2. 海军军医大学长征医院骨肿瘤科, 上海 200003
2. Department of Bone Tumor, Changzheng Hospital, Navy Medical University, Shanghai 200003, China
颈椎后路单开门椎管扩大椎板成形术只需要将一侧椎板掀起,即可获得满意的减压效果,已被广泛应用于颈椎椎间盘突出症、颈椎椎管狭窄症及颈椎后纵韧带骨化症(OPLL)等疾病的治疗。该术式由Hirabayashi等[1]在20世纪80年代首次介绍,几十年来被不断改良。2004年,Park等[2]报道了椎板成形术并钛板固定的术式,该术式可有效保障椎弓根的生物力学稳定性,防止因椎板“再关门”而引起的神经症状恶化,文献[3-5]报道其在维持椎板稳定性,减少术后“再关门”现象的发生方面效果良好。但术中掀开椎板时,铰链侧偶尔会发生完全骨折离断,影响铰链处的骨性愈合,造成术后椎板不稳定,是发生椎板“再关门”和神经症状的潜在原因之一[6-7],甚至可能发生铰链侧椎板断端向椎管内塌陷而导致手术失败。有学者建议一旦出现铰链侧完全骨折,应行全椎板切除术,但椎板切除对颈椎的稳定性影响较大,可能导致颈椎不稳、后凸畸形等并发症发生[8];另有学者主张,当铰链侧椎板断裂不超过2个节段时,可不作处理[2]。本研究组通过总结临床经验,提出一种新型棘突悬吊法,用于固定颈椎单开门椎板成形术中铰链侧的断裂,发现其适用于椎板断裂不超过2个节段的情况,现报告如下。
1 资料与方法 1.1 病例资料2016年6月—2019年4月,海军军医大学长征医院采用ARCH钢板并单节段椎板成形术治疗多节段颈椎OPLL致椎管狭窄患者,术中发生铰链侧椎板断裂(≤2个节段)30例。早期发生铰链侧椎板断裂的15例患者未行任何处理(对照组),其中男8例、女7例,年龄为(50.67±11.29)岁;手术节段为C3~7者10例,C3~6者5例。后期的15例患者采用新型棘突悬吊法固定(试验组),其中男8例、女7例,年龄为(52.80±10.45)岁;手术节段为C3~7者9例,C3~6者6例。2组患者术前一般资料差异无统计学意义(P > 0.05),具有可比性。所有手术由同一医师团队完成。
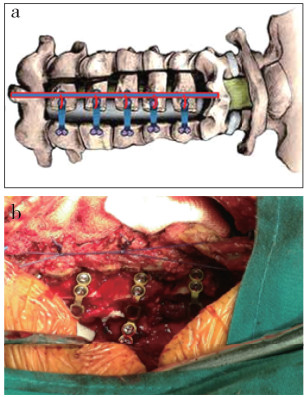
1.2 手术方法患者全身麻醉后取俯卧位,颈部稍前屈,与头部一并用石膏床固定。常规消毒铺巾,做颈部后正中切口,切开皮肤、皮下组织、项韧带,由棘突两侧骨膜下分离椎旁肌群,暴露C3~7椎板、棘突、关节突内侧。用尖刀切断C2/C3和C6/C7棘上、棘间韧带和黄韧带,保留C2、C7棘突及肌肉附着点。选择症状较重侧为开门侧,对侧为铰链侧。先在铰链侧距关节突内侧缘1.5 ~ 2.5 mm处用超声骨刀“V”形刀头开槽,对侧用超声骨刀在椎板和侧块交界处切开椎板全层,用枪钳小心咬除椎板内侧骨皮质。切开开门侧椎板间黄韧带,将C3~6椎板像“青枝骨折”一样向铰链侧掀起,打开椎板,小心分离硬膜外组织。用明胶海绵和脑棉片压迫椎管内静脉出血点,开门角度为45° ~ 60°。开门后,用钢板模具试模后,选用合适长度的ARCH钢板,分别对椎板开门侧进行固定。前期未对开门后发生铰链侧椎板完全骨折的病例进行任何处理(对照组);后期采用新型棘突悬吊法对铰链侧骨折椎板进行固定,将不可吸收缝线上下两端分别固定于C2、C7棘突,并在维持一定张力情况下向中轴缝线牵拉,以达到骨折端内侧缘稍高于外侧缘为标准(试验组,图 1)。用C形臂X线机透视确定钢板位置无误后,仔细探查硬膜外腔,彻底止血、冲洗,置负压引流管1根,清点器械敷料无误后逐层缝合伤口。术后72 h视引流量情况决定是否拔除引流管。引流管拔除后,佩戴颈托下床活动,并开始主动进行颈部屈伸活动,锻炼颈后肌群,颈托佩戴4周。
|
a:铰链侧骨折椎板的棘突中点用不可吸收缝线固定后向中轴牵拉固定(蓝红线代表术中使用的不可吸收缝线)b:术中C3,4铰链侧椎板断裂后采用新型棘突悬吊法固定 a: Midpoint of spinous process of hinge lateral lamina fracture is fixed with non absorbable suture and then pulled and fixed to central axis(blue-red line represents non-absorbable suture) b: New spinous process suspension method after C3, 4 hinge side fracture 图 1 新型棘突悬吊法固定操作 Fig. 1 Operation procedure of new spinous process suspension method |
