2. 盐城市第三人民医院骨科,盐城 224008
2. Department of Orthopaedics, Yancheng Third People's Hospital, Yancheng 224008, Jiangsu, China
无骨折脱位型颈椎脊髓损伤(SCI)是一种特殊类型SCI,影像学检查未见颈椎骨折或脱位,而患者却出现明显SCI症状与体征[1]。一般认为这种损伤的产生与颈椎退行性变及颈椎椎管狭窄等病理基础有关[2]。也有学者[3]认为,急性外伤性椎间盘突出也是该损伤中造成脊髓受压的重要因素。随着人口老龄化,此类损伤的发生率呈上升趋势[4]。MRI检查中常表现为损伤平面T2WI高信号改变,而高信号的存在高度提示髓内神经细胞受到实质损伤,且术后神经功能的恢复程度与T2WI高信号的改善程度呈正相关[5-6]。有学者[7]认为,伴有T2WI高信号改变的颈椎SCI应尽早行手术治疗,且前路手术疗效优于后路,但采用何种术式仍存争议[8]。本研究比较了2014年1月—2017年1月海安市人民医院采用颈椎后路椎管扩大椎板成形术联合单侧椎弓根螺钉短节段内固定术与颈椎前路减压植骨融合内固定术治疗的MRI T2WI高信号无骨折脱位型SCI患者临床疗效,现报告如下。
1 资料与方法 1.1 一般资料纳入标准:①下颈椎损伤分类(SLIC)评分[9]≥4分的下颈椎损伤;②术前MRI T2WI高信号改变;③无颈椎椎体骨折或脱位影像学表现;④受伤到接受手术治疗时间 < 72 h。排除标准:①存在颈椎结核、畸形、肿瘤、感染及影响骨代谢的疾病;②术前存在胸椎、腰椎等影响下肢功能的疾病;③有颅脑损伤、血气胸等全身其他部位损伤;④既往有颈椎手术史。根据上述标准,纳入MRI T2WI高信号无骨折脱位颈椎SCI患者89例,其中摔伤27例,重物砸伤10例,交通伤41例,坠落伤11例。其中43例采用颈椎后路椎管扩大椎板成形术联合单侧椎弓根螺钉短节段内固定术治疗(后路组),46例采用颈椎前路减压植骨融合内固定术治疗(前路组)。2组患者术前一般资料差异无统计学意义(P > 0.05,表 1),具有可比性。
|
|
表 1 2组患者一般资料 Tab. 1 General information of 2 groups |
患者全身麻醉后,留置导尿管,俯卧于石膏床上,常规手术区消毒铺巾。做颈部后正中纵向切口,切开皮肤约12 cm,分离椎旁肌,开口、钻道、探深后,分别在脊髓高信号节段拟开门侧上、下椎弓根各置入1枚椎弓根螺钉,预弯钛棒,固定于钉尾并锁紧。透视确定螺钉方向、位置满意。用磨钻在减压节段椎板两侧分别开槽,门轴侧开槽深度至内侧皮质骨,开门侧(即椎弓根螺钉侧)开槽深度至椎管,使用磨钻及枪钳去除椎板及黄韧带,使椎板完全游离,依次提拉游离的椎板,使其开口到合适宽度后,置入微型Arch钛板,开口钻孔,螺钉固定。硬膜囊减压后脊髓慢慢变粗,恢复搏动,检查确认减压上、下缘椎板对脊髓无卡压,硬膜囊膨起满意。止血、放置引流管,逐层缝合。
1.2.2 前路组患者全身麻醉后取仰卧位,常规消毒铺巾。做颈前右侧横切口,由颈血管鞘和内脏鞘之间钝性分离进入椎前间隙,显露手术节段椎体及两侧椎间盘,髓核钳去除发生退行性变的椎间盘,刮除终板软骨,咬骨钳咬除椎体大部,磨钻磨薄椎体后壁及后缘骨赘,枪钳咬除突入椎管内的髓核组织。见到受压脊髓逐渐恢复正常形态后取合适长度植有碎骨的钛网填入骨槽中,适当锤紧。若存在其他节段椎间盘突出,相同方法处理椎间隙并置入合适大小椎间融合器。取合适长度钛板固定于椎体前壁,拧入螺钉并锁紧。止血、放置引流管,逐层缝合。
1.3 疗效评估记录2组手术时间、术中出血量,手术前后颈椎活动度(ROM)、脊髓横截面积、椎管面积残余率、髓内高信号强度比值,手术前后采用日本骨科学会(JOA)评分[10]和颈椎功能障碍指数(NDI)[11]评价疗效。
髓内高信号强度比值计算方法采用Uchida等[5]报道的方法,采用Image J软件对MRI T2WI进行分析。在信号最显著处取0.1 cm2的区域测量其光密度值(IOD1),在同一矢状面取C7/T1水平正常髓内信号部位0.1 cm2的区域测量IOD2,髓内高信号强度比值=IOD1/IOD2。采用本院IMPAX系统工具测量手术前后MRI高信号水平的脊髓横截面积平均值和CT上椎管横截面积平均值,分别取高信号上缘、高信号中央及高信号下缘的脊髓和椎管横截面积,计算平均值。椎管面积残余率(%)=椎管实际面积/椎管发育性面积×100%。JOA评分改善率(%)=(末次随访JOA评分-术前JOA评分)/(17分-术前JOA评分)×100%。NDI改善率(%)=(术前NDI-术后NDI)/术前NDI×100%。
