跳跃型颈椎椎间盘突出症是2个非连续节段的颈椎椎间盘退变的病理过程,其特点是突出的髓核和相应破裂的纤维环突向椎管内致使神经根或脊髓受压而引起相应的临床症状或体征,而上、下2个病变椎间盘之间可见1个或多个正常椎间盘结构。传统的颈前路减压植骨融合术是治疗多节段颈椎椎间盘突出症的经典术式,但融合术后颈椎应力重新分布、邻近节段运动过度,增加邻椎病的发生率,也可能牺牲中间正常椎间盘结构。近年来,人工颈椎椎间盘置换术(ACDR)已经用于治疗有症状的单节段和多节段颈椎椎间盘退行性疾病,并且取得了满意的临床效果[1-4]。ACDR在彻底减压的同时能维持椎间隙高度,保留置换节段的运动功能,并且能降低邻近椎间盘内的应力,理论上可减少邻椎病的发生[5-7]。笔者采用ACDR治疗跳跃型颈椎椎间盘突出症29例,现报告如下。
1 资料与方法 1.1 一般资料2008年1月—2015年2月,29例跳跃型颈椎椎间盘突出症患者在本院接受ACDR治疗。其中男14例、女15例,平均年龄45.8岁(37 ~ 54岁)。手术节段:C3/C4和C5/C6 20例,C4/C5和C6/C7 7例,C3/C4和C6/C7 1例,C2/C3和C5/C6 1例。术前影像学检查包括颈椎正侧位和过伸过屈位X线片、CT三维重建和颈椎MRI。所有患者均满足颈人工椎间盘置换术的条件。纳入标准:① 18 ~ 65岁的骨骼发育成熟的个体;② 典型神经根或者脊髓受压的症状和体征,且被CT、MRI等影像学证实受压主要以椎间盘突出软性压迫为主;③ C2~7 2个非连续节段发生病变;④ >6周非手术治疗无效。排除标准:1个或者>2个节段的病变或者是2个连续节段的病变,系统性感染,颈椎曾受过严重外伤,颈椎曾接受过手术治疗,严重的小关节疾病,颈椎不稳,颈椎畸形,骨质疏松,糖尿病或其他代谢疾病,颈椎肿瘤等。
1.2 手术方法手术均由同一位高年资医师实施。全麻下患者取仰卧位固定,保持颈椎中立位并轻度后伸。常规颈前入路显露颈椎前部。小心剥离置换节段的椎前筋膜和前纵韧带,用尖刀和刮匙切除病变椎间盘、软骨终板、椎体前缘骨质。显露部位不超过上、下椎体中点,中间跳跃节段完整保留椎前结构,不予处理。用磨钻及大小合适的骨锉打磨终板,选择大小合适的型号试模确定假体的大小。在C形臂X线机透视下植入相应型号Prestige-LP假体(MedtronicSofamor Danek,美国),位置满意后,仔细止血;同法对另一病变椎间盘实施置换手术。用大量生理盐水冲洗椎间隙及整个手术野,缝合关闭椎前筋膜、皮下脂肪组织及皮肤,伤口内放置血浆引流管1根。
1.3 评价指标术前、术后1周、术后3个月、术后6个月、术后12个月以及末次随访时,采用生活质量量表(SF-36,心理评分量表和躯体评分量表)[8]、颈部疼痛视觉模拟量表(VAS)[9]、日本骨科学会(JOA)评分[10]、颈椎功能障碍指数(NDI)[11]评价患者心理和躯体健康情况、颈部和上肢的疼痛程度、神经系统的恢复情况及颈椎功能。
应用颈椎正侧位及功能位X线片测量颈椎曲度、C2~7活动度(ROM)、跳跃节段椎间角度、置换节段及跳跃节段ROM、置换节段及跳跃节段的椎间隙高度。所有测量工作采用ACDSee Canvas 12软件完成。颈椎曲度:用Cobb角测量方法,即在侧位X线片上沿C2颈椎下缘和C7颈椎下缘各画一直线,测量此二直线所成角度(前凸为正,后凸为负)。根据Kim等[12]提出的方法评价颈椎曲度:颈椎生理曲度理想(Cobb角≥ 5°);颈椎曲度消失(0° ≤Cobb角<5°);颈椎后凸畸形(Cobb角<0°)。在侧位X线片上沿上位椎体下缘和下位椎体上缘各画一条直线,测量此二直线所成角度(前凸为正,后凸为负)即为跳跃节段椎间角度;在动力位X线片上沿C2和C7颈椎下缘各画一直线,测量此二直线所成角度,过伸与过屈位X线片上两角度之差即为C2~7 ROM;在动力位X线片上沿目标椎间盘上位椎体上缘和下位椎体下缘各画一直线,测量此二直线所成角,过伸与过屈位X线片上两角度之差即为置换节段和跳跃节段ROM。椎间隙高度为侧位X线片上目标椎间隙上下终板中点间距离。
颈椎影像学改变根据Kim等[12]采用的评价方法评定:新生前缘骨赘或者原有骨赘增大;原有椎间隙塌陷程度增加或者出现新的椎间隙高度下降(与术前相比超过30%);前纵韧带钙化、异位骨化的评定根据McAfee等[13]提出的分级方法。
1.4 统计学处理采用SPSS 19.0软件对数据进行统计学分析,测量所得数据用x±s表示,置换前后的SF-36评分、JOA评分、NDI、VAS评分、椎间高度、颈椎曲度、椎间角度以及颈椎整体和节段ROM采用配对t检验和秩和检验进行统计学分析,以P<0.05为差异有统计学意义。
2 结果 2.1 临床疗效29例患者术后平均随访25.1个月(6~82个月),其中22例患者随访>24个月,4例患者随访>48个月。术前、术后各随访点SF-36评分、JOA评分、VAS评分和NDI结果见表 1。各随访点SF-36躯体和心理评分、JOA评分均较术前明显提高,差异具有统计学意义(P<0.05);各随访点VAS评分和NDI均较术前明显降低,差异具有统计学意义(P<0.05)。
