颈椎后路单开门椎管扩大椎板成形术已广泛应用于治疗发育性颈椎椎管狭窄症(CSS)、多节段脊髓型颈椎病(MCSM)及后纵韧带骨化症(OPLL)等疾病,经过长期临床观察,颈椎后路单开门椎管扩大椎板成形术在改善神经功能方面具有显著疗效[1-2]。然而,传统的单开门手术需要广泛剥离两侧椎旁肌肉和韧带,术后存在诸多并发症,如颈部轴性疼痛、颈部僵硬、颈椎曲度丢失,甚至出现颈椎后凸畸形等[3-6]。为了减少对后方肌肉-韧带结构的损伤、减少相关并发症,本研究组采用颈椎后路单侧显露通道辅助下椎管扩大椎板成形术治疗颈椎退行性疾病,初步效果良好,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄>30岁且<80岁;②确诊为MCSM、CSS、OPLL,并采用椎管扩大椎板成形术治疗;③均接受颈椎X线、CT三维重建及MRI检查且随访资料完整。排除标准:①严重骨质疏松;②强直性脊柱炎、类风湿关节炎等疾病;③颈椎畸形、外伤、感染、肿瘤等病史;④颈椎手术史。本研究纳入2020年9月—2021年11月符合上述标准的64例患者,其中36例采用颈椎后路单侧显露通道辅助进行手术(通道组),28例采用传统后路进行手术(对照组)。2组患者术前一般资料差异无统计学意义(P>0.05,表 1),具有可比性。2组手术均由同一组医师完成。
|
|
表 1 2组患者一般资料 Tab. 1 General data of 2 groups |
对照组患者全身麻醉后取俯卧位,取颈后正中切口切开皮肤,显露C3~7皮下筋膜,经棘突两侧骨膜下电刀分离肌肉,显露C3~7椎板及侧块内缘。在C3~7椎板右侧与侧块交界处用磨钻磨除表层骨皮质,开槽作为铰链侧;椎板左侧与侧块交界处用磨钻磨至内层骨皮质,用2 mm枪钳咬除剩余骨质,作为开门侧。用椎板夹持器夹持椎板并旋转,逐个掀开开门,使用ARCH钛板(强生,美国)固定于开门侧。常规生理盐水冲洗,放置负压引流管后关闭切口,术后48~72 h拔除引流管,术后第2天鼓励患者佩戴颈托下床活动。
通道组患者全身麻醉后取俯卧位,取颈后正中切口切开皮肤,显露C3~7皮下筋膜,手指触摸棘突左侧分叉处,电刀沿棘突左侧骨膜下剥离,显露C3~7椎板左侧及侧块内缘,磨钻磨至内层骨皮质,初步估计磨除的深度。于C3棘突右侧旁1.0~1.5 cm处,经椎旁肌直接穿刺置入可扩张通道(自主研发设计,两扩张叶片远端宽5 mm、近端宽8 mm;图 1a),通道可向头端、尾端倾斜移动。根据开门侧的预估深度,用3 mm磨钻头开槽制作铰链,完毕后取出通道。相同步骤处理C4~7椎板。开门侧用2 mm枪钳咬除剩余骨质,使之完全离断,用椎板夹持器夹持椎板并旋转,逐个开门。C3开门不需要切除C2/C3节段棘间韧带、棘上韧带等后方韧带结构,C7开门需要切除C7/T1节段棘间韧带、棘上韧带等后方韧带结构。使用ARCH钛板(强生,美国)固定开门侧。手术结束后,铰链侧肌肉韧带基本完好(图 1b)。

|
图 1 通道组术中通道置入 Fig. 1 Intraoperative channel placement in channel group a:术中置入自主研发设计的可扩张通道,磨钻于通道下制作铰链 b:术后铰链侧肌肉韧带基本完好 a: Self-developed expandable channel is inserted intraoperatively, and hinge is made by drill grinding under channel b: Muscle and ligaments on hinge side are basically intact after surgery |
记录2组患者手术时间、住院时间、术中出血量、术后引流量等指标及并发症发生情况。于术前、术后即刻、术后2个月及末次随访时采用疼痛视觉模拟量表(VAS)评分[7]评估颈部和上肢疼痛程度,采用颈椎功能障碍指数(NDI)[8]和日本骨科学会(JOA)评分[9]评估神经功能状况。
1.4 统计学处理采用SPSS 18.0软件对数据进行统计分析,符合正态分布的计量资料以x±s表示,患者一般情况比较采用χ2检验,组内手术前后数据比较采用重复测量方差分析,组间数据比较采用独立样本t检验。以P<0.05为差异有统计学意义。
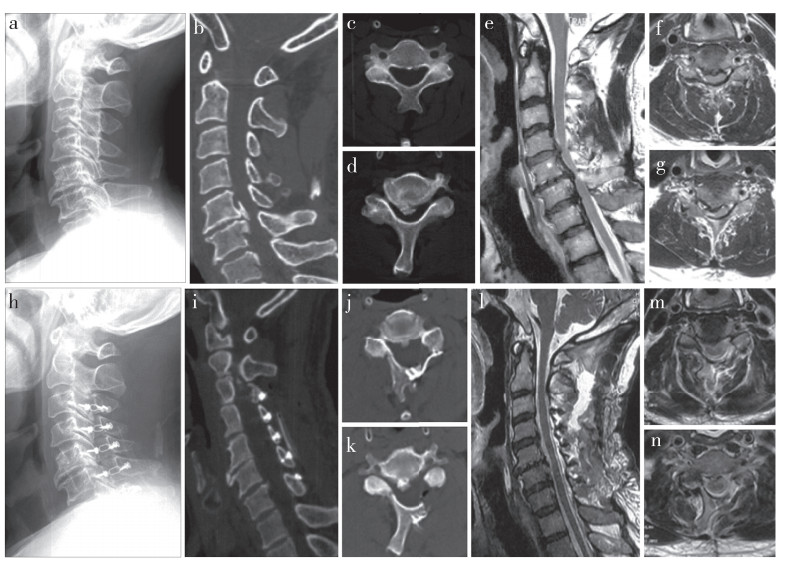
2 结果所有手术顺利完成。所有患者随访3~16个月,平均7.8个月。术后未发生神经损伤、感染等并发症。2组手术时间、住院时间差异无统计学意义(P>0.05,表 2)。通道组术中出血量和术后引流量均明显小于对照组,差异有统计学意义(P<0.05,表 2)。末次随访时2组颈痛VAS评分均较术前显著改善,且术后即刻、术后2个月通道组颈痛VAS评分低于对照组,差异均有统计学意义(P<0.05,表 2)。2组术后各时间点上肢痛VAS评分、NDI及JOA评分均较术前明显改善,差异有统计学意义(P<0.05,表 2);各时间点组间差异无统计学意义(P>0.05,表 2)。通道组典型病例影像学资料见图 2。
|
|
表 2 2组疗效评估指标比较 Tab. 2 Comparison of efficacy indexes of 2 groups |
|
