骨质疏松性椎体压缩性骨折(OVCF)主要表现为轻度或无外力冲击时出现腰背疼痛症状,影像学多见椎体骨折伴高度下降[1]。经皮椎体成形术(PVP)是临床上治疗OVCF的常用术式,具有镇痛效果佳、术后恢复快等优势,但该术式需将骨水泥加压注入椎体内,易出现骨水泥经静脉丛或骨折裂隙外渗等问题,不利于临床预后改善[2]。基于上述问题,国外学者对PVP术式进行改良,PVP术中采用新型Vessel-X骨材料填充器(Vessel-PVP)注入骨水泥,术中沿椎弓根入路于椎体内置入中空PET滤网,并经通道将骨水泥注入滤网内,在部分恢复椎体高度的同时限制骨水泥流动,降低骨水泥椎体外渗漏的风险[3]。目前,Vessel-PVP与传统PVP治疗OVCF的疗效对比报道仍相对较少,所得结论亦存在明显差异[3-4]。本研究对比了Vessel-PVP与传统PVP治疗老年OVCF的临床疗效及安全性,旨在为临床手术方案选择提供参考,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄≥65岁,符合骨质疏松诊断标准[5];②根据外伤史、症状及影像学检查确诊为单节段OVCF;③非手术治疗无效;④术前疼痛视觉模拟量表(VAS)评分[6] > 5分。排除标准:①椎体压缩程度 > 50%;②既往有脊柱手术史;③病理性骨折;④无法耐受手术或不愿接受手术治疗。按照上述标准,纳入2015年6月—2018年12月接受手术治疗的119例老年OVCF患者。前期67例患者采用传统PVP治疗(对照组),其中男37例、女30例,年龄为(74.47±6.85)岁,受伤至手术时间为(8.29±2.06)h;骨折节段:T11 3例,T12 22例,L1 18例,L2 13例,L3 8例,L4 3例。后期52例患者采用Vessel-PVP治疗(观察组),其中男28例、女24例,年龄为(75.01±6.99)岁,受伤至手术时间为(8.10±1.96)h;骨折节段:T11 3例,T12 18例,L1 16例,L2 9例,L3 5例,L4 1例。2组术前一般资料差异无统计学意义(P >0.05),具有可比性。研究方案符合《赫尔辛基宣言》要求,所有患者及家属知情同意并签署知情同意书。所有手术均由同一组医师完成。
1.2 手术方法对照组患者采用传统PVP治疗。观察组患者全身麻醉后取俯卧位,在标记的进针点处沿骨折椎体椎弓根外入路单侧穿刺,穿刺按术前CT测量规划的矢状位及水平位角度进行,当穿刺针在侧位透视下通过椎体后壁时,正位到达椎弓根内壁,继续旋转穿刺针至侧位透视到达椎体中后1/3交界点,拔出针芯,建立工作通道,置入扩张矫形器,顺时针缓慢旋转使金属弹片扩张,以恢复椎体高度并在椎体内形成一定程度的空腔。扩张满意后退出扩张器,置入新型Vessel-X骨材料填充网袋,透视时使其前端在侧位位于椎体前1/3、正位位于棘突附近,连接螺旋推进器,调试骨水泥,注入拉丝期骨水泥3.5 ~ 6.5 mL,X线透视下确认骨水泥逐步填充至网袋中,并缓慢逐层渗出至网袋边缘的松质骨内,骨水泥弥散良好后停止灌注。逆时针旋转注入管并退出,覆盖无菌敷料结束手术。
1.3 评价指标记录患者手术时间、住院时间,测量手术前后侧位X线片上骨折节段椎体前缘高度,评估伤椎高度恢复情况,椎体高度恢复率(%)=(术后椎体前缘高度-术前椎体前缘高度)/术前椎体前缘高度×100%。于术前、术后7 d、术后12个月记录患者VAS评分,评估临床疗效,VAS评分改善率(%)=(术前VAS评分-术后VAS评分)/术前VAS评分×100%。记录骨水泥渗漏情况。
1.4 统计学处理采用SPSS 20.0软件对数据进行统计分析,符合正态分布的计量资料以x±s表示,组间比较采用独立样本t检验,手术前后数据比较采用配对t检验;计数资料以百分比表示,组间比较采用χ2检验;以P <0.05为差异有统计学意义。
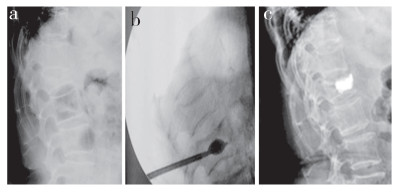
2 结果所有手术顺利完成。患者随访12 ~ 19(15.31±2.71)个月。2组术后7 d、术后12个月的VAS评分及伤椎前缘高度较术前明显改善,差异均有统计学意义(P <0.05,表 1);组间差异无统计学意义(P >0.05,表 1)。2组骨水泥注入量、手术时间、住院时间、椎体高度恢复率及骨水泥渗漏率差异均无统计学意义(P >0.05,表 1)。观察组典型病例影像学资料见图 1。
|
|
表 1 2组患者统计数据 Tab. 1 Statistical data of patients in 2 groups |
|
男,78岁,L1 OVCF,伤后1周采用Vessel-PVP治疗a:术前侧位X线片示L1椎体压缩b:术中骨填充网袋置入c:术后3 d侧位X线片示骨水泥弥散良好 Male, 78 years old, L1 OVCF, Vessel-PVP is performed at 1 week after injury a: Preoperative lateral roentgenograph shows L1 vertebral compression b: Bone-filled mesh bag is placed during operation c: Lateral roentgenograph at postoperative 3 d shows bone cement is well dispersed 图 1 观察组典型病例影像学资料 Fig. 1 Imaging data of a typical case in observation group |