1.4 统计学处理采用SPSS 23.0软件对数据进行统计分析。符合正态分布的计量资料以x±s表示,采用Student’s T-Test进行假设检验;计数资料以百分比或率表示,采用Wilcoxon Signed-Rank Test进行假设检验;采用χ2检验分析分类资料的显著性;以P < 0.05为差异有统计学意义。
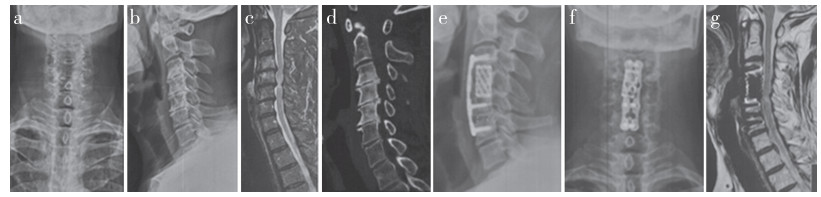
2 结果所有手术顺利完成,所有患者随访时间 > 24个月。2组手术时间、术中出血量差异无统计学意义(P > 0.05,表 2)。术后6个月和术后2年,2组髓内高信号强度比值、脊髓横截面积、椎管面积残余率、JOA评分和NDI较术前显著改善,且后路组术后6个月和术后2年颈椎ROM和椎管面积残余率、术后2年NDI和NDI改善率优于前路组,差异均有统计学意义(P < 0.05,表 2)。2组典型病例影像学资料见图 1、2。
|
|
表 2 手术及疗效相关统计数据 Tab. 2 Statistical data related to surgery and efficacy |

|
图 1 后路组典型病例影像学资料 Fig. 1 Imaging data of a typical case in posterior group a ~ d:术前影像学资料示颈椎SCI e、f:术后即刻正侧位X线片示内固定位置良好 g:术后2年MRI示颈椎脊髓无明显压迫 a-d: Preoperative imaging data show cervical SCI e, f: Anteroposterior and lateral roentgenographs at immediate postoperative show internal fixation in good position g: MRI at postoperative 2 years shows no obvious compression of cervical spinal cord |
|
图 2 前路组典型病例影像学资料 Fig. 2 Imaging data of a typical case in anterior group a ~ d:术前影像学资料示颈椎SCI e、f:术后2年正侧位X线片示内固定位置良好 g:术后2年MRI示颈椎脊髓无明显压迫 a-d: Preoperative imaging data show cervical SCI e, f: Anteroposterior and lateral roentgenographs at postoperative 2 years show internal fixation in good position g: MRI at postoperative 2 years shows no obvious compression of cervical spinal cord |
无骨折脱位型颈椎SCI通常是存在发育性颈椎椎管狭窄(Pavlov比值< 0.75)、后纵韧带骨化及颈椎退行性变等病理基础的情况下,结合一定的外力作用,在无骨性结构损伤的前提下发生的SCI,常见于颈椎过伸伤,导致脊髓褶皱挤压,从而产生以颈椎脊髓中央管为中心的损伤,在X线片上并不能观察到明显的椎体、关节的破坏移位[1]。MRI对无骨折脱位型颈椎SCI有较好的诊断价值,可清晰显示颈椎脊髓及其周围软组织,同时,MRI也具有较好的预后评估价值[12]。Suri等[13]发现,无论患者采用前路手术还是后路手术治疗,MRI T2WI高信号的出现均提示较差的神经功能预后。Ikegami等[14]的研究发现,术后1年随访时脊髓高信号较术前好转的患者其神经功能也获得更好的恢复。本研究结果提示,2种术式均可有效改善患者的脊髓高信号及神经功能,且疗效相当。
对无骨折脱位型颈椎SCI的治疗方式目前仍存在争议[15],有学者建议采用非手术治疗,Kawano等[4]的研究发现,接受非手术治疗和手术治疗的患者预后无明显差异。然而大部分学者认为,非手术治疗效果有限,难以改善神经功能,可能出现SCI加重的情况,因为脊髓的实际压迫因素并未解除,仅改善脊髓微循环并不能实现脊髓功能的恢复,解除压迫必须依赖于手术治疗[16]。另有研究[17]发现,急性颈椎SCI后早期手术可获得更好的神经功能恢复,同时可以减少并发症的发生。对于SLIC评分≥4分的下颈椎损伤患者推荐采用手术治疗,其中脊髓持续受压一项的分值就为4分,可见SCI后及时解除压迫是必要的[18]。本研究纳入的患者SLIC评分均≥4分,术后2组患者JOA评分及NDI均显著改善,进一步证实了手术减压治疗无骨折脱位型颈椎SCI的有效性。