图 2 通道组典型病例影像学资料 Fig. 2 Imaging data of a typical case in channel group a~d:术前侧位X线片、矢状位及横断面CT示颈椎OPLL,C5,6椎管内骨性占位 e~g:术前矢状位及横断面MRI示C5,6水平脊髓明显受压 h~k:术后侧位X线片、矢状位及横断面CT示C5,6椎管扩大,铰链骨槽位置理想 l~n:术后矢状位、横断面MRI示C5,6水平脊髓减压充分 a-d: Preoperative lateral roentgenograph, sagittal and cross-sectional CTs show cervical OPLL, bony mass in spinal canal of C5, 6 e-g: Preoperative sagittal and cross-sectional MRIs show obvious spinal cord compression at C5, 6 levels h-k: Postoperative lateral roentgenographs, sagittal and cross-sectional CTs show enlargement of C5, 6 spinal canals and ideal position of hinge bone slot l - n: Postoperative sagittal and cross-sectional MRIs show sufficient spinal decompression at C5, 6 levels |
传统的颈椎后路单开门椎管扩大椎板成形术需要广泛剥离肌肉、韧带,术后患者会出现颈椎曲度进一步丢失、颈部轴性疼痛发生率增加等问题[10-13],鹅颈畸形发生率达10%[14],即使术中行肌肉、韧带断端缝合重建,术后肌肉萎缩仍然明显[15]。为了避免术中广泛剥离肌肉、韧带,有学者[16-17]尝试保留颈后肌肉-韧带复合体的改良单开门椎管扩大椎板成形术,术中常规显露椎板左侧,于棘突基底截断棘突,将棘突及附着的肌肉、韧带推向右侧,骨膜下显露椎板,制作铰链,完成单开门手术,可降低术后轴性症状发生率。但该方法的弊端也显而易见:破坏棘突完整性、铰链侧仍需剥离肌肉和韧带、需要重建棘突稳定性。由解剖学基础得知,回旋短肌起于横突,止于上位椎体棘突基底部;回旋长肌也起于横突,向上跨越一个椎体后止于棘突基底部;多裂肌起自骶骨背面、腰椎、胸椎横突和C4~7关节突,肌束跨越2~4个椎骨后止于除寰椎外的棘突基底部。该手术方法可能会破坏颈部回旋肌和多裂肌的完整性,并且,颈后肌肉-韧带复合体通过棘突来传递各种应力,术中破坏了棘突的完整性,颈后肌肉-韧带复合体的力学作用也大大降低[18]。因此,改良手术仍存在一定缺陷,需要进一步改进。
颈后的深层伸肌,如颈半棘肌和多裂肌,直接附着于棘突,对颈椎的后伸和稳定起到重要作用。常规的椎管扩大椎板成形术需要破坏深层伸肌,术后可能会发生颈椎不稳,如能有效保留深层伸肌的完整性,对颈椎的运动功能有积极意义。如果开门及铰链侧都通过头半棘肌和颈半棘肌之间的肌肉间隙进行显露,可减少手术创伤,对维持颈椎曲度、降低术后轴性症状的发生率有一定帮助[19-21]。但是,该方法存在明显弊端,双侧显露需要于棘突末端离断项韧带、头夹肌、颈夹肌,破坏了头半棘肌、颈半棘肌更深面的肌肉,如多裂肌、颈回旋肌,虽保留了附着于棘突的部分深层伸肌,但需要广泛剥离多裂肌、颈回旋肌在关节突关节处的附着点才能显露椎板制作铰链,术中肌肉、韧带的损伤较重。
Hosono等[22]提出采用超声骨刀制作铰链的方法,开门侧常规显露,用小的剥离器插入棘突间隙,骨膜下剥离肌肉、韧带,并将其推向对侧,显露铰链侧椎板,用超声骨刀做“V”形开槽,开门侧用磨钻开槽,开门后铰链侧“V”形开槽处正好闭合。作者认为这样可以减少铰链侧肌肉、韧带的损伤,但也存在铰链侧的开槽位置显露受限,导致开槽位置过于靠近棘突等不足;肥胖或肌肉发达的患者,显露C6、C7椎板的难度增加,如患者存在项韧带钙化,此方法显露椎板将更加困难。
鉴于上述技术的不足之处,本研究组提出颈椎后路单侧显露通道辅助下椎管扩大椎板成形术,该技术可最大程度保留铰链侧肌肉、韧带的完整性。使用该技术的注意事项:①术中先显露开门侧,于椎板与侧块内缘处用磨钻磨至内层骨皮质,并记录磨除的深度,再于铰链侧置入可扩张通道,根据开门侧的预估深度,用3 mm磨钻头开槽制作铰链。②C3开门不需要离断C2/C3节段的棘间韧带和棘上韧带,C7开门需要离断C7/T1节段的棘间韧带和棘上韧带。本研究组在术中尝试保留C7/T1节段的棘间韧带、棘上韧带,发现开门程度不足,故只能离断。该术式最大的优点是保留了棘突的完整性、没有破坏铰链侧肌肉和韧带在棘突、关节突关节处的附着点,穿刺方法、置入通道大大减少了肌肉、韧带在骨性结构附着点的剥离,从而显著降低了铰链侧肌肉、韧带的损伤,减少了术中出血量和术后引流量。对比文献[16-22]报道中减少铰链侧肌肉、韧带损伤的方法,本研究组认为该方法目前最为微创、有效。
本研究样本量较小,缺乏中长期随访结果;该术式对颈椎整体曲度、颈椎活动度及颈椎稳定性的影响,将是今后进一步的研究重点。综上,与常规术式相比,颈椎后路单侧显露通道辅助下椎管扩大椎板成形术能有效减少铰链侧肌肉和韧带损伤,减少术中出血量、术后引流量及降低术后早期轴性颈痛发生率。
| [1] |
Lopez WY, Goh BC, Upadhyaya S, et al. Laminoplasty—an underutilized procedure for cervical spondylotic myelopathy[J]. Spine J, 2021, 21(4): 571-577. DOI:10.1016/j.spinee.2020.10.021 |
| [2] |
Machino M, Ando K, Kobayashi K, et al. Risk factors for poor outcome of cervical laminoplasty: multivariate analysis in 505 patients with cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976), 2021, 46(5): 329-336. DOI:10.1097/BRS.0000000000003783 |