PVP是最早应用于临床的椎体强化技术,目前已成为老年OVCF的主要微创治疗手段。PVP治疗OVCF主要不良事件为骨水泥渗漏,发生率可达80%,即使行经皮椎体后凸成形术(PKP)治疗,这一比例亦接近25%[7]。有研究[8]报道,术后骨水泥渗漏大多数情况下不会发生严重并发症,但渗漏至椎管造成硬膜或神经根压迫则可出现明显症状,渗漏入血管可能引起肺栓塞,严重者危及生命。骨折严重程度和骨水泥黏稠度被认为与骨水泥渗漏的发生密切相关,术前影像学检查有助于判断皮质破坏程度及椎体内部裂隙,降低渗漏发生风险[9]。一项针对活体解剖标本的研究[10]证实,伤椎内仅需注入3.5 mL骨水泥即可纠正椎体间应力分布异常,注入7.0 mL骨水泥椎弓间正常压力负担可恢复,但此时骨水泥渗漏概率增加2 ~ 3倍。有研究[11]报道,对于骨质疏松不全性爆裂性骨折患者,经椎弓根置入中空钛网后再注入骨水泥有助于降低骨水泥渗漏发生的风险。
Vessel-PVP采用的骨材料填充网袋主要成分为涤纶树脂,具有良好的生物相容性[12]。骨材料填充网袋置入椎体内,骨水泥经网孔分次缓慢弥散至椎体骨小梁间隙,骨水泥与周围骨组织结合,并能够维持稳定弥散形态,降低骨水泥渗漏风险,且骨水泥逐渐填充使网袋膨胀,进一步抬高终板,骨水泥注入与椎体高度恢复同步完成,无回弹现象发生风险,这对改善椎体高度具有重要意义[13]。Vessel-PVP已被广泛应用于OVCF、血管瘤及转移瘤等疾病的治疗,止痛效果好,骨水泥渗漏发生率低[14]。本研究中2组骨水泥渗漏率差异无统计学意义,分析原因可能是早期观察组骨水泥注射速度较快,而对照组采用缓慢注射和逐步退针的方法,注射速度控制在每分钟1.0 mL以内,降低了骨水泥经骨缝流出椎体外的风险。本研究中对照组骨水泥渗漏率(13.43%)较既往报道[15]显著降低,同时未见椎管内渗漏和肺栓塞发生,椎旁静脉、椎旁骨膜下渗漏等均未引起明显症状。有研究[16]报道,Vessel-PVP能够促进OVCF患者椎体高度恢复。但本研究结果显示,2组术后7 d椎体高度恢复率差异无统计学意义,主要原因可能为其球囊工作原理与PKP存在差异,PKP球囊属于密闭型,而Vessel-PVP球囊因有网孔难以实现囊内闭合加压[17]。
综上,Vessel-PVP治疗老年OVCF临床疗效及安全性满意,但较PVP并未显现出明显优势,且操作更为耗时;PVP术中无须球囊置入,更为简便,仍应将PVP作为首选术式。此外,笔者认为Vessel-PVP更适用于椎管后壁轻度破损的患者,能够在促进椎体高度部分恢复的同时,预防骨水泥渗漏的发生。
本研究不足之处:①为单中心回顾性研究,纳入样本量相对较小,可能存在选择偏倚;②仅评估短期疗效,有待后续开展长期随访研究以评估总体疗效。
| [1] |
陈吉, 陈勇, 张征石, 等. 骨质疏松性椎体压缩性骨折经皮椎体后凸成形术中骨水泥渗漏原因回顾性分析[J]. 中华骨质疏松和骨矿盐疾病杂志, 2017, 10(1): 27-33. |
| [2] |
Zhu Y, Cheng J, Yin J, et al. Therapeutic effect of kyphoplasty and balloon vertebroplasty on osteoporotic vertebral compression fracture: a systematic review and meta-analysis of randomized controlled trials[J]. Medicine(Baltimore), 2019, 98(45): e17810. |
| [3] |
Chen Z, Wu Y, Ning S, et al. Risk factors of secondary vertebral compression fracture after percutaneous vertebroplasty or kyphoplasty: a retrospective study of 650 patients[J]. Med Sci Monit, 2019, 25: 9255-9261. DOI:10.12659/MSM.915312 |
| [4] |
唐海, 贾璞, 陈浩, 等. 新型Vessel-X经皮椎体强化系统在脊柱微创治疗的临床应用[J]. 中华医学杂志, 2017, 97(33): 2567-2572. DOI:10.3760/cma.j.issn.0376-2491.2017.33.003 |
| [5] |
夏维波, 章振林, 林华, 等. 原发性骨质疏松症诊疗指南(2017)[J]. 中华骨质疏松杂志, 2019, 25(3): 281-309. |
| [6] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [7] |
