目前,社会老龄化逐渐加剧,退行性腰椎滑脱的发生率约为5%~7%,常合并腰腿疼痛、间歇性跛行、马尾神经综合征等,严重影响患者生活质量[1]。微创经椎间孔入路腰椎椎间融合术(MIS-TLIF)逐渐成为临床治疗腰椎退行性疾病的常用术式[2]。经过近15年的不断研究,为减少经腰大肌入路相关并发症的发生,Silvestre等[3]于2012年首次报道了斜外侧腰椎椎间融合术(OLIF)。与传统前路手术相比,该术式的腰丛神经损伤发生率明显降低[4]。本研究采用OLIF和MIS-TLIF治疗单节段轻中度腰椎滑脱患者,对比分析其临床疗效和影像学结果,现报告如下。
1 临床资料 1.1 一般资料纳入标准:①反复腰骶部疼痛伴下肢神经症状或间歇性跛行,严重影响生活质量;②影像学检查提示单节段Meyerding Ⅰ或Ⅱ度椎体滑脱(L3/L4或L4/L5);③诊断明确后经非手术治疗3~6个月,症状未见缓解;④合并马尾神经综合征。排除标准:①既往有腰椎手术史;②腰椎肿瘤、感染;③严重的脊柱畸形(强直性脊柱炎、脊柱侧凸等);④合并心肺功能不全、血液疾病、严重骨质疏松症等基础疾病。
根据上述标准,纳入2015年2月—2018年2月收治的单节段(L3/L4或L4/L5)Meyerding Ⅰ或Ⅱ度椎体滑脱患者48例,其中22例采用OLIF治疗(OLIF组),26例采用MIS-TLIF治疗(MIS-TLIF组)。2组患者术前基线资料差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 2组患者基线资料 Tab. 1 Baseline data of patients in 2 groups |
2组手术均由同一组医师配合完成。
OLIF组患者全身麻醉后取右侧卧位,左侧向上。定位后,确定目标椎间隙并标记椎间隙中部,在该点前4~10 cm处做一4~5 cm皮肤切口。逐层切开皮肤、腹外斜肌筋膜,用手指钝性分离腹外斜肌、内斜肌、背侧深横筋膜和腹横肌,进入腹膜后间隙。用示指或“花生米”钝性分离横筋膜,用示指绕筋膜下表面行圆周探查,确保腹膜不与筋膜粘连,然后沿腹壁内侧及腰方肌方向确定触及腰椎横突及腰大肌,注意保护腹腔内容物及输尿管等重要结构。用克氏针定位责任椎间盘,透视确认无误后放置工作套管,切开纤维环(至少1.8 cm),使用髓核钳清除髓核,然后将撑开器穿过椎间盘插入并旋转以释放对侧纤维环。由小到大进行试模,透视确认椎间高度及椎间孔大小恢复后选择尺寸匹配的融合器。取同种异体骨填充融合器,先倾斜进入,然后垂直旋转,将其垂直放置在椎间隙,C形臂X线机侧位透视确认椎间融合器位于椎间盘前1/3和中1/3之间,正位透视融合器位于椎间隙中心位置。取2枚直径为6.5 mm的前外侧螺钉置入上下椎体,长度约等于椎体宽度,椎体螺钉的进钉点靠近邻近终板,放置连接棒固定。冲洗术野,逐层缝合切口,留置引流管。
MIS-TLIF组患者全身麻醉后取平卧位,采用双侧Wiltse入路,具体手术流程参照陈斌彬等[5]的方法。
1.3 观察指标记录手术时间、术中出血量、住院时间及并发症发生情况;术前及术后1周、1个月、6个月及末次随访时采用疼痛视觉模拟量表(VAS)评分[6]和Oswestry功能障碍指数(ODI)[7]评估腰腿痛程度及腰椎功能。术前和末次随访时,在侧位X线片上测量手术节段Cobb角(手术节段上位椎体上终板与下位椎体下终板延长线间的夹角,图 1a)和腰椎前凸角(LL,L1与S1上终板延长线间的夹角,图 1b),在矢状面CT上测量椎间高度(DH,椎间隙前缘与后缘高度和的平均值,图 1c)和椎间孔面积(FA,图 1c):在横断面MRI上测量椎管横截面积(CSA,图 1d)。
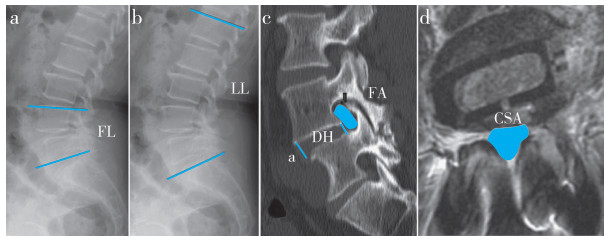
|
图 1 腰椎参数测量 Fig. 1 Measurement of lumbar parameters a:侧位X线片上测量手术节段Cobb角 b:侧位X线片上测量LL c:矢状面CT上测量DH,FA d:横断面MRI上测量椎管CSA a: Measurement of operative segment Cobb angle on lateral roentgenograph b: Measurement of LL on lateral roentgenograph c: Measurement of DH and FA on sagittal CT d: Measurement of spinal canal CSA on axial MRI |
采用SPSS 21.0软件对数据进行统计分析,符合正态分布的计量资料以x±s表示,组间数据两两比较采用独立样本t检验,组内各时间点数据比较采用单因素方差分析,手术前后数据比较采用配对t检验;计数资料以频数表示,组间比较采用χ2检验;以P < 0.05为差异有统计学意义。