|
|
表 1 统计数据 Table 1 Statistical data |
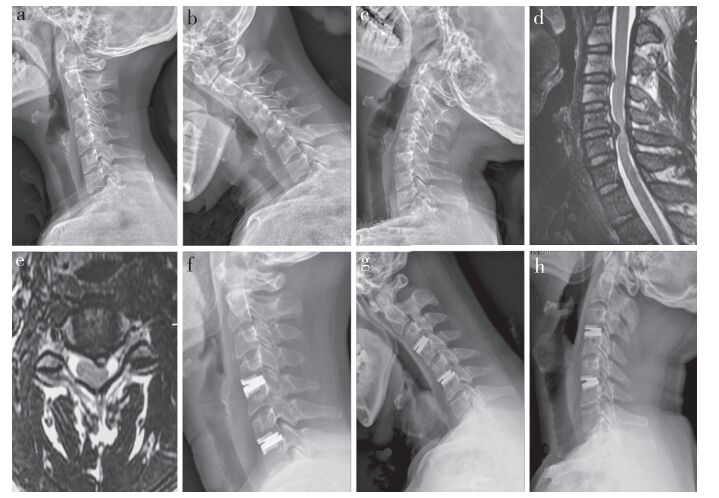
典型病例影像学资料见图 1。所有患者颈椎曲度在整个随访期间基本维持在同一水平:21例术前颈椎生理曲度理想(Cobb角≥ 5°)的患者,术后仍保持理想的生理曲度;6例颈椎曲度消失(0° ≤Cobb角<5°)的患者中,4例术后颈椎曲度未纠正,2例术后颈椎曲度部分恢复;2例术前颈椎后凸畸形(Cobb角<0°)的患者,1例术后颈椎生理曲度得到部分恢复,1例术后颈椎仍后凸畸形。
|
a:术前侧位X线片b:术前过屈位X线片c:术前过伸位X线片d:术前矢状位MRI e:术前C3/C4横断面MRI f:术后24个月侧位X线片g:术后24个月过屈位X线片h:术后24个月过伸位X线片 a: Preoperative lateral roentogenograph b: Preoperative hyperflexion roentogenograph c: Preoperative hyperextension roentogenographd: Preoperative sagittal MRI e: Preoperative transverse MRI of C3/C4 f: Lateral roentogenograph at postoperative 24 months g: Hyperflexionroentogenograph at postoperative 24 months h: Hyperextension roentogenograph at postoperative 24 months 图 1 典型病例影像学资料 Figure 1 Imaging data of a typical case |
跳跃节段椎间角度在整个随访期间维持在同一水平(表 1)。C2~7 ROM在术后1周明显减少,与术前相比差异具有统计学意义(P<0.05);术后3个月逐渐恢复,至末次随访时与术前相比差异无统计学意义(P > 0.05,表 1)。上、下位手术节段ROM在术后1周明显减少,与术前相比差异具有统计学意义(P<0.05);术后3个月逐渐恢复,至末次随访时与术前相比差异无统计学意义(P > 0.05,表 1)。跳跃节段ROM在术后1周明显减少,与术前相比差异具有统计学意义(P<0.05);术后3个月时明显增加,与术前相比差异具有统计学意义(P<0.05);术后3个月后逐渐下降,至末次随访时接近术前水平,差异无统计学意义(P>0.05,表 1)。
上、下位手术节段椎间高度在术后1周明显增加,与术前相比差异具有统计学意义(P<0.05,表 1);3个月之后各随访点无明显变化,椎间高度有效维持。跳跃节段椎间高度在各随访点与术前相比差异均无统计学意义(P>0.05,表 1)。
2.3 术后并发症置换术后3例患者出现咽部疼痛和吞咽困难症状,经非手术治疗1周后症状缓解。其余26例患者均未出现声嘶、吞咽困难、血肿、脑脊液漏等并发症。29例患者术后随访中未见新生前缘骨赘或者原有骨赘增大,椎间隙塌陷、前纵韧带钙化等影像学改变。也未发现假体下沉、脱出,置换关节异位骨化或自发性融合等并发症,随访期间均无再次手术。
3 讨论多节段颈椎椎间盘突出症的外科治疗以往以颈前路椎间盘切除融合术(ACDF)为主,长期临床效果确切,安全性较高。但是ACDF术后不可避免地会造成患者手术节段ROM消失,导致邻近节段椎间压力增加以及邻近节段ROM增加,对颈椎力学环境干扰大,这可能是产生邻椎病的原因[14]。也有医师会选择3个节段的颈椎次全切除融合术(ACCF),而不是单独对病变节段分别进行治疗,原因可能是担心中间正常节段受到两端融合节段更大的压力而加速退变[15-16],但是这种手术方式牺牲了中间正常椎间盘的结构及功能。此外,也有采用其他手术方式治疗跳跃型颈椎椎间盘突出症的报道。Wang等[17]报道用自锁型PEEK椎间融合器对16例跳跃型颈椎椎间盘退行性变患者的病变节段各自进行融合治疗;Kan等[18]报道了对32例跳跃型颈椎椎间盘退行性变患者行ACDF并ACCF治疗。以上术式理论上使中间正常节段承受了来自上、下两端的异常应力而更容易发生退变,同时,有学者报道融合节段的多少影响着邻近椎间盘的退变程度,融合的椎体越多,邻近椎间盘的退变越明显[19-20]。另一方面,这些采用融合技术治疗的颈椎椎间盘突出症患者中有很多满足椎间盘置换的纳入标准远高于需要融合的条件。因此,为了尽可能维持颈椎结构和功能并且减少或延缓邻椎病的发生,本组尝试用ACDR治疗跳跃型颈椎椎间盘突出症。
ACDR的适应证主要是脊髓型和神经根型颈椎椎间盘突出症,而对跳跃型颈椎椎间盘突出症患者的纳入标准更为严苛,要求以椎间盘退行性变、突出等软性压迫为主,病变节段没有明显的不稳,无明显的局部或者整体的颈椎后凸,不伴有明显的骨性椎管狭窄等。席焱海等[21]也认为骨赘明显、椎间隙高度丢失、小关节丢失的非连续多节段颈椎病不作为ACDR的适应证。
