2. 海军军医大学长征医院骨科, 上海 200003
2. Department of Orthopedics, Changzheng Hospital, Naval Medical University, Shanghai 200003, China
腰椎在脊柱中活动范围广,承受压力大,特别是下腰椎,最易发生退行性变导致的腰椎椎间盘突出症(LDH),其中以L4/L5及L5/S1节段最为常见[1-2]。随着脊柱微创技术的迅速发展,经椎板间和椎间孔入路是目前内窥镜技术的主要入路[3],椎弓根直接或间接参与组成这2个通道,是术中的重要解剖参考标志之一。既往研究[1-2, 4-5]对椎弓根、椎板间和椎间孔的解剖结构及形态特征有了一定认识,但缺乏对椎弓根形态(长度与角度)与相应节段椎板间及椎间孔大小之间相关性的研究。基于此,本研究主要通过对LDH患者L4~S1节段的影像学测量,研究和探讨椎弓根长度、角度与相应节段椎板间及椎间孔大小的相关性,进一步认识人脊柱的形态结构特点,为临床进行腰椎全内窥镜下手术提供相关的解剖学依据和术前预判,减少术中及术后并发症的发生,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①年龄18~55岁;②影像学确诊为L4/L5或L5/S1节段LDH;③腰椎X线片和CT影像学资料完整。排除标准:①影像学资料提示L4/L5或L5/S1节段椎弓根及椎板破坏,如骨折等;②合并腰椎滑脱、畸形、肿瘤、感染等。按照上述标准,纳入2020年1月—2022年6月海军军医大学长征医院收治的50例L4/L5或L5/S1节段LDH患者作为研究组,并选取同时期50名健康成年志愿者作为对照组。其中,研究组男34例、女16例,年龄为(40.94±9.61)岁,体质量指数(BMI)为(25.04±3.02)kg/m2;对照组男24例、女26例,年龄为(36.16±10.55)岁,BMI为(23.58±3.51)kg/m2。2组性别、年龄和BMI等一般资料差异无统计学意义(P>0.05),具有可比性。本研究经海军军医大学长征医院伦理委员会审核备案。
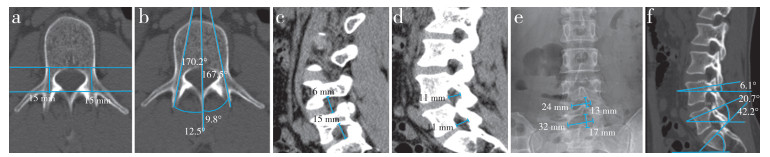
1.2 影像学指标测量所有患者接受腰椎正侧位X线(DitalDiagnost,飞利浦,荷兰)和CT平扫(Brilliance,32层,管电流220 mA,管电压120 kV,层厚1.0 mm,飞利浦,荷兰)及三维重建(层厚1.0 mm,间距0.5 mm)检查。在腰椎正侧位X线片上测量L4/L5和L5/S1椎板间隙的最大高度和宽度,在CT上测量椎弓根长度和角度、椎间孔最小高度和宽度,以上指标均采用IMPAX6.3.4095—AGFA系统测量。为减少测量误差,每项指标均由3位脊柱外科医师独立测量,取平均值,同一椎体左右两侧再取平均值,记录并作为测量值。参考文献[2, 4-10]的方法,测量左右椎弓根长度(图 1a)、椎弓根外展角(图 1b)、椎间孔高度与宽度(图 1c、d)、椎板间高度与宽度(图 1e)、椎弓根头倾角(图 1f)。
|
图 1 影像学指标测量 Fig. 1 Measurement of imaging indicators a:椎弓根长度 b:椎弓根外展角 c、d:椎间孔高度与宽度 e:椎板间高度与宽度 f:椎弓根头倾角 a: Pedicle length b: Pedicle abduction angle c, d: Height and width of foramen e: Height and width of interlaminar f: Pedicle head inclination angle |
采用SPSS 21.0软件对数据进行统计分析。采用Shapiro-Wilk检验评估数据分布,用Levine检验评估方差齐性,如果呈正态分布,以x±s表示,采用t检验;如果呈非正态分布,采用中位数(下四分位数,上四分位数)表示,采用Mann-Whitney U检验;以P<0.05为差异有统计学意义。采用Pearson相关系数检验评价参数关系;采用逐步多元线性回归的多元相关性来确定相关变量对椎间孔及椎板间大小的独立影响。