2 结果所有手术顺利完成,所有患者随访24~45个月,平均32.8个月。OLIF组手术时间、术中出血量及住院时间明显少于MIS-TLIF组,差异均有统计学意义(P < 0.05,表 2)。2组术后各随访时间点VAS评分和ODI较术前明显改善,差异均有统计学意义(P < 0.05,表 2);术后1周OLIF组VAS评分和ODI优于MIS-TLIF组,差异均有统计学意义(P < 0.05,表 2)。2组末次随访时LL、手术节段Cobb角、DH、椎管CSA和FA较术前明显改善,差异均有统计学意义(P < 0.05,表 2);末次随访时OLIF组LL、手术节段Cobb角、DH和FA矫正值优于MIS-TLIF组,差异均有统计学意义(P < 0.05,表 2)。
|
|
表 2 2组临床疗效指标比较 Tab. 2 Comparison of efficacy indexes between 2 groups |
OLIF组并发症发生率为13.6%(3/22):术中节段动脉损伤1例,术中通过双极电凝及明胶海绵填塞止血处理后无进行性出血;术侧腰大肌无力合并大腿外侧麻木1例,左侧交感干损伤1例,术后常规指导患者进行功能锻炼并给予甲钴胺肌肉注射营养神经等处理,均于术后3个月症状完全消失。MIS-TLIF组并发症发生率为15.4%(4/26):术中硬膜撕裂1例,术中进行初步修复,未造成不良后遗症;术后出现神经根性症状2例,顽固性腰痛1例,术后采用维生素B、α-硫辛酸、甲钴胺和阿米替林等药物治疗,3个月后腰背部疼痛和精神障碍均有所改善。2组均未发生融合器移位、塌陷、螺钉退钉失效等并发症。2组典型病例影像学资料见图 2、3。
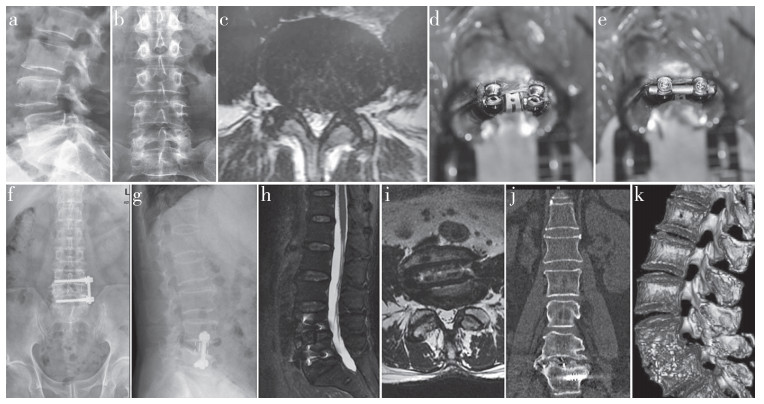
|
图 2 OILF组典型病例影像学资料 Fig. 2 Imaging data of a typical case in OILF group 男,42岁,L4/L5节段MeyerdingⅠ度滑脱 a、b:术前正侧位X线片示L4Ⅰ度滑脱 c:术前横断面MRI示椎管狭窄,硬膜囊受压 d、e:术中置入椎体螺钉、融合器及连接钛棒 f、g:术后2 d正侧位X线片示滑脱椎体复位,内固定及融合器位置良好 h、i:术后2周横断面及矢状面MRI示椎管减压充分 j、k:术后2年CT及三维重建示融合器与上下椎体骨性融合 Male, 42 years old, L4/L5 Meyerding degreeⅠ spondylolisthesis a, b: Preoperative anteroposterior and lateral roentgenographs show L4 degreeⅠ spondylolisthesis c: Preoperative transverse MRI shows spinal stenosis and compression of dural sac d, e: Intraoperative placement of vertebral screws, fusion cages and connecting titanium rods f, g: Anteroposterior and lateral roentgenographs at postoperative 2 d show satisfactory reduction and good position of cage and internal fixation h, i: Transverse and sagittal MRIs at postoperative 2 weeks show sufficient decompression j, k: CT and three-dimensional at postoperative 2 years show bony fusion between fusion cage and upper and lower vertebral bodies |
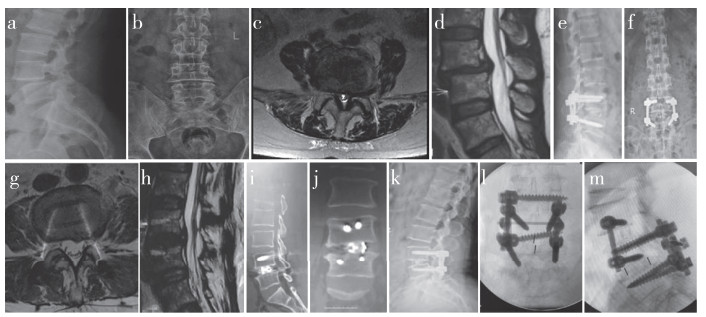
|
