2. 中国医科大学附属第一医院骨科, 沈阳 110001
2. Department of Orthopaedics, First Affiliated Hospital of China Medical University, Shenyang 110001, Liaoning, China
颈椎椎间盘突出症(CDH)是中老年人常见疾病[1],颈椎前路手术目前是临床治疗颈椎病的最主要手术入路[2]。其中,前路颈椎椎间盘切除融合术(ACDF)因其融合率高及疗效好而被作为治疗颈椎病的金标准[3]。然而,融合后的节段很可能会降低颈椎的活动度(ROM),并加速相邻椎体的退行性变[4-5]。颈椎全椎间盘置换术(CTDR)可为颈椎保留良好的ROM,但其术后异位骨化和后凸畸形的发生率较高,故未能得到广泛应用[6-9]。颈椎动态装置植入术(DCI)是一种非融合技术,具有更广泛的适应证,同时与CTDR相比,其手术方式相对简单[10]。目前,越来越多的临床医师使用DCI替代CTDR。理论上,非融合手术相较于ACDF可保留更多ROM;但对于单节段CDH患者,有关上述2种术式对其颈椎ROM的影响如何,相关研究资料较少。为此,本研究回顾性分析了2018年6月—2019年9月海军军医大学长征医院收治的78例单节段CDH患者临床资料,并对其临床和影像学结果进行比较,同时分析患者手术前后的颈椎ROM变化,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①经影像学检查确诊为单节段CDH,且临床表现与病变节段相一致;②年龄25 ~ 70岁。排除标准:①合并后纵韧带骨化、肿瘤、感染、外伤或神经系统疾病;②既往有颈椎手术史;③颈椎结构不稳、重度骨质疏松等手术禁忌证。所有患者均适合采用ACDF和DCI治疗,术式选择由患者在完全了解2种手术的益处和风险后决定。根据以上标准,共纳入患者78例,其中42例采用ACDF治疗(ACDF组),36例采用DCI治疗(DCI组),2组患者术前一般资料比较,差异无统计学意义(P > 0.05,表 1),具有可比性。患者术前均签署知情同意书。
|
|
表 1 2组患者一般资料 Tab. 1 General data of patients in 2 groups |
所有手术均由同一位主任医师带领的团队完成。患者全身麻醉后取仰卧位,在肩背部垫小枕,颈部自然后伸,颈部术区常规消毒铺巾。在颈前部右侧沿皮纹做横切口,长约4.0 cm。依次切开皮肤、皮下组织,游离皮下间隙,纵行切开颈阔肌,剪开颈血管鞘与内脏鞘之间的联合筋膜,由二者之间钝性分离进入椎前间隙,将气管、食管向左侧牵开,剪开椎前筋膜,显露椎体及两侧椎间盘前部,X线透视下明确定位无误后,用Caspar撑开器撑开椎体,用尖刀切除病变节段的椎间盘前部纤维环,以髓核钳取出发生退行性变的髓核组织,继续刮除终板软骨,以枪状咬骨钳清除突入椎管的椎间盘组织、肥厚增生的后纵韧带及椎体后缘骨赘,以大量生理盐水冲洗创腔,确认受压的脊髓逐渐恢复正常形态。以三关节咬骨钳咬除椎体前缘骨赘,试模成功后取合适大小的置入物(有碎骨的融合器或动态装置)置入椎间隙。取出椎体撑开器,用骨蜡封闭钉孔(ACDF组取合适长度的钛板,预弯后固定于椎体前壁,拧入螺钉并锁定)。透视确认内置物位置良好后,再次使用大量生理盐水冲洗术区,仔细检查,确认无明显出血点后切口旁另切1个小口,引入1根负压引流管。逐层缝合联合腱膜、颈阔肌、皮下组织,以可吸收线缝合皮肤。确认负压引流通畅,无菌包扎创口。
术后2 d,雾化吸入1 mg/mL地塞米松磷酸钠注射液10 mL以缓解气管和食管不适。引流管于术后24 ~ 48 h取出。术后次日,患者可于颈托保护下下床活动,术后颈托佩戴10 d。
1.3 观察指标记录手术时间及术中出血量,术前及术后1年日本骨科学会(JOA)评分[11]、疼痛视觉模拟量表(VAS)[12]评分、手术节段Cobb角(手术节段上位椎体上终板与下位椎体下终板间的夹角)、C2~7颈椎曲度(C2下终板与C7下终板间的夹角)、邻近椎体高度(上位椎体上终板及下位椎体下终板间的垂直距离)及颈椎各运动方向(前屈后伸、左右侧曲、左右旋转)的ROM。按照新型头盔式颈椎ROM测量仪(Performance Attainments AssociatesTM,美国)操作指南,嘱被检者取端坐位,挺直上身,腰背部紧贴椅背,头戴颈椎ROM仪,提前适度活动颈椎以增加颈部肌肉顺应性,调整体位,确认冠状面及矢状面量角仪的初始读数归零,然后依次测量颈椎左右侧曲、左右旋转、前屈后伸ROM。整个过程中被检者应保持相同体位(图 1)。

|
a:左曲 b:右曲 c:左旋 d:右旋 e:前屈 f:后伸 a: Left lateral bending b: Right lateral bending c: Left rotation d: Right rotation e: Flexion f: Extension 图 1 颈椎ROM测量 Fig. 1 Measurement of cervical ROM |