| [3] |
Nori S, Shiraishi T, Aoyama R, et al. Muscle-preserving selective laminectomy maintained the compensatory mechanism of cervical lordosis after surgery[J]. Spine (Phila Pa 1976), 2018, 43(8): 542-549. DOI:10.1097/BRS.0000000000002359 |
| [4] |
Lee SH, Son DW, Lee JS, et al. Does extension dysfunction affect postoperative loss of cervical lordosis in patients who undergo laminoplasty?[J]. Spine(Phila Pa 1976), 2019, 44(8): E456-E464. DOI:10.1097/BRS.0000000000002887 |
| [5] |
Liu J, Xie R, Ruan H, et al. The preoperative cross-sectional area of the deep cervical extensor muscles does not predict loss of lordosis after cervical laminoplasty[J]. Clin Spine Surg, 2022, 35(1): E181-E186. DOI:10.1097/BSD.0000000000001199 |
| [6] |
Nakashima H, Kanemura T, Satake K, et al. Reoperation for late neurological deterioration after laminoplasty in individuals with degenerative cervical myelopathy: comparison of cases of cervical spondylosis and ossification of the posterior longitudinal ligament[J]. Spine(Phila Pa 1976), 2020, 45(15): E909-E916. DOI:10.1097/BRS.0000000000003408 |
| [7] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [8] |
Vernon H, Mior S. The neck disability index: a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409-415. |
| [9] |
Yonenobu K, Wada E, Tanaka T, et al. Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire(JOACMEQ): Part 2. Endorsement of the alternative item[J]. J Orthop Sci, 2007, 12(3): 241-248. DOI:10.1007/s00776-007-1119-0 |
| [10] |
Kim KR, Lee CK, Park JY, et al. Preoperative parameters for predicting the loss of lordosis after cervical laminoplasty[J]. Spine(Phila Pa 1976), 2020, 45(21): 1476-1484. DOI:10.1097/BRS.0000000000003604 |
| [11] |
Mun HW, Yuk CD, Kim TH, et al. Cervical sagittal imbalance after cervical laminoplasty in elderly patients[J]. Biomed Res Int, 2020, 2020: 8810540. |
| [12] |
Kimura A, Shiraishi Y, Inoue H, et al. Predictors of persistent axial neck pain after cervical laminoplasty[J]. Spine(Phila Pa 1976), 2018, 43(1): 10-15. DOI:10.1097/BRS.0000000000002267 |
| [13] |
Cheung JPY, Cheung PWH, Law K, et al. Postoperative rigid cervical collar leads to less axial neck pain in the early stage after open-door laminoplasty—a single-blinded randomized controlled trial[J]. Neurosurgery, 2019, 85(3): 325-334. DOI:10.1093/neuros/nyy359 |