2 结果2组L4~S1椎弓根长度、L4/L5及L5/S1节段椎间孔和椎板间高度差异均无统计学意义(P>0.05,表 1)。研究组S1椎弓根外展角小于对照组;研究组L4椎弓根头倾角高于对照组,S1椎弓根头倾角低于对照组;研究组L4与L5、L5与S1椎弓根头倾角差值低于对照组;研究组L4/L5和L5/S1节段椎间孔宽度、椎板间宽度小于对照组;以上指标差异均有统计学意义(P<0.05,表 1)。
|
|
表 1 2组影像学指标比较 Tab. 1 Comparison of imaging indicators between 2 groups |
进一步将各指标与L4/L5和L5/S1节段的椎间孔及椎板间高度和宽度进行Pearson相关分析,年龄与椎板间高度和宽度及椎间孔高度呈负相关,椎弓根外展角与椎板间宽度呈正相关,椎弓根长度与椎间孔宽度呈正相关,相邻腰椎椎弓根头倾角差值与椎间孔宽度呈正相关,椎板间宽度与椎间孔宽度呈正相关(表 2)。
|
|
表 2 椎间孔及椎板间高度和宽度的Pearson相关分析 Tab. 2 Pearson correlation analysis of height and width of foramen and interlaminae |
再对每个节段进行多重线性回归建模,患者的年龄、椎弓根长度及角度与椎间孔及椎板间大小独立相关,L5、S1椎弓根外展角与椎板间宽度显著正相关(P<0.05),L5椎弓根头倾角与L4/L5及L5/S1椎间孔高度显著负相关(P<0.05);相邻腰椎椎弓根头倾角差值与椎间孔宽度显著正相关(P<0.05)。得到8个拟合直线。
L4/L5椎间孔高度(mm)=18.016-0.048×年龄(岁)-0.094×L5椎弓根头倾角(°)+0.043×体质量(kg);(R2=0.225,P<0.05)。
L4/L5椎间孔宽度(mm)=1.383+0.387×L5椎弓根长度(mm)+0.101×L4与L5椎弓根头倾角差值(°)+0.099×L4/L5椎板间宽度(mm);(R2=0.254,P<0.05)。
L4/L5椎板间高度(mm)=17.42-0.082×年龄(岁);(R2=0.10,P<0.05)。
L4/L5椎板间宽度(mm)=0.513×L5椎弓根外展角(°)+10.254×身高(cm)+0.556×L4/L5椎间孔宽度(mm)-10.431;(R2=0.461,P<0.05)。
L5/S1椎间孔高度(mm)=10.103-0.097×L5椎弓根头倾角(°)+0.035×体质量(kg)+0.203×L5/S1椎板间高度(mm);(R2=0.225,P<0.05)。
L5/S1椎间孔宽度(mm)=0.332×L5椎弓根长度(mm)+0.064×L5与S1椎弓根头倾角差值(°)+0.139×L5/S1椎板间宽度(°);(R2=0.254,P<0.05)。
L5/S1椎板间高度(mm)= 12.12-0.05×年龄(岁)+0.330×L5/S1椎间孔高度(°);(R2=0.078,P<0.05)。
L5/S1椎板间宽度(mm)=14.712-0.100×年龄(岁)+0.330×S1椎弓根外展角(°)+0.715×L5/S1椎间孔宽度(°);(R2=0.327,P<0.05)。
3 讨论近年来,内窥镜下腰椎融合内固定术在国内发展迅速,经椎板间入路和经椎间孔入路是目前主要的术式。本研究通过对椎弓根长度和角度的分析,来预测椎间孔和椎板间大小及手术难易程度,指导临床入路选择,达到优化手术方式、减少手术并发症的目的。腰椎内窥镜下手术均可通过椎板或关节突成形,使工作通道顺利到达靶点[11]。张海峰等[5]指出,术前椎间孔和椎板间的测量对研判手术切除骨量具有重要意义。术前根据椎弓根、椎板间和椎间孔形态结构选择不同的手术入路,经椎板间或椎间孔暴露椎间盘过程中,内窥镜下常以下位椎体椎弓根为参考点,通过切除上下关节突后的Kambin三角[3, 12-13],贴近并参照椎弓根上缘外展及头倾角和方向置入融合器,此方法可远离神经行走根和出口根,避免意外损伤硬膜或神经根,将融合器安全置入椎间隙偏中线的位置,学习曲线相对平缓,更易掌握。