图 3 MIS-TLIF组典型病例影像学资料 Fig. 3 Imaging data of a typical case in MIS-TLIF group 男,45岁,L4/L5节段MeyerdingⅠ度滑脱 a、b:术前正侧位X线片示L4Ⅰ度滑脱 c、d:术前横断面和矢状面MRI示椎管狭窄,硬膜囊受压 e、f:术后2 d正侧位X线片示滑脱椎体复位,内固定及融合器位置良好 g、h:术后2周横断面和矢状面MRI示椎管减压充分 i、j:术后2年CT示融合器与上下椎体骨性融合 k:术后3年侧位X线片示L3/L4节段滑脱 l、m:L3/L4节段行OLIF Male, 45 years old, L4/L5 Meyerding degreeⅠ spondylolisthesis a, b: Preoperative anteroposterior and lateral roentgenographs show L4 degreeⅠ spondylolisthesis c, d: Preoperative transverse and sagittal MRIs show spinal stenosis and compression of dural sac e, f: Anteroposterior and lateral roentgenographs at postoperative 2 d show satisfactory reduction and good position of cage and internal fixation g, h: Transverse and sagittal MRIs at postoperative 2 weeks show sufficient decompression i, j: CTs at postoperative 2 years show bony fusion between fusion cage and upper and lower vertebral bodies k: Lateral roentgenograph at postoperative 3 years shows L3/L4 spondylolisthesis l, m: Revision surgery with OLIF on L3/L4 |
后路腰椎融合术存在椎旁肌广泛损伤、硬膜撕裂等风险,且术后椎间孔高度/面积、腰椎矢状面参数恢复不佳,大大影响手术效果[8]。前路间接减压与后路直接减压相比,具有创伤小、手术时间短、患者术后恢复快等优点[9]。然而,前路手术因解剖结构复杂,常常存在重要血管损伤、逆行性射精、腰丛神经损伤、腹腔脏器损伤、输尿管损伤(尿潴留)等并发症[10-11]。本研究结果显示,OLIF组术后1例出现术侧腰大肌无力合并大腿外侧麻木,1例左侧交感干神经损伤(4.5%,4.5%),发生率与既往荟萃分析[12]结果相仿(3.6%,2.8%)。Mehren等[13]采用OLIF治疗812例患者,其中腰丛神经损伤的发生率为0.37%(3/812),未发生交感干损伤。另一回顾性研究[14]报告腰大肌/腰丛神经损伤(4/179,2.2%)和交感干损伤(3/179,1.7%)的发生率更低。张建锋等[12]的研究称交感神经链位于椎体前1/3处,因管道置入空间有限(特别是L4/L5节段),所以本研究组建议,在放置管道时应斜置并将交感神经链保护性向前推移,使撑开器置于交感神经链的后方,从而降低交感干损伤率。早前研究[15]报道,腰椎前路手术中动脉损伤发生率为0.3%~2.4%,然而,OLIF主要累及节段动脉,多可通过术中止血处理解决[16]。本研究OLIF组1例发生节段动脉损伤,术中给予双极电凝配合明胶海绵片填塞后出血被迅速控制。本研究中MIS-TLIF组发生术中硬膜撕裂1例,术后神经根性症状(直接减压相关)2例;随访期间遗留顽固性腰背部疼痛(后方复合体损伤相关)1例,而OLIF组未发生上述并发症,说明OLIF治疗单节段轻中度腰椎滑脱安全有效,且可避免后路手术相关并发症的发生。但一些特殊情况仍建议采用MIS-TLIF治疗:①致压物来自后方,黄韧带严重骨化、关节突增生内聚、骨性侧隐窝狭窄等继发的严重椎管狭窄;②合并神经根性症状或马尾神经综合征,需要进行神经根或硬膜囊探查、减压;③合并严重腰椎椎间盘突出,髓核游离甚至与硬膜囊粘连,须进一步探查减压;④高髂嵴L5/S1节段退行性滑脱。
本研究结果显示,OLIF组手术时间和术中出血量明显少于MIS-TLIF组,与之前的研究结果[17]一致,考虑原因为间接减压未破坏后方复合体进入椎管。本研究结果还显示,OLIF组住院时间比MIS-TLIF组短,分析原因为OLIF术中保留了椎旁肌和腰大肌,且未破坏后方关节突关节,患者术后恢复快,可早期行功能锻炼[18]。本研究中OLIF组术后1周VAS评分和ODI均优于MIS-TLIF组,术后1个月、6个月及末次随访时2组VAS评分及ODI大致相仿,说明OLIF有助于患者早期功能恢复,但长期随访功能评分二者相当。