使用SPSS 22.0软件对数据进行统计学分析。计量资料以x±s表示,手术前后比较采用配对样本t检验,2种术式间比较采用独立样本t检验,计数资料采用χ2检验;以P < 0.05为差异有统计学意义。
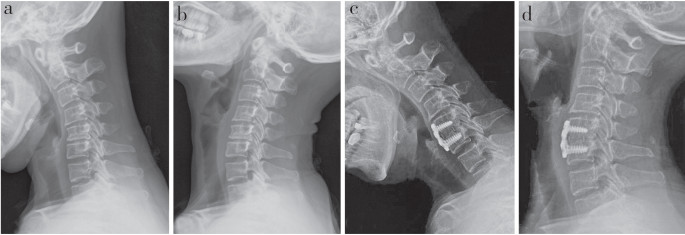
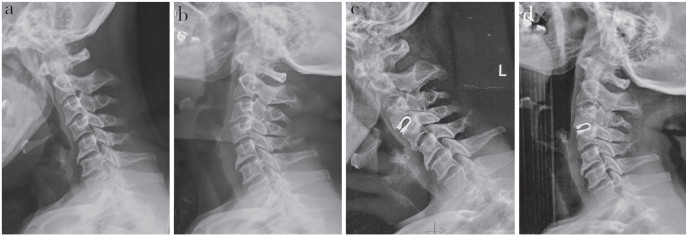
2 结果所有手术顺利完成,未发生死亡、感染、脊髓损伤或气管、食管损伤等并发症。2组术中出血量比较,差异无统计学意义(P > 0.05,表 2)。DCI组手术时间比ACDF组短,差异有统计学意义(P < 0.05,表 2)。所有患者随访超过1年。2组患者术后1年JOA评分、VAS评分和邻近椎体高度均较术前改善,差异有统计学意义(P < 0.05,表 2),但组间差异均无统计学意义(P > 0.05,表 2)。术后1年ACDF组C2~7颈椎曲度、手术节段Cobb角均较术前有所丢失,差异有统计学意义(P < 0.05,表 2);DCI组无明显丢失,与术前比较,差异无统计学意义(P > 0.05,表 2);组间比较,差异有统计学意义(P < 0.05,表 2)。术后1年2组前屈后伸、左右侧曲ROM与术前比较均未出现明显变化,差异无统计学意义(P > 0.05,表 2)。术后1年2组左右旋转ROM出现了相近程度的受限,与术前相比,差异有统计学意义(P < 0.05,表 2);组间比较,差异无统计学意义(P > 0.05,表 2)。典型病例影像学资料见图 2、3。
|
|
表 2 2组患者统计数据 Tab. 2 Statistical data of patients in 2 groups |
|
a、b:术前过伸过屈位X线片c、d:术后1年过伸过屈位X线片示术后手术节段Cobb角、C2~7颈椎曲度均有丢失 a, b: Preoperative flexion and extension roentgenographs c, d: Flexion and extension roentgenographs at postoperative 1 year show Cobb's angle of operation segment and C2-7 cervical curvature are lost 图 2 ACDF组典型病例影像学资料 Fig. 2 Imaging data of a typical case in ACDF group |
|
a、b:术前过伸过屈位X线片c、d:术后1年过伸过屈位X线片示术后手术节段Cobb角、C2~7颈椎曲度无明显丢失 a, b: Preoperative flexion and extension roentgenographs c, d: Flexion and extension roentgenographs at postoperative 1 year show Cobb's angle of operation segment and C2-7 cervical curvature has no significant loss 图 3 DCI组典型病例影像学资料 Fig. 3 Imaging data of a typical case in DCI group |
颈椎病是危害人类的常见病。当患者接受的常规非手术治疗失败或症状恶化时,常需要手术处理,而所有的手术治疗都是通过切除椎间盘来解除脊髓压迫。近年来常用的经典融合术和椎间盘置换术,对手术节段ROM的保留效果不同。1958年,Smith等[13]和Cloward[14]采用ACDF治疗椎间盘退行性变引起的颈椎病,取得了良好的临床效果,成为治疗颈椎病的典型术式。然而,正如在大量长期临床病例中发现的那样,ACDF存在一些术后并发症,如颈椎ROM降低和邻近节段椎间盘退行性变加速[15]。Hilibrand等[16]对374例采用ACDF治疗的患者进行了21年的随访,发现融合后邻近节段退行性变导致的临床症状在术后10年内平均发生率为2.9%。上述并发症的存在使可以维持手术节段ROM的颈椎关节置换术在临床上得到应用。CTDR能保持颈椎运动,降低相邻节段退行性变的发生率,在术后早中期有良好的临床效果[17-18]。然而,大量的随访发现,其术后后凸畸形和异位骨化的发生率很高[19-20]。CTDR的设计思想是模仿关节假体,但脊柱的多节段运动比髋关节和膝关节复杂,影响因素众多,假体植入对假体大小的选择、置换节段上下终板的处理、假体关节线高度、旋转轴、旋转中心位置等方面要求较高,文献报道其术中和术后并发症发生率高[21-22]。与髋关节和膝关节置换术不同,颈椎椎间盘置换术的研究还不够深入,不足以替代融合手术,仍需要进一步研究。DCI是颈椎非融合技术的又一尝试,它与颈椎椎间盘置换术类似,也是对恢复椎间盘高度和保持一定稳定性的某些特征和特点的模拟重建。动态装置的动态设计具有轴向顺应性和减震功能,有效避免了上下相邻节段退行性变加速。