记录并比较2组手术时间、术中出血量、术后引流量,术前及术后3个月疼痛视觉模拟量表(VAS)评分[9]、日本骨科学会(JOA)评分[10]、颈椎功能障碍指数(NDI)[11]、C2~7 Cobb角、颈椎曲度[12]、颈椎活动度(ROM)[13],以及术后并发症(轴性疼痛、感染、C5神经根麻痹、术后6个月椎板未愈合)发生情况。JOA评分改善率(%)=(术后JOA评分-术前JOA评分)/(17分-术前JOA评分)×100%。根据患者术后6个月横断面CT判断铰链侧骨折愈合情况,若椎板铰链处内外层骨皮质均连续连接则判断为骨折愈合;若椎板铰链处内外层骨皮质未连接或仅有内层皮质骨连接则判断为骨折未愈合[6]。
1.4 统计学处理采用SPSS 21.0软件对数据进行统计学分析,计量资料以x±s表示,组间比较采用独立样本t检验;等级变量资料采用χ2检验;以P < 0.05为差异有统计学意义。
2 结果所有患者随访10 ~ 35个月,平均20个月。对照组手术时间、术中出血量少于试验组,差异有统计学意义(P < 0.05,表 1)。2组术后3个月VAS评分、JOA评分、NDI、C2~7 Cobb角、颈椎曲度及颈椎ROM较术前显著改善,差异均有统计学意义(P < 0.05,表 1)。试验组术后3个月VAS评分、JOA评分、NDI及颈椎ROM优于对照组,差异均有统计学意义(P < 0.05,表 1)。2组术后3个月C2~7 Cobb角和颈椎曲度差异均无统计学意义(P > 0.05)。
|
|
表 1 2组观察指标 Tab. 1 Observation index of 2 groups |
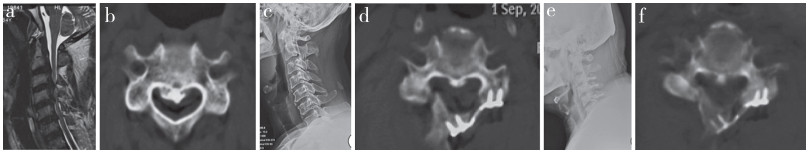
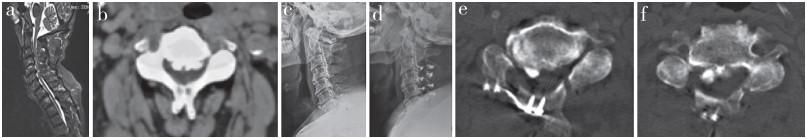
对照组发生轴性疼痛7例,感染2例,C5神经根麻痹4例,术后6个月椎板未愈合6例;试验组发生轴性疼痛1例,感染2例,C5神经根麻痹3例,术后6个月椎板未愈合3例。2组术后轴性疼痛发生情况差异有统计学意义(P < 0.05)。典型病例影像学资料见图 2、3。
|
男,54岁,脊髓型颈椎病,混合型OPLL,行C3~6单开门椎板成形术,术中C3,4铰链侧椎板断裂,采用新型棘突悬吊法固定a ~ c:术前影像学资料示明显OPLL并椎管内压迫d:术后3个月CT示铰链侧骨痂生成不明显,存在明显骨折线e:术后6个月X线片示内固定位置良好f:术后6个月CT示铰链侧明显骨痂形成,骨性连接形成 Male, 54 years old, cervical spondylotic myelopathy mixed type OPLL, treated with single-door cervical laminoplasty in C3-6, adopting new spinous process suspension method after C3, 4 hinge side fracture a-c: Preoperative imaging data show obvious OPLL and compression of spinal canal d: CT at postoperative 3 months shows no obvious callus formation on hinge side and obvious fracture line e: Roentgenograph at postoperative 6 months shows that position of internal fixation is good f: CT at postoperative 6 months shows obvious bone fusion on hinged side 图 2 试验组典型病例影像学资料 Fig. 2 Imaging data of a typical case in experiment group |
|
男,65岁,颈椎椎管狭窄,行C3~6单开门椎板成形术,术中C3,4铰链侧椎板完全骨折后未行处理a ~ c:术前影像学资料示颈椎生理曲度变直,C2~7后纵韧带及黄韧带骨化,继发多节段椎管狭窄d:术后3个月X线片示内固定位置良好e:术后3个月CT示铰链侧椎板骨折未愈合f:术后6个月CT示铰链侧椎板骨折线愈合不明显,骨痂生长不明显 Male, 65 years old, cervical spinal stenosis, treated with single-door cervical laminoplasty in C3-6, without any treatment after C3, 4 hinge side fracture a-c: Preoperative imaging data show that cervical