本研究结果显示,脊柱退行性变随着年龄增长逐渐加重,椎板间及椎间孔高度和宽度均变小,身高与椎弓根角度和长度无显著相关性,与乔风雷等[4]、张海峰等[5]和Yan等[14]的研究结论部分一致。目前被广泛接受的椎间孔解剖结构是指一个具有上、下椎弓根边界的沙漏形椎间室[15],腰椎CT三维重建可见L4/L5、L5/S1椎间孔的高度和宽度递减[4],与本研究测量结果一致。L5椎弓根头倾角与L4/L5和L5/S1椎间孔高度呈负相关,在极度弯腰时椎间孔高度增大[16-17]。相邻椎弓根头倾角差值与椎间孔宽度呈正相关,腰椎退行性变加重、生理曲度减小时,椎间孔宽度会相应减小,导致椎间孔狭窄,出口神经根受压,引起腰腿痛。腰椎椎弓根垂直于椎体后缘切线时椎间孔狭窄部最宽。L4至S1椎弓根外展角逐渐增大,椎间孔方向由侧方移行至斜前方,在椎间孔建立通道时,穿刺难度增加,手术皮肤开口离棘突中线距离也需增加,目的是使工作通道顺利到达靶点,不被关节突阻挡,切除最少的骨质,避免破坏腰椎稳定性,因此,L4/L5节段病变时选择椎间孔入路更有优势。本研究结果进一步显示,L5/S1椎板间高度和宽度均大于L4/L5节段,高度与宽度的乘积也大于L4/L5节段,因此,L5/S1节段病变时选择椎板间入路相对更安全,与别业俊等[2]和张海峰等[5]的研究结果一致。本研究组在测量过程中发现,L4/L5到L5/S1椎间孔高度(即相邻椎弓根距离)递减,椎弓根矢状位角度差递增,相对应椎板弧线距离递减,但椎板间隙高度却递增,考虑与L5椎板高度减小有关[1-2, 5]。另外,椎弓根头倾角逐渐增大,椎弓根与相连的椎板夹角逐渐增加[18],椎板头倾角度越大,越容易出现“百叶窗”现象,导致椎板间隙越大,这也可解释椎间孔高度递减而椎板间高度递增的部分原因。
本研究的局限性:①测量主要基于影像学资料,而患者体位存在不一致的可能性,矢状面、冠状面和横断面在影像学资料上可能出现扭曲,导致最窄区测量误差[7]。②所收集的影像学资料均来自同一研究中心,有待在多中心人群中验证其准确性。③样本量较小,后续研究有待扩大样本量增强说服力。
综上,椎板间及椎间孔高度和宽度随着患者年龄增长而变小,椎板间宽度随着L5、S1椎弓根外展角度增大而变大;L5椎弓根头倾角越大,相邻椎间孔高度越小;相邻椎体椎弓根头倾角差值增加,椎间孔宽度增大;椎弓根角度和长度影响椎板间及椎间孔的大小,影响手术难度和手术方式选择。
| [1] |
Tao S, Jin L, Hou Z, et al. A new radiographic feature of lower lumbar disc herniation in young patients[J]. Int Orthop, 2018, 42(3): 583-586. DOI:10.1007/s00264-017-3723-8 |
| [2] |
别业俊, 常晓涛, 徐燕笑, 等. 腰椎椎板间隙的放射解剖学测量及分型[J]. 中国临床解剖学杂志, 2018, 36(4): 383-386. |
| [3] |
柯荣军, 夏新, 刘方刚, 等. 经椎板间入路经皮内窥镜下椎间盘切除术治疗L5/S1椎间盘突出症术中应用不同麻醉方式对术后疗效的影响[J]. 脊柱外科杂志, 2019, 17(4): 248-251. DOI:10.3969/j.issn.1672-2957.2019.04.006 |
| [4] |
乔风雷, 朱斌, 马军, 等. 螺旋CT容积再现法腰椎椎间孔测量探讨[J]. 中国临床医学影像杂志, 2015, 26(11): 820-822. |
| [5] |
张海峰, 占新华, 傅泽泽, 等. 下腰椎板间隙的影像解剖学测量及其临床意义[J]. 中国临床解剖学杂志, 2021, 39(1): 37-40. |
| [6] |
Dzierzanowski J, Skotarczyk M, Baczkowska-Waliszewska Z, et al. Morphometric analysis of the lumbar vertebrae concerning the optimal screw selection for transpedicular stabilization[J]. Adv Exp Med Biol, 2019, 1133: 83-96. |