多节段ACDR已经在临床上取得了较为满意的效果。Kim等[12]对105例颈椎椎间盘退行性变患者进行了术后19个月的随访,其中ACDR治疗51例,单节段39例,双节段12例;ACDF治疗54例,单节段26例,双节段28例。两组疗效差异无统计学意义,ACDR组术后颈椎局部和整体ROM均得到保持,且ACDR组发生邻近节段退变率(17.64%)低于ACDF组(40.74%)。Fay等[22]对77例双节段颈椎椎间盘病变患者进行了3年随访,认为双节段ACDR与融合手术效果相当,但ACDR患者能够有效保留颈椎运动功能。Davis等[1]报道的4年随机对照研究中,225例患者采用Mobi-C行ACDR,105例行ACDF。相比ACDF组,ACDR组术后NDI等指标改善更明显,二次手术发生率也更低(4.0% vs.15.2%)。此外,多节段ACDR也表现出优于单节段置换的优势。Pimenta等[23]报道了一项采用PCM行ACDR治疗的颈椎椎间盘突出症前瞻性队列研究,其中双节段置换69例,单节段置换71例,发现术后多节段组和单节段组的NDI下降率分别为52.6%和37.6%,多节段组的症状改善较单节段组更为显著。由此可见,在治疗多节段颈椎椎间盘突出症的领域,ACDR可能较融合手术具有更大的优势。
本研究使用Prestige-LP假体[24]分别对病变节段行ACDR,保留中间正常节段的结构和功能。采用选择性椎间隙减压,手术操作仅在病变椎间盘上下椎体的1/2内,不涉及中间正常椎间隙,以保留置换节段及邻近节段的高度和ROM,减少应力重新分布。结果发现,患者症状改善明显,末次随访SF-36评分、JOA评分、VAS评分和NDI仍保持良好结果,临床效果显著,这可能与术中彻底减压和术后疼痛逐渐解除、颈椎运动功能逐渐恢复有关,与以往报道的研究结果一致[12, 22, 25-31]。采用Prestige-LP行ACDR治疗跳跃节段颈椎椎间盘突出症术后颈椎序列与术前基本一致,没有明显纠正颈椎曲度的作用,国外也有相似报道[5, 32-33]。同时,本研究在末次随访中发现ACDR术后能够维持置换节段椎间隙高度,跳跃节段的椎间隙高度在各随访点没有明显变化,提示置换术后对中间跳跃节段影响不大。有趣的是,跳跃节段术后3个月ROM较术前增加约3.32°,差异具有统计学意义(P<0.05),在以后随访中ROM逐渐下降并接近术前水平。分析可能是术后3个月内颈托保护引起颈背部肌肉萎缩、关节僵直或疼痛和心理紧张因素导致置换节段活动受限,而跳跃节段及邻近节段等正常椎间盘代偿活动所致;3个月以后完全脱离颈托后,置换节段运动功能逐渐恢复,跳跃节段代偿作用逐渐减小。
术后随访中没有发现跳跃节段有影像学上的退行性改变。因为本组资料没有ACDF作为对照组,于是参考了国内外已发表的行跳跃融合手术治疗跳跃型颈椎椎间盘退行性病变的文献。Wang等[17]报道了16例用PEEK椎间融合器对跳跃型颈椎椎间盘退行性变患者的病变节段各自进行融合治疗,在2年随访中发现6.25%的患者在跳跃节段出现了邻椎病。Bisson等[34]报道了17例用2块前路钢板对跳跃型颈椎椎间盘退行性变患者的病变节段分别进行融合治疗,在平均26个月的随访中发现跳跃节段的邻近节段退变发生率为50%。Shi等[35]报道了17例用Zero-P椎间融合器对跳跃型颈椎椎间盘退行性变患者的病变节段分别进行融合治疗,在平均24个月的随访中发现20%的患者跳跃节段发生影像学的改变。Kan等[18]报道了用ACDF并ACCF手术治疗32例跳跃型颈椎椎间盘退行性变患者的3年随访结果,其中22.92%(22/96)的邻近节段发生了退变,63.63%(14/22)发生在跳跃节段。与上述研究结果相比,本研究中邻近节段退变发生率更低,对中间跳跃节段的力学环境改变少,理论上对该节段有保护意义。
综上所述,在本研究中,经术后平均25.1个月的随访,患者疗效满意,并发症少,较好保留了置换节段及颈椎整体运动学特性,并完整保留了跳跃节段的结构和功能。根据本研究的随访结果,认为采用Prestige-LP行ACDR是一种安全有效的治疗跳跃型颈椎椎间盘突出症的手术方案。本研究的不足之处:① 是一项回顾性研究,缺乏ACDF对照组,证据级别低;② 样本量较少,随访时间较短。未来仍需更大规模、长期、前瞻性的随机对照研究来验证ACDR治疗跳跃型颈椎椎间盘突出症的安全性和有效性。
| [1] | Davis RJ, Nunley PD, Kim KD, et al. Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion:a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results[J]. J Neurosurg Spine, 2015, 22(1): 15–25. DOI:10.3171/2014.7.SPINE13953 |