curvature is straightened, and ossification of C2-7 posterior longitudinal ligament and ligamentum flavum results in multi-segment spinal stenosis d: Roentgenograph at postoperative 3 months shows that position of internal fixation is good e: CT at postoperative 3 months shows that hinge side fracture is not healed f: CT at postoperative 6 months shows fracture line of hinge side and growth of callus is not obvious 图 3 对照组典型病例影像学资料 Fig. 3 Imaging data of a typical case in control group |
目前,颈椎后路单开门椎板成形术是治疗多节段颈椎椎管狭窄症的经典术式,临床疗效满意。随着临床工作的深入以及术式的不断改良,微型钛板的应用得到了众多学者的认可。Rhee等[6]的研究发现,单纯微型钛板固定开门侧椎板与侧块可提供即时稳定性,有效维持开门状态,减少轴性疼痛、颈椎ROM丢失等并发症的发生。铰链侧椎板完全骨折是单开门椎板成形术中常见并发症,可通过术中发现的明显“咔嚓”骨折声,或术后即刻CT检查所示内、外皮质不连续或椎板铰链部位移位超过1 mm来识别。当铰链侧发生骨折时,可先行观察,不必要行临床干预[14]。根据以上原则,本研究组早期对不超过2个节段的铰链侧椎板完全骨折未行特别处理,结果显示,术后3个月VAS评分、JOA评分、NDI、C2~7 Cobb角、颈椎曲度及颈椎ROM均较术前显著改善,疗效满意。
铰链侧椎板的完全骨折使椎板处于不稳定状态,在颈部多轴向活动过程中椎板容易受到周围组织及肌肉的牵拉而出现移位,导致骨折延迟愈合甚至椎板内移塌陷,刺伤脊髓或造成椎管再狭窄而压迫脊髓。微型钛板的应用对椎体形成了半刚性的固定,虽然对铰链侧椎板有一定的稳定作用,但是,对于术中发生完全骨折的铰链侧椎板未能提供有力的支撑。因而在铰链侧骨折达到骨性愈合之前颈椎的早期活动可能会导致骨折不稳、移位甚至内移塌陷,最终导致手术失败。Chen等[15]的研究认为,由于颈椎活动及外部压力的影响,铰链侧椎板时常处于微动状态,不利于铰链侧骨折的愈合。颈椎活动是多轴向的,在颈椎活动过程中颈后肌群压力易传导至铰链侧,导致铰链侧骨折不愈合甚至迟发骨折。本研究对照组6例发生椎板未愈合且伴有明显骨折椎板移位,可能与铰链侧椎板骨折后缺乏有效固定及早期颈部肌肉锻炼有关。
轴性疼痛作为单开门椎板成形术后常见并发症,发生率为30% ~ 60%[16],常伴有颈椎生理曲度、ROM的丢失。有研究[17-20]发现,术中保持颈后肌肉-韧带复合体的完整性、开门侧刚性固定及术后早期功能锻炼能明显减少此类并发症的发生。还有研究[16, 21-22]发现,轴性疼痛症状与铰链侧椎板骨折的愈合情况有关,在对C2、C7棘突及椎旁肌肉组织做相同保留的情况下,铰链侧椎板骨折的患者轴性疼痛发生率较高;术后CT证实铰链侧椎板的骨性愈合有利于轴性疼痛症状的缓解。本研究对照组中7例术后发生轴性疼痛,可能原因为椎板受到颈后肌群屈伸活动的影响,导致完全骨折的铰链侧椎板不稳,在早期活动过程中,铰链侧椎板处于微动状态,对周围关节突及神经根造成刺激,而出现轴性疼痛症状。
后期本研究组采用新型棘突悬吊法固定完全骨折的铰链侧椎板,其可为铰链侧骨折椎板提供向内向后的拉力作用,维持椎板稳定,防止椎板移位、塌陷,适用于铰链侧椎板断裂不超过2个节段的情况,旨在降低术后轴性疼痛及椎板不愈合的发生率。本研究结果显示,试验组术后3个月VAS评分、JOA评分、NDI及颈椎ROM均优于对照组;术后6个月铰链侧椎板骨折愈合率为80%(12/15),没有出现明显的椎板移位,术后仅1例发生轴性疼痛,证明新型棘突悬吊法可在维持开门侧稳定的基础上防止骨折的铰链侧椎板移位,促进门轴侧椎板骨性愈合,降低轴性疼痛发生率。
本研究术中采用本院特制石膏床固定患者头颈部,使头颈部处于自然中立位,而并非头架式体位摆放时的颈部屈曲位,可避免术后中立位缝线松弛。且术中测试后仰动作,只要术中悬吊高度充足,颈部后仰时高度极少丢失,并不存在门轴侧再次关闭的可能,患者术后随访的影像学资料亦未发现嵌入椎管的情况。
综上,颈椎单开门椎板成形术中铰链侧椎板断裂后采用新型棘突悬吊法固定,更有利于降低患者术后颈椎功能障碍发生率,保留颈椎ROM,促进门轴侧椎板骨性愈合,减少轴性疼痛的发生。但本研究样本量较小,随访时间较短,尚需进一步纳入更多病例,延长随访时间观察其远期疗效。