有研究[19]报道,MIS-TLIF对LL矫正无效。还有研究[20]发现,MIS-TLIF对LL的影响取决于后柱压缩的矫正程度。本研究结果显示,OLIF在恢复LL、手术节段Cobb角、DH及FA方面更有优势,考虑与使用的融合器型号有关,MIS-TLIF组融合器长24~30 mm、宽12~14 mm、高10~12 mm,OLIF组融合器长45~55 mm、宽18~22 mm、高10~14 mm。唐冲等[21]的一项荟萃分析结论得出,OLIF可有效撑开病变椎间隙,增加硬膜CSA,扩大神经根管,解除神经根及硬膜压迫,同时改善腰椎整体及节段前凸,恢复腰椎曲度,最终达到解除临床症状、改善生活质量的目的。本研究中2组末次随访椎管CSA矫正值与其报道一致。郑晓青等[22]回顾性分析采用单节段OLIF治疗的49例患者,发现融合器越宽术后影像学参数矫正效果越好,但融合器高度越高越容易发生终板损伤,且多见于上终板。本研究发生融合器下沉病例,可能与术中终板的处理、术中自体颗粒骨回植及融合器放置位置有关,这将是本研究未来关注的一个方向,且椎体螺钉固定是否对治疗结果产生影响也需进一步研究明确。
综上,OLIF作为一项脊柱外科新兴微创手术,具有创伤小、患者术后恢复快、疗效好、并发症少等优势,在严格把握适应证的条件下,值得临床进一步推广。但本研究属于单中心回顾性病例研究,样本量较少,随访时间跨度相对较大,在获取随访信息时可能存在信息误差。且OLIF技术难度较高,术者学习曲线陡峭,且须严格掌握手术适应证,尽量降低术中神经及血管损伤的风险。
| [1] |
Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment[J]. Neurosurg Clin N Am, 2019, 30(3): 299-304. DOI:10.1016/j.nec.2019.02.003 |
| [2] |
Kim JS, Jung B, Lee SH. Instrumented minimally invasive spinaltransforaminal lumbar interbody fusion(MIS-TLIF): minimum 5-year follow-up with clinical and radiologic outcomes[J]. Clin Spine Surg, 2018, 31(6): E302-E309. DOI:10.1097/BSD.0b013e31827415cd |
| [3] |
Silvestre C, Mac-Thiong JM, Hilmi R, et al. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients[J]. Asian Spine J, 2012, 6(2): 89-97. DOI:10.4184/asj.2012.6.2.89 |
| [4] |
王吉莹, 周志杰, 范顺武, 等. 斜外侧椎间融合术治疗腰椎退行性疾病的早期并发症分析[J]. 中华骨科杂志, 2017, 37(16): 1006-1013. |
| [5] |
陈斌彬, 毛克亚, 韩振川, 等. 微创经椎间孔入路腰椎椎间融合术治疗腰椎滑脱症的中短期随访[J]. 脊柱外科杂志, 2019, 17(5): 297-302. |
| [6] |
Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127-1131. |
| [7] |
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire[J]. Physiotherapy, 1980, 66(8): 271-273. |
| [8] |
Goz V, Weinreb JH, Schwab F, et al. Comparison of complications, costs, and length of stay of three different lumbar interbodyfusion techniques: an analysis of the Nationwide Inpatient Sample database[J]. Spine J, 2014, 14(9): 2019-2027. DOI:10.1016/j.spinee.2013.11.050 |
| [9] |
Nakashima H, Kanemura T, Satake K, et al. Comparative radiographic outcomes of lateral and posterior lumbar interbody fusion in the treatment of degenerative lumbar kyphosis[J]. Asian Spine J, 2019, 13(3): 395-402. DOI:10.31616/asj.2018.0204 |
| [10] |