| [2] | Loumeau TP, Darden BV, Kesman TJ, et al. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease(SCDD) following ProDisc-C total disc arthroplasty(TDA) versus anterior cervical discectomy and fusion(ACDF)[J]. Eur Spine J, 2016, 25(7): 2263–2270. DOI:10.1007/s00586-016-4431-6 |
| [3] | Lei T, Liu Y, Wang H, et al. Clinical and radiological analysis of Bryan cervical disc arthroplasty:eight-year follow-up results compared with anterior cervical discectomy and fusion[J]. Int Orthop, 2016, 40(6): 1197–1203. DOI:10.1007/s00264-015-3098-7 |
| [4] | 丁琛, 刘浩, 胡韬, 等. 双节段Bryan人工颈椎椎间盘置换联合双节段融合治疗多节段颈椎椎间盘突出症:5年随访结果[J]. 脊柱外科杂志, 2011, 9(5): 288–292. |
| [5] | Peng CW, Yue WM, Basit A, et al. Intermediate results of the Prestige LP cervical disc replacement:clinical and radiological analysis with minimum two-year follow-up[J]. Spine(Phila Pa 1976), 2011, 36(2): E105–111. DOI:10.1097/BRS.0b013e3181d76f99 |
| [6] | Chen J, Wang X, Yuan W, et al. Cervical myelopathy after cervical total disc arthroplasty:case report and literature review[J]. Spine(Phila Pa 1976), 2012, 37(10): E624–628. DOI:10.1097/BRS.0b013e3182413930 |
| [7] | 孙宇, 赵衍斌, 周非非, 等. Bryan人工椎间盘置换术对颈椎曲度影响的研究[J]. 脊柱外科杂志, 2011, 9(5): 260–262. |
| [8] | Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey(SF-36). Ⅰ. Conceptual framework and item selection[J]. Med Care, 1992, 30(6): 473–483. DOI:10.1097/00005650-199206000-00002 |
| [9] | Huskisson EC. Measurement of pain[J]. Lancet, 1974, 2(7889): 1127–1131. |
| [10] | Yonenobu K, Abumi K, Nagata K, et al. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy[J]. Spine(Phila Pa 1976), 2001, 26(17): 1890–1895. DOI:10.1097/00007632-200109010-00014 |
| [11] | Vernon H, Mior S. The Neck Disability Index:a study of reliability and validity[J]. J Manipulative Physiol Ther, 1991, 14(7): 409–415. |
| [12] | Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases[J]. Eur Spine J, 2009, 18(2): 218–231. DOI:10.1007/s00586-008-0854-z |
| [13] | McAfee PC, Cunningham BW, Devine J, et al. Classification of heterotopic ossification(HO) in artificial disk replacement[J]. J Spinal Disord Tech, 2003, 16(4): 384–389. DOI:10.1097/00024720-200308000-00010 |
| [14] | Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion[J]. Spine(Phila Pa 1976), 2002, 27(22): 2431–2434. DOI:10.1097/00007632-200211150-00003 |