治疗颈椎SCI的常用术式有2种,一是颈椎前路减压植骨融合内固定术,二是后路单开门椎管扩大椎板成形术[19]。前路手术的优势在于可以直接去除病灶减压、恢复颈椎正常生理曲度、维持损伤节段的稳定性,减压直观、彻底。Liu等[20]、Joaquim等[21]、王建杰等[22]的研究发现,颈椎前路手术JOA评分改善情况优于后路手术,但术后吞咽困难、发音困难等并发症的发生率较高。另外,由于颈椎前部结构复杂,前路手术还容易发生食管/气管损伤、脑脊液漏、医源性SCI、血肿和内置物移位等并发症[23]。传统后路单开门椎管扩大椎板成形术同样可以实现早期减压的目的,但由于破坏了后方椎板韧带结构,一定程度上会造成椎间结构不稳,从而产生轴性疼痛,同时可能加重高信号区域的SCI[24-25]。相较于传统的颈椎后路单开门椎管扩大椎板成形术,本研究采用颈椎后路椎管扩大椎板成形术联合单侧椎弓根螺钉短节段内固定术,在保证有效扩大椎管容积的前提下,采用单侧椎弓根螺钉短节段固定高信号区域,更好地保证高信号区域椎体结构的稳定性,为脊髓的恢复提供稳定的空间环境,防止因颈椎运动使SCI加重。Chen等[26]采用后路联合手术治疗伴有节段不稳的颈椎后纵韧带骨化症,并取得满意疗效。相较于前路手术,后路联合手术只进行短节段椎弓根螺钉内固定,不破坏椎间盘结构,同时也未进行广泛融合,有助于保持颈椎ROM,这一点在本研究中得到证实。另外,由于门轴侧椎板韧带结构未受到破坏,仅对单侧(开门侧)椎弓根进行置钉,降低了置钉的手术风险,缩短了手术时间。
本研究结果显示,后路组术后短期内在改善患者生活质量方面作用弱于前路组,但在神经功能改善方面与前路组相似;从远期疗效来看,后路组具有更高的生活质量(NDI改善率)。笔者猜测,2种术式均可有效减压,使神经症状得以迅速改善,但后路手术造成颈椎后部肌肉韧带破坏,而前路手术损伤较小,因此,前路手术短期内具有更好的生活质量;与前路手术比较,后路联合手术使椎管容积增大更为显著,脊髓减压更为彻底,从而使脊髓血液灌注(尤其是脊髓微循环)更加充盈,为SCI的修复提供了更好的微环境,所以长期来看,后路联合手术在改善疼痛、提高生活质量方面效果更加显著。本研究测量2组患者术后脊髓横截面积并无差异,但后路组具有更大的椎管容积,而末次随访时2组JOA评分改善率差异无统计学意义,推测或许与样本量较小有关。
综上,本研究比较颈椎后路椎管扩大椎板成形术联合单侧椎弓根螺钉短节段内固定术与颈椎前路减压植骨融合内固定术治疗MRI T2WI高信号无骨折脱位型颈椎SCI的临床疗效,结果显示,2种术式均可有效治疗MRI T2WI高信号无骨折脱位型颈椎SCI,但颈椎后路椎管扩大椎板成形术联合单侧椎弓根螺钉短节段内固定术在术后远期生活质量改善方面更胜一筹,同时可更好地保留颈椎ROM。
| [1] |
Maeda T, Ueta T, Mori E, et al. Soft-tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury[J]. Spine(Phila Pa 1976), 2012, 37(25): E1560-E1566. DOI:10.1097/BRS.0b013e318272f345 |
| [2] |
Oichi T, Oshima Y, Okazaki R, et al. Preexisting severe cervical spinal cord compression is a significant risk factor for severe paralysis development in patients with traumatic cervical spinal cord injury without bone injury: a retrospective cohort study[J]. Eur Spine J, 2016, 25(1): 96-102. DOI:10.1007/s00586-015-4142-4 |
| [3] |
赵敦炎, 赵剑. 对急性创伤性无骨折脱位型颈髓损伤的病因探讨[J]. 中华骨科杂志, 1997, 17(5): 284-286. DOI:10.3760/j.issn:0253-2352.1997.05.002 |
| [4] |
Kawano O, Ueta T, Shiba K, et al. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study[J]. Spinal Cord, 2010, 48(7): 548-553. DOI:10.1038/sc.2009.179 |
| [5] |
Uchida K, Nakajima H, Takeura N, et al. Prognostic value of changes in spinal cord signal intensity on magnetic resonance imaging in patients with cervical compressive myelopathy[J]. Spine J, 2014, 14(8): 1601-1610. DOI:10.1016/j.spinee.2013.09.038 |
