符合脊柱微创理念,手术创伤小、操作简单、出血量少,有利于患者早期快速康复;同时,经伤椎椎弓根植骨可有效解决复位后骨折椎体中空现象,促进骨折愈合,避免椎体高度丢失、假关节形成、继发性后凸以及脊髓神经损伤等远期并发症的发生。因此,改良Wiltse入路经伤椎椎弓根植骨内固定术治疗胸腰椎爆裂性骨折临床疗效满意,具有一定的推广价值。
| [1] |
Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture[J]. Asian Spine J, 2015, 9(1): 133-146. DOI:10.4184/asj.2015.9.1.133 |
| [2] |
刘小鹏, 颜春铭, 郭伟华, 等. 经伤椎椎弓根植骨联合椎弓根钉内固定系统治疗胸腰椎爆裂性骨折[J]. 脊柱外科杂志, 2018, 16(6): 340-343. DOI:10.3969/j.issn.1672-2957.2018.06.005 |
| [3] |
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries[J]. Spine(Phila Pa 1976), 1983, 8(8): 817-831. DOI:10.1097/00007632-198311000-00003 |
| [4] |
Holdsworth F. Fractures, dislocation, and fracture-disloctions of the spine[J]. J Bone Joint Surg Am, 1970, 52(15): 1534-1551. |
| [5] |
Vaccaro AR, Lehman RA Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status[J]. Spine (Phila Pa 1976), 2005, 30(20): 2325-2333. DOI:10.1097/01.brs.0000182986.43345.cb |
| [6] |
Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive of classification of thoracic and lumbar injuries[J]. Eur Spine J, 1994, 3(4): 184-201. DOI:10.1007/BF02221591 |
| [7] |
Kumar A, Aujla R, Lee C. The management of thoracolumbar burst fractures: a prospective study between conservative management, traditional open spinal surgery and minimally interventional spinal surgery[J]. Springerplus, 2015, 4: 204. DOI:10.1186/s40064-015-0960-4 |
| [8] |
American Spinal Injury Association. Standards for neurological classification of spinal injury patients[M]. Chicago: American Spinal Injury Association, 2011: 644-645.
|
| [9] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [10] |
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271-273. |
| [11] |
Haiyun Y, Rui G, Shucai D, et al. Three-column reconstruction through single posterior approach for the treatment of unstable thoracolumbar fracture[J]. Spine (Phila Pa 1976), 2010, 35(8): E295-E302. DOI:10.1097/BRS.0b013e3181c392b9 |
| [12] |
江伟伟, 裴蕾, 王胜云, 等. 胸腰椎爆裂性骨折: 从致伤因素看临床症状[J]. 第二军医大学学报, 2019, 40(8): 909-913. |
| [13] |
赵小灵, 潘飞龙, 刘志元, 等. 经皮椎弓根内固定术与后路切开复位椎弓根内固定术在治疗胸腰椎骨折的疗效比较[J]. 世界最新医学信息文摘, 2019, 19(82): 198, 203. |
| [14] |
李琳, 李峰, 陈华. 微创经皮与Wiltse入路椎弓根钉内固定治疗胸腰椎骨折的疗效比较[J]. 中国骨与关节损伤杂志, 2017, 32(1): 18-21. |
| [15] |
冯明星, 肖杰, 龙浩, 等. 肌间隙有限暴露结合椎板间减压治疗胸腰椎爆裂性骨折[J]. 脊柱外科杂志, 2018, 16(6): 363-367. DOI:10.3969/j.issn.1672-2957.2018.06.010 |
| [16] |
Van Herck B, Leirs G, Van Loon J. Transpedicular bone grafting as a supplement to posterior pedicle screw instrumentation in thoracolumbar burst fractures[J]. Acta Orthop Belg, 2009, 75(6): 815-821. |
| [17] |
Li Q, Yun C, Li S. Transpedicular bone grafting and pedicle screw fixation in injured vertebrae using a paraspinal approach for thoracolumbar fractures: a retrospective study[J]. J Orthop Surg Res, 2016, 11(1): 115. DOI:10.1186/s13018-016-0452-4 |
 2021, Vol.19
2021, Vol.19  Issue(1): 34-37
Issue(1): 34-37