| [15] | Mao N, Wu J, Zhang Y, et al. A comparison of anterior cervical corpectomy and fusion combined with artificial disc replacement and cage fusion in patients with multilevel cervical spondylotic myelopathy[J]. Spine (Phila Pa 1976), 2015, 40(16): 1277–1283. DOI:10.1097/BRS.0000000000000957 |
| [16] | Mummaneni PV, Haid RW. The future in the care of the cervical spine:interbody fusion and arthroplasty. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2004[J]. J Neurosurg Spine, 2004, 1(2): 155–159. DOI:10.3171/spi.2004.1.2.0155 |
| [17] | Wang HR, Li XL, Dong J, et al. Skip-level anterior cervical discectomy and fusion with self-locking stand-alone PEEK cages for the treatment of 2 noncontiguous levels of cervical spondylosis[J]. J Spinal Disord Tech, 2013, 26(7): E286–292. DOI:10.1097/BSD.0b013e31828679b3 |
| [18] | Kan L, Kang J, Gao R, et al. Clinical and radiological results of two hybrid reconstructive techniques in noncontiguous 3-level cervical spondylosis[J]. J Neurosurg Spine, 2014, 21(6): 944–950. DOI:10.3171/2014.8.SPINE13791 |
| [19] | Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level[J]. J Neurosurg Spine, 2007, 7(3): 336–340. DOI:10.3171/SPI-07/09/336 |
| [20] | Finn MA, Samuelson MM, Bishop F, et al. Two-level noncontiguous versus three-level anterior cervical discectomy and fusion:a biomechanical comparison[J]. Spine(Phila Pa 1976), 2011, 36(6): 448–453. DOI:10.1097/BRS.0b013e3181fd5d7c |
| [21] | 席焱海, 何海龙, 许国华, 等. 人工颈椎间盘置换在非连续型多节段颈椎病手术中的初步应用研究[J]. 脊柱外科杂志, 2009, 7(5): 304–306. |
| [22] | Fay LY, Huang WC, Tsai TY, et al. Differences between arthroplasty and anterior cervical fusion in two-level cervical degenerative disc disease[J]. Eur Spine J, 2014, 23(3): 627–634. DOI:10.1007/s00586-013-3123-8 |
| [23] | Pimenta L, McAfee PC, Cappuccino A, et al. Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes:229 consecutive PCM prostheses[J]. Spine(Phila Pa 1976), 2007, 32(12): 1337–1344. DOI:10.1097/BRS.0b013e318059af12 |
| [24] | Gornet MF, Lanman TH, Burkus JK, et al. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels:results of a prospective, multicenter randomized controlled clinical trial at 24 months[J]. J Neurosurg Spine, 2017. |