罗学勤. 椎体成形术中采用高黏度骨水泥治疗胸腰椎重度骨质疏松性椎体压缩性骨折[J]. 脊柱外科杂志, 2020, 18(1): 34-37. |
| [8] |
Félix S, Humbert M, Büla C, et al. Vertebroplasty in elderly patients: is less still too much?[J]. Rev Med Suisse, 2019, 15(670): 2027-2031. |
| [9] |
Hanke A, Bäumlein M, Lang S, et al. Long-term radiographic appearance of calcium-phosphate synthetic bone grafts after surgical treatment of tibial plateau fractures[J]. Injury, 2017, 48(12): 2807-2813. DOI:10.1016/j.injury.2017.10.030 |
| [10] |
Barbieri D, Yuan H, Ismailoğlu AS, et al. Comparison of two moldable calcium phosphate-based bone graft materials in a noninstrumented canine interspinous implantation model[J]. Tissue Eng Part A, 2017, 23(23-24): 1310-1320. DOI:10.1089/ten.tea.2016.0347 |
| [11] |
Parkkinen M, Lindahl J, Mäkinen TJ, et al. Predictors of osteoarthritis following operative treatment of medial tibial plateau fractures[J]. Injury, 2018, 49(2): 370-375. DOI:10.1016/j.injury.2017.11.014 |
| [12] |
Erden T, Batar S, Uzer G, et al. Early results of the medial approach for arthroscopic-assisted fixation of lateral tibial plateau fractures[J]. Orthop J Sports Med, 2017, 5(Suppl 2): 170-174. |
| [13] |
许兵, 王萧枫, 叶小雨, 等. 骨填充网袋椎体成形术与经皮球囊后凸成形术治疗骨质疏松性椎体压缩性骨折[J]. 中国骨伤, 2018, 31(11): 993-997. |
| [14] |
Duan ZK, Zou JF, He XL, et al. Bone-filling mesh container versus percutaneous kyphoplasty in treating Kümmell's disease[J]. Arch Osteoporos, 2019, 14(1): 109. DOI:10.1007/s11657-019-0656-4 |
| [15] |
Zhong W, Liang X, Luo X, et al. Vertebroplasty and vertebroplasty in combination with intermediate bilateral pedicle screw fixation for OF4 in osteoporotic vertebral compression fractures: a retrospective single-centre cohort study[J]. BMC Surg, 2019, 19(1): 178. DOI:10.1186/s12893-019-0646-x |
| [16] |
He CJ, Liu GD. Comparison of the efficacy and safety of bone-filling mesh container and simple percutaneous balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures[J]. Pain Physician, 2018, 21(3): 259-268. |
| [17] |
Zhong R, Liu J, Wang R, et al. Unilateral curved versus bipedicular vertebroplasty in the treatment of osteoporotic vertebral compression fractures[J]. BMC Surg, 2019, 19(1): 193. |
 2021, Vol.19
2021, Vol.19  Issue(5): 318-321
Issue(5): 318-321