| [6] |
Vedantam A, Rajshekhar V. Does the type of T2-weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? A review[J]. Eur Spine J, 2013, 22(1): 96-106. DOI:10.1007/s00586-012-2483-9 |
| [7] |
Sun Q, Hu H, Zhang Y, et al. Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament?[J]. Eur Spine J, 2011, 20(9): 1466-1473. DOI:10.1007/s00586-011-1813-7 |
| [8] |
Wang J, Li J, Cai L. Effects of treatment of cervical spinal cord injury without fracture and dislocation in a medium-to long-term follow-up study[J]. World Neurosurg, 2018, 113: e515-e520. DOI:10.1016/j.wneu.2018.02.071 |
| [9] |
Vaccaro AR, Hulbert RJ, Patel AA, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex[J]. Spine(Phila Pa 1976), 2007, 32(21): 2365-2374. DOI:10.1097/BRS.0b013e3181557b92 |
| [10] |
Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890-1895. DOI:10.1097/00007632-200109010-00014 |
| [11] |
Vernon H, Mior S. The neck disability index: a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409-415. |
| [12] |
Matsushita A, Maeda T, Mori E, et al. Can the acute magnetic resonance imaging features reflect neurologic prognosis in patients with cervical spinal cord injury?[J]. Spine J, 2017, 17(9): 1319-1324. DOI:10.1016/j.spinee.2017.05.009 |
| [13] |
Suri A, Chabbra RP, Mehta VS, et al. Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy[J]. Spine J, 2003, 3(1): 33-45. DOI:10.1016/S1529-9430(02)00448-5 |
| [14] |
Ikegami S, Takahashi J, Misawa H, et al. Spinal cord MRI signal changes at 1 year after cervical decompression surgery is useful for predicting midterm clinical outcome: an observational study using propensity scores[J]. Spine J, 2018, 18(5): 755-761. DOI:10.1016/j.spinee.2017.09.004 |
| [15] |
Mazaki T, Ito Y, Sugimoto Y, et al. Does laminoplasty really improve neurological status in patients with cervical spinal cord injury without bone and disc injury? A prospective study about neurological recovery and early complications[J]. Arch Orthop Trauma Surg, 2013, 133(10): 1401-1405. DOI:10.1007/s00402-013-1810-x |