| [7] |
Tang C, Liao YH, Tang Q, et al. What is the difference in pedicle morphology of the fifth lumbar vertebra between isthmic and degenerative L5 - S1 spondylolisthesis? An anatomic study of 328 patients via multi-slice spiral computed tomography[J]. Eur Spine J, 2021(30): 2301-2310. |
| [8] |
Wang Y, Cai Y, Xu Y, et al. Anatomic morphological study of thoracolumbar foramen in normal adults[J]. Folia Morphol(Warsz), 2021(80): 675-682. |
| [9] |
甄瑞鑫, 李玉波, 宋有鑫, 等. 椎下切迹的测量分析对经椎间孔入路的脊柱内镜技术的意义[J]. 实用骨科杂志, 2017, 23(10): 879-883. |
| [10] |
Xu WX, Xu B, Ding WG, et al. Feasibility of anterior pedicle screw fixation in lumbosacral spine: a radiographic and cadaveric study[J]. Ann Transl Med, 2021(9): 968. |
| [11] |
王洪伟, 李铠湘, 王青云, 等. 基于MRN技术的下腰椎Kambin三角的解剖学研究[J]. 中国临床解剖学杂志, 2022, 40(3): 267-270. |
| [12] |
李亚伟, 王冰, 吕国华, 等. 椎板间隙成形技术在经椎板间入路完全内窥镜下手术治疗L4/5椎间盘突出症中的应用[J]. 中国脊柱脊髓杂志, 2017, 27(3): 193-199. |
| [13] |
谭洪栋, 许良. 简易穿刺定位法在经椎间孔入路经皮内窥镜下腰椎椎间盘切除术中的临床应用[J]. 脊柱外科杂志, 2021, 19(5): 308-312. DOI:10.3969/j.issn.1672-2957.2021.05.004 |
| [14] |
Yan S, Zhang Y, Wang K, et al. Three-dimensional morphological characteristics of lower lumbar intervertebral foramen with age[J]. Biomed Res Int, 2018, 8157061. |
| [15] |
Shim DW, Lee BH, Seo J, et al. Efficacy of computed tomography in prediction of operability of L5/S1 foraminal stenosis using region of interest: a STROBE-compliant retrospective study[J]. Medicine(Baltimore), 2019, 98(42): e17422. |
| [16] |
冯宇鹏, 李辉, 李云庆. 腰椎间孔的应用解剖[J]. 中国微侵袭神经外科杂志, 2019, 24(11): 522-524. |
| [17] |
张黎明, 杨晋才. 腰椎间孔区解剖结构特点与临床应用研究进展[J]. 实用骨科杂志, 2020, 26(1): 44-47. |
| [18] |
王洪例, 姜建元, 吕飞舟, 等. 腰椎椎板-椎弓根解剖参数的影像学测量及临床意义[J]. 中华骨与关节外科杂志, 2015, 8(6): 467-471. |
 2024, Vol.22
2024, Vol.22  Issue(1): 21-26
Issue(1): 21-26