| [1] |
Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy[J]. Spine(Phila Pa 1976), 1983, 8(7): 693-699. DOI:10.1097/00007632-198310000-00003 |
| [2] |
Park YK, Lee DY, Hur JW, et al. Delayed hinge fracture after plate-augmented, cervical open-door laminoplasty and its clinical significance[J]. Spine J, 2014, 14(7): 1205-1213. DOI:10.1016/j.spinee.2013.08.012 |
| [3] |
Liu G, Buchowski JM, Bunmaprasert T, et al. Revision surgery following cervical laminoplasty: etiology and treatment strategies[J]. Spine(Phila Pa 1976), 2009, 34(25): 2760-2768. DOI:10.1097/BRS.0b013e3181b11ee1 |
| [4] |
Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2:advantages of anterior decompression and fusion over laminoplasty[J]. Spine(Phila Pa 1976), 2007, 32(6): 654-660. DOI:10.1097/01.brs.0000257566.91177.cb |
| [5] |
Deutsch H, Mummaneni PV, Rodts GE, et al. Posterior cervical laminoplasty using a new plating system: technical note[J]. J Spinal Disord Tech, 2004, 17(4): 317-320. DOI:10.1097/01.bsd.0000091070.73042.23 |
| [6] |
Rhee JM, Register B, Hamasaki T, et al. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures[J]. Spine(Phila Pa 1976), 2011, 36(1): 9-14. DOI:10.1097/BRS.0b013e3181fea49c |
| [7] |
Lee DH, Park SA, Kim NH, et al. Laminar closure after classic Hirabayashi open-door laminoplasty[J]. Spine (Phila Pa 1976), 2011, 36(25): E1634-E1640. DOI:10.1097/BRS.0b013e318215552c |
| [8] |
Rhee JM, Basra S. Posterior surgery for cervical myelopathy: laminectomy, laminectomy with fusion, and laminoplasty[J]. Asian Spine J, 2008, 2(2): 114-126. DOI:10.4184/asj.2008.2.2.114 |
| [9] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [10] |
Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890-1895. DOI:10.1097/00007632-200109010-00014 |
| [11] |
Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409-415. |
| [12] |
Harrison DE, Harrison DD, Cailliet R, et al. Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods[J]. Spine(Phila Pa 1976), 2001, 26(11): E235-E242. DOI:10.1097/00007632-200106010-00003 |