Bateman DK, Millhouse PW, Shahi N, et al. Anterior lumbar spine surgery: a systematic review and meta analysis of associated complications[J]. Spine J, 2015, 15(5): 1118-1132. DOI:10.1016/j.spinee.2015.02.040 |
| [11] |
陈漩, 李野, 赵海洋, 等. 微创经椎间孔、极外侧、斜外侧入路腰椎椎间融合术的适应证及并发症研究进展[J]. 脊柱外科杂志, 2020, 18(6): 419-424. |
| [12] |
张建锋, 范顺武, 方向前, 等. 斜外侧椎间融合术在单节段腰椎间盘退行性疾病中的应用[J]. 中华骨科杂志, 2017, 37(2): 80-88. |
| [13] |
Mehren C, Mayer HM, Zandanell C, et al. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications[J]. Clin Orthop Relat Res, 2016, 474(9): 2020-2027. DOI:10.1007/s11999-016-4883-3 |
| [14] |
Quillo-Olvera J, Lin GX, Jo HJ, et al. Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies[J]. Ann Transl Med, 2018, 6(6): 101. DOI:10.21037/atm.2018.01.22 |
| [15] |
Malham GM, Parker RM, Blecher CM, et al. Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months[J]. Glob Spine J, 2016, 6(5): 472-481. DOI:10.1055/s-0035-1569055 |
| [16] |
Phan K, Maharaj M, Assem Y, et al. Review of early clinical results and complications associated with oblique lumbar interbody fusion(OLIF)[J]. J Clin Neurosci, 2016, 31: 23-29. DOI:10.1016/j.jocn.2016.02.030 |
| [17] |
Sembrano JN, Tohmeh A, Isaacs R, et al. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: PartⅠ: clinical findings[J]. Spine(Phila Pa 1976), 2016, 41(8): S123-S132. |
| [18] |
Liu J, Feng H. Oblique lateral interbody fusion(OLIF) with supplemental anterolateral screw and rod instrumentation: a preliminary clinical study[J]. World Neurosurg, 2020, 134: e944-e950. |
| [19] |
轩安武, 谢雁春, 张猛, 等. 微创经椎间孔入路与极外侧入路腰椎椎间融合术治疗短节段腰椎退行性疾病的近期疗效比较[J]. 脊柱外科杂志, 2019, 17(2): 84-89. |
| [20] |
Carlson BB, Saville P, Dowdell J, et al. Restoration of lumbar lordosis after minimally invasive transforaminal lumbar interbody fusion: a systematic review[J]. Spine J, 2019, 19(5): 951-958. |
| [21] |
唐冲, 刘正, 吴四军, 等. 斜外侧腰椎椎间融合术治疗腰椎退行性疾病疗效的meta分析[J]. 中华骨科杂志, 2019, 39(21): 1320-1332. |
| [22] |
郑晓青, 尹东, 顾宏林, 等. 斜向腰椎融合中不同型号椎间融合器与椎体终板损伤的关系[J]. 中国组织工程研究, 2019, 23(34): 5418-5424. |
 2023, Vol.21
2023, Vol.21  Issue(1): 26-31
Issue(1): 26-31