| [14] |
Sinha S, Jagetia A. Bilateral open-door expansive laminoplasty using unilateral posterior midline approach with preservation of posterior supporting elements for management of cervical myelopathy and radiculomyelopathy—analysis of clinical and radiological outcome and surgical technique[J]. Acta Neurochir (Wien), 2011, 153(5): 975-984. DOI:10.1007/s00701-010-0872-6 |
| [15] |
Shiraishi T, Yato Y, Yoshida H, et al. New double-door laminoplasty procedures to preserve the muscular attachments to the spinous processes including the axis[J]. Eur J Orthop Surg Traumatol, 2002, 12(4): 175-180. DOI:10.1007/s00590-002-0050-5 |
| [16] |
Lee YS, Lee S, Ko MJ, et al. Preservation of deep cervical extensor muscle volume: comparison between conventional open-door and muscle preserving laminoplasty approaches in the same patients[J]. World Neurosurg, 2020, 141: e514-e523. DOI:10.1016/j.wneu.2020.05.225 |
| [17] |
Chen C, Yang C, Yang S, et al. Clinical and radiographic outcomes of modified unilateral open-door laminoplasty with posterior muscle-ligament complex preservation for cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976), 2019, 44(24): 1697-1704. DOI:10.1097/BRS.0000000000003158 |
| [18] |
Mesregah MK, Buchanan IA, Formanek B, et al. Intra- and post-complications of cervical laminoplasty for the treatment of cervical myelopathy: an analysis of a nationwide database[J]. Spine(Phila Pa 1976), 2020, 45(20): E1302-E1311. DOI:10.1097/BRS.0000000000003574 |
| [19] |
Park JH, Jeong EK, Lee MK, et al. A unilateral open door laminoplasty technique: prospective analysis of the relationship between midline extensor muscle preservation and postoperative neck pain[J]. J Clin Neurosci, 2015, 22(2): 308-314. DOI:10.1016/j.jocn.2014.07.018 |
| [20] |
Guo Q, Xu Y, Fang Z, et al. Clinical and radiological outcomes of two modified open-door laminoplasties based on a novel paraspinal approach for treatment of multilevel cervical spondylotic myelopathy[J]. Spine(Phila Pa 1976), 2021, 47(6): E222-E232. |
| [21] |
王占超, 吴晓东, 王新伟, 等. 肌间隙入路与传统后路单开门成形术治疗多节段颈椎退行性疾病的临床疗效[J]. 脊柱外科杂志, 2018, 16(1): 35-40. DOI:10.3969/j.issn.1672-2957.2018.01.008 |
| [22] |
Hosono N, Sakaura H, Mukai Y, et al. En bloc laminoplasty without dissection of paraspinal muscles[J]. J Neurosurg Spine, 2005, 3(1): 29-33. DOI:10.3171/spi.2005.3.1.0029 |
 2022, Vol.20
2022, Vol.20  Issue(5): 289-294
Issue(5): 289-294