| [13] |
Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people[J]. Spine(Phila Pa 1976), 1986, 11(6): 521-524. DOI:10.1097/00007632-198607000-00003 |
| [14] |
Lee DH, Kim H, Lee CS, et al. Clinical and radiographic outcomes following hinge fracture during open-door cervical laminoplasty[J]. J Clin Neurosci, 2017, 43: 72-76. DOI:10.1016/j.jocn.2017.04.037 |
| [15] |
Chen H, Liu H, Zou L, et al. Effect of mini-plate fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty[J]. Clin Spine Surg, 2016, 29(6): E288-E295. DOI:10.1097/BSD.0000000000000131 |
| [16] |
Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication[J]. Spine(Phila Pa 1976), 1996, 21(17): 1969-1973. DOI:10.1097/00007632-199609010-00005 |
| [17] |
Yeh KT, Chen IH, Yu TC, et al. Modified expansive open-door laminoplasty technique improved postoperative neck pain and cervical range of motion[J]. J Formos Med Assoc, 2015, 114(12): 1225-1232. DOI:10.1016/j.jfma.2014.10.005 |
| [18] |
Takeuchi K, Yokoyama T, Aburakawa S, et al. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3-C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis[J]. Spine(Phila Pa 1976), 2005, 30(22): 2544-2549. DOI:10.1097/01.brs.0000186332.66490.ba |
| [19] |
Sakaura H, Hosono N, Mukai Y, et al. C3-6 laminoplasty for cervical spondylotic myelopathy maintains satisfactory long-term surgical outcomes[J]. Global Spine J, 2014, 4(3): 169-174. DOI:10.1055/s-0034-1381727 |
| [20] |
Lee TT, Green BA, Gromelski EB. Safety and stability of open-door cervical expansive laminoplasty[J]. J Spinal Disord, 1998, 11(1): 12-15. |
| [21] |
Chiba K, Ogawa Y, Ishii K, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy-average 14-year follow-up study[J]. Spine(Phila Pa 1976), 2006, 31(26): 2998-3005. DOI:10.1097/01.brs.0000250307.78987.6b |
| [22] |
Chen G, Luo Z, Nalajala B, et al. Expansive open-door laminoplasty with titanium miniplate versus sutures[J]. Orthopedics, 2012, 35(4): e543-e548. DOI:10.3928/01477447-20120327-24 |
 2021, Vol.19
2021, Vol.19  Issue(2): 83-88
Issue(2): 83-88