颈椎ROM对于评价颈椎术后患者的生活质量及颈椎活动功能十分重要,是临床广为接受的评价指标。头盔式颈椎ROM测量仪设计完善,已广泛应用于临床研究[23-24],被认为是准确可靠的ROM测量工具。本研究采用颈椎ROM测量仪测得6个方向的颈椎ROM,综合讨论患者术后颈椎ROM的变化,发现2组术后颈椎前屈后伸、左右侧曲ROM均未出现明显的下降,而2组左右旋转ROM出现相近程度的受限,说明单节段颈椎前路手术,不管是否融合,对患者前屈后伸、左右侧曲活动的影响并不大,只有旋转活动会受到一定的限制。术后1年ACDF组C2~7颈椎曲度、手术节段Cobb角较术前有所丢失,DCI组则无明显丢失,说明从影像学角度,DCI对颈椎的屈伸功能影响相对更小。但本研究仍存在一定的局限性,本研究的观察对象为单节段颈椎前路手术患者,而多节段手术对颈椎ROM的影响仍未可知,本团队目前也在积极开展这项研究,希望在未来长期随访中得出结论。
综上,虽然影像学结果显示ACDF在保留颈椎ROM方面的表现不如DCI,但颈椎ROM测量仪测量结果表明,2种术式颈椎ROM的丢失有限。这也为临床手术方式的选择及患者颈椎活动能力的预后判断提供了参考。
| [1] |
贾连顺. 颈椎病的诊断学基础[J]. 脊柱外科杂志, 2004, 2(3): 187-189. DOI:10.3969/j.issn.1672-2957.2004.03.021 |
| [2] |
袁文. 对颈椎融合与非融合手术的再认识[J]. 中国脊柱脊髓杂志, 2012, 22(6): 481-482. DOI:10.3969/j.issn.1004-406X.2012.06.01 |
| [3] |
杨有庚, 任宪盛, 杨晨, 等. 剖析颈椎病外科治疗的策略提高颈椎病前路手术的疗效[J]. 脊柱外科杂志, 2009, 7(5): 260-262. DOI:10.3969/j.issn.1672-2957.2009.05.002 |
| [4] |
Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion[J]. Eur Spine J, 2001, 10(4): 314-319. DOI:10.1007/s005860000239 |
| [5] |
Wang X, Meng Y, Liu H, et al. Association of cervical sagittal alignment with adjacent segment degeneration and heterotopic ossification following cervical disc replacement with Prestige-LP disc[J]. J Orthop Surg(Hong Kong), 2020, 28(3): 2309499020968295. |
| [6] |
Parkinson JF, Sekhon LH. Cervical arthroplasty complicated by delayed spontaneous fusion. Case report[J]. J Neurosurg Spine, 2005, 2(3): 377-380. DOI:10.3171/spi.2005.2.3.0377 |
| [7] |
Leung C, Casey AT, Goffin A, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial[J]. Neurosurgery, 2005, 57(4): 759-762. DOI:10.1227/01.NEU.0000175856.31210.58 |
| [8] |
Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement[J]. Spine(Phila Pa 1976), 2006, 31(24): 2802-2806. DOI:10.1097/01.brs.0000245852.70594.d5 |
| [9] |
Heidecke V, Burkert W, Brucke M, et al. Intervertebral disc replacement for cervical degenerative disease-clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis[J]. Acta Neurochir(Wien), 2008, 150(5): 453-459. DOI:10.1007/s00701-008-1552-7 |
| [10] |
Li Z, Yu S, Zhao Y, et al. Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease[J]. J Clin Neurosci, 2014, 21(6): 942-948. DOI:10.1016/j.jocn.2013.09.007 |
| [11] |
Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890-1894. DOI:10.1097/00007632-200109010-00014 |