| [16] |
孙宇, 蔡钦林, 王立舜, 等. 无骨折脱位型颈脊髓损伤外科治疗随诊观察[J]. 中国脊柱脊髓杂志, 2002, 12(2): 90-92. |
| [17] |
Fehlings MG, Rabin D, Sears W, et al. Current practice in the timing of surgical intervention in spinal cord injury[J]. Spine(Phila Pa 1976), 2010, 35(21 Suppl): S166-S173. |
| [18] |
王建元, 刘华, 盛伟斌. SLIC评分在下颈椎损伤术式选择中的应用价值[J]. 中国脊柱脊髓杂志, 2016, 26(5): 415-420. DOI:10.3969/j.issn.1004-406X.2016.05.06 |
| [19] |
Hirai T, Yoshii T, Sakai K, et al. Long-term results of a prospective study of anterior decompression with fusion and posterior decompression with laminoplasty for treatment of cervical spondylotic myelopathy[J]. J Orthop Sci, 2018, 23(1): 32-38. DOI:10.1016/j.jos.2017.07.012 |
| [20] |
Liu X, Min S, Zhang H, et al. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis[J]. Eur Spine J, 2014, 23(2): 362-372. DOI:10.1007/s00586-013-3043-7 |
| [21] |
Joaquim AF, Murar J, Savage JW, et al. Dysphagia after anterior cervical spine surgery: a systematic review of potential preventative measures[J]. Spine J, 2014, 14(9): 2246-2260. DOI:10.1016/j.spinee.2014.03.030 |
| [22] |
王建杰, 曾至立, 朱睿, 等. 前路减压与稳定性重建对颈椎过伸性损伤的临床疗效[J]. 中华医学杂志, 2018, 98(47): 3858-3863. DOI:10.3760/cma.j.issn.0376-2491.2018.47.009 |
| [23] |
Daniels AH, Riew KD, Yoo JU, et al. Adverse events associated with anterior cervical spine surgery[J]. J Am Acad Orthop Surg, 2008, 16(12): 729-738. DOI:10.5435/00124635-200812000-00005 |
| [24] |
Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament[J]. Clin Orthop Relat Res, 1999(359): 35-48. |
| [25] |
Krappinger D, Lindtner RA, Zegg MJ, et al. Spondylotic traumatic central cord syndrome: a hidden discoligamentous injury?[J]. Eur Spine J, 2019, 28(2): 434-441. DOI:10.1007/s00586-018-5796-5 |
| [26] |
Chen Y, Chen D, Wang X, et al. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique[J]. Arch Orthop Trauma Surg, 2013, 133(2): 171-177. DOI:10.1007/s00402-012-1658-5 |
 2024, Vol.22
2024, Vol.22  Issue(2): 117-122
Issue(2): 117-122