| [25] | Davis RJ, Kim KD, Hisey MS, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease:a prospective, randomized, controlled multicenter clinical trial:clinical article[J]. J Neurosurg Spine, 2013, 19(5): 532–545. DOI:10.3171/2013.6.SPINE12527 |
| [26] | Hou Y, Liu Y, Yuan W, et al. Cervical kinematics and radiological changes after Discover artificial disc replacement versus fusion[J]. Spine J, 2014, 14(6): 867–877. DOI:10.1016/j.spinee.2013.07.432 |
| [27] | Cheng L, Nie L, Zhang L, et al. Fusion versus Bryan cervical disc in two-level cervical disc disease:a prospective, randomised study[J]. Int Orthop, 2009, 33(5): 1347–1351. DOI:10.1007/s00264-008-0655-3 |
| [28] | Qizhi S, Lei S, Peijia L, et al. A comparison of Zero-Profile devices and artificial cervical disks in patients with 2 noncontiguous levels of cervical spondylosis[J]. Clin Spine Surg, 2016, 29(2): E61–66. |
| [29] | 王贝宇, 刘浩, 丁琛, 等. Bryan人工颈椎椎间盘置换术治疗颈椎病的中期临床效果及对邻近椎间盘退变的影响[J]. 脊柱外科杂志, 2011, 9(5): 273–278. |
| [30] | 丁琛, 刘浩, 胡韬, 等. Bryan人工颈椎间盘置换治疗颈椎病的中期临床随访[J]. 中国组织工程研究与临床康复, 2011, 15(17): 3047–3052. DOI:10.3969/j.issn.1673-8225.2011.17.004 |
| [31] | 尚子琨, 张英泽, 张迪, 等. 人工椎间盘置换术治疗跳跃型多节段颈椎病的中期疗效[J]. 中华骨科杂志, 2014, 34(8): 791–798. |
| [32] | Yoon DH, Yi S, Shin HC, et al. Clinical and radiological results following cervical arthroplasty[J]. Acta Neurochir(Wien), 2006, 148(9): 943–950. DOI:10.1007/s00701-006-0805-6 |
| [33] | Sasso RC, Metcalf NH, Hipp JA, et al. Sagittal alignment after Bryan cervical arthroplasty[J]. Spine (Phila Pa 1976), 2011, 36(13): 991–996. DOI:10.1097/BRS.0b013e3182076d70 |
| [34] | Bisson EF, Samuelson MM, Apfelbaum RI. Intermediate segment degeneration after noncontiguous anterior cervical fusion[J]. Acta Neurochir(Wien), 2011, 153(1): 123–128. DOI:10.1007/s00701-010-0832-1 |
| [35] | Shi S, Liu ZD, You WJ, et al. Application of a stand-alone anchored spacer in noncontiguous anterior cervical arthrodesis with radiologic analysis of the intermediate segment[J]. J Clin Neurosci, 2016, 25: 69–74. DOI:10.1016/j.jocn.2015.05.050 |
 2017, Vol.15
2017, Vol.15  Issue(4): 193-199
Issue(4): 193-199