| [12] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [13] |
Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion[J]. J Bone Joint Surg Am, 1958, 40-A(3): 607-624. |
| [14] |
Cloward RB. The anterior approach for removal of ruptured cervical disks[J]. J Neurosurg, 1958, 15(6): 602-617. DOI:10.3171/jns.1958.15.6.0602 |
| [15] |
Sasso RC, Best NM. Cervical kinematics after fusion and Bryan disc arthroplasty[J]. J Spinal Disord Tech, 2008, 21(1): 19-22. DOI:10.1097/BSD.0b013e3180500778 |
| [16] |
Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis[J]. J Bone Joint Surg Am, 1999, 81(4): 519-528. DOI:10.2106/00004623-199904000-00009 |
| [17] |
Yang S, Wu X, Hu Y, et al. Early and intermediate follow-up results after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: single- and multiple-level[J]. Spine(Phila Pa 1976), 2008, 33(12): E371-E377. DOI:10.1097/BRS.0b013e31817343a6 |
| [18] |
Ding C, Hong Y, Liu H, et al. Intermediate clinical outcome of Bryan cervical disc replacement for degenerative disk disease and its effect on adjacent segment disks[J]. Orthopedics, 2012, 35(6): e909-e916. DOI:10.3928/01477447-20120525-33 |
| [19] |
Pickett GE, Sekhon LH, Sears WR, et al. Complications with cervical arthroplasty[J]. J Neurosurg Spine, 2006, 4(2): 98-105. DOI:10.3171/spi.2006.4.2.98 |
| [20] |
Pickett GE, Mitsis DK, Sekhon LH, et al. Effects of a cervical disc prosthesis on segmental and cervical spine alignment[J]. Neurosurg Focus, 2004, 17(3): E5. |
| [21] |
Fong SY, DuPlessis SJ, Casha S, et al. Design limitations of Bryan disc arthroplasty[J]. Spine J, 2006, 6(3): 233-241. DOI:10.1016/j.spinee.2006.01.007 |
| [22] |
Sasso RC, Smucker JD, Hacker RJ, et al. Clinical outcomes of Bryan cervical disc arthroplasty: a prospective, randomized, controlled multicenter trial with 24-month follow-up[J]. J Spinal Disord Tech, 2007, 20(7): 481-491. DOI:10.1097/BSD.0b013e3180310534 |
| [23] |
江丽强, 岳亚玲, 颜继英, 等. 不同固定方法对颈椎单开门术后颈椎曲度和活动度的影响[J]. 现代中西医结合杂志, 2015, 24(22): 2445-2447. |
| [24] |
徐帅, 欧云生, 杜兴, 等. Prestige人工颈椎间盘置换术后异位骨化对颈椎活动度的影响[J]. 解剖学报, 2020, 51(3): 405-410. |
 2021, Vol.19
2021, Vol.19  Issue(2): 73-78
Issue(2): 73-78